Abstract
Lung transplantation (LTx) can be a life-extending treatment option for patients with advanced and/or progressive fibrotic interstitial lung disease (ILD), especially idiopathic pulmonary fibrosis (IPF), fibrotic hypersensitivity pneumonitis, sarcoidosis and connective tissue disease-associated ILD. IPF is now the most common indication for LTx worldwide. Several unique features in patients with ILD can impact optimal timing of referral or listing for LTx, pre- or post-transplant risks, candidacy and post-transplant management. As the epidemiology of LTx and community practices have evolved, recent literature describes outcomes and approaches in higher-risk candidates. In this review, we discuss the unique and important clinical findings, course, monitoring and management of patients with IPF and other progressive fibrotic ILDs during pre-LTx evaluation and up to the day of transplantation; the need for co-management with clinical experts in ILD and LTx is emphasised. Some post-LTx complications are unique in these patient cohorts, which require prompt detection and appropriate management by experts in multiple disciplines familiar with telomere biology disorders and infectious, haematological, oncological and cardiac complications to enhance the likelihood of improved outcomes and survival of LTx recipients with IPF and other ILDs.
Short abstract
This review summarises the many unique and important features in patients who undergo lung transplant for interstitial lung disease that can impact pre-transplant disease progression, transplant risks, candidacy and post-transplant management https://bit.ly/2PU1FLq
Introduction
Lung transplantation (LTx) can extend and improve quality of life for patients with advanced lung disease. The International Society for Heart and Lung Transplantation (ISHLT) has reported a steady increase in worldwide transplants over the past two decades, with nearly 4500 performed in 2017 [1]. These data are estimated to capture approximately three-quarters of worldwide lung transplant activity, of which roughly 55% and 34% of total transplants have been performed in North America and Europe, respectively [2]. The distribution of diagnoses undergoing LTx has also evolved, with interstitial lung disease (ILD) surpassing COPD as the most common indication in 2007, and the percentage of total worldwide transplants for ILD having increased in 2017 to 40.5%, including 32.4% for idiopathic pulmonary fibrosis (IPF) [1]. The trend is most pronounced in North America, including the USA, where 60% of total lung transplants were performed for restrictive lung disease in 2018 [1, 3]. With the community transitioning toward a philosophy of transplanting those at highest short-term risk of death, simulations evaluating broader organ sharing and high emergency allocation systems also project increasing transplant rates among candidates with ILD [4–6].
LTx outcomes have improved for patients transplanted for ILD and other diagnoses. The ISHLT reports a median post-transplant survival of 5.2 years for patients with idiopathic interstitial pneumonia, and 6.7 years for other ILDs transplanted between 1992 and 2017, with outcomes improving in the most recent years [1]. In IPF treatment guidelines by the American Thoracic Society (ATS)/European Respiratory Society (ERS)/Japanese Respiratory Society (JRS)/Latin American Thoracic Association (ALAT), LTx receives a strong recommendation based on a 75% reduced risk of death compared to medical management alone in well-selected patients, a survival benefit that probably also extends to patients with other severe or progressive ILDs [7–11].
With a growing population of pre- and post-transplant patients with ILD, there is increasing need to fully appreciate the unique issues faced by this complex population that can impact candidacy, peri-operative risks and post-LTx management. In this article, we review the unique and important considerations in patients transplanted for IPF and other fibrotic lung diseases.
Consideration and timing of LTx in patients with ILD
Preparing for LTx in a given patient includes the separate, often overlapping phases of 1) transplant referral; 2) an evaluation period guided by the transplant centre; 3) active listing by the transplant team; and 4) concurrent management of disease progression by an experienced ILD team (figure 1). Determining the optimal timing can be challenging, and particularly in IPF, some advocate for a philosophy of broad referral for LTx as early as feasible, while others, acknowledging limitations in resources including transplant programme capacity, suggest a more selective approach [12]. International guidelines recommend that LTx be considered in patients with chronic lung disease who have a high risk of death within 2 years [13, 14], and the timing of both referral and listing for LTx incorporate current quality of life and expected survival, along with patient preferences.
FIGURE 1.
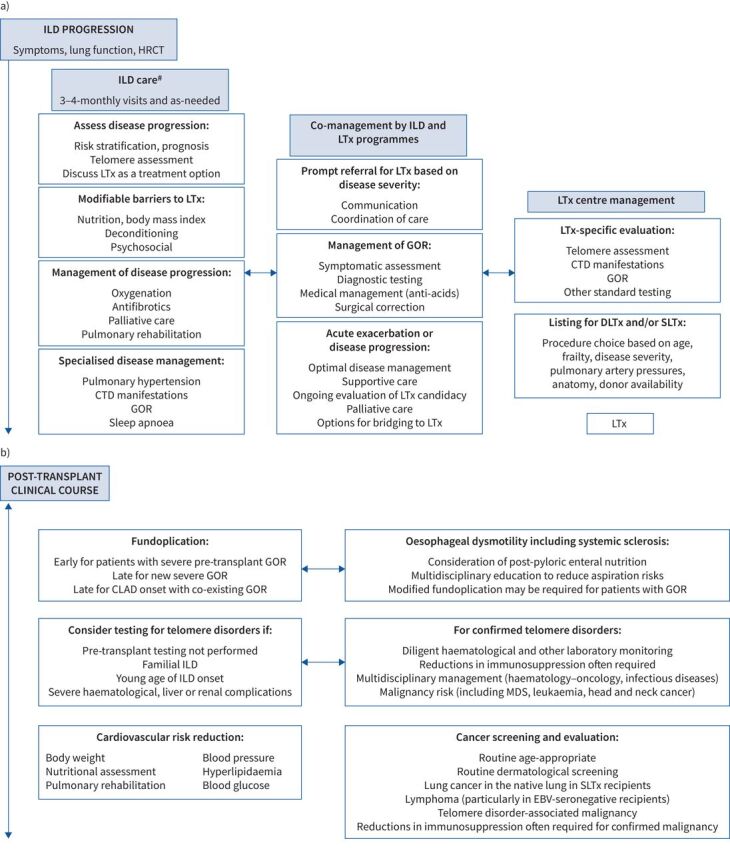
Suggested approach for management of progressive interstitial lung disease (ILD) a) before and b) after lung transplantation (LTx). HRCT: high-resolution computed tomography; CTD: connective tissue disease; GOR: gastro-oesophageal reflux; DLTx: double lung transplantation; SLTx: single lung transplantation; CLAD: chronic lung allograft dysfunction; MDS: myelodysplastic syndrome; EBV: Epstein–Barr virus. #: ILD care should preferably be undertaken by experts in ILD in an experienced centre.
IPF, the prototype ILD manifesting progressive pulmonary fibrosis carries a generally poor prognosis with median survival 2–5 years from diagnosis [13, 15–17]. However, prediction in a given individual remains challenging, considering that >20% of the overall IPF population exhibits a less aggressive disease course [18]. Moreover, the long-term effects of antifibrotics on prognosis remain unclear, with both nintedanib and pirfenidone shown to reduce the rate of forced vital capacity (FVC) decline and acute exacerbations, and post hoc pooled analyses suggesting mortality benefit [19–21]. In addition to clinical experience suggesting stabilisation with antifibrotics in a subset of patients, longer term outcomes were recently reported in a 2-year extension of the TOMORROW trial (which had compared 52 weeks of nintedanib versus placebo in IPF [22]), demonstrating mortality in only 25.9% of patients treated with full-dose nintedanib over the extension period [23].
Survival varies significantly among patients with non-IPF ILD, often exceeding that of IPF by many years, particularly in sarcoidosis, connective tissue disease (CTD)-associated nonspecific interstitial pneumonia (NSIP) and occupational ILD [24–26]. A recent French study grouped several different and specific (non-IPF) ILDs into a single entity termed progressive-fibrosing ILD, defined by ≥10% fibrosis on baseline high-resolution computed tomography (HRCT) and clinical disease progression for 2 years prior to study inclusion (by symptoms, lung function and/or HRCT) [27]. Survival was worse in unclassifiable disease or hypersensitivity pneumonitis compared to CTD-ILD, sarcoidosis or other ILDs, but was >87% at 2 years and 49.1–80.2% at 7 years in all groups, indicating survival at the time of initial assessment exceeding the usual thresholds to consider LTx. Furthermore, several recent studies have demonstrated a benefit of antifibrotics in non-IPF ILDs [28–31], suggesting that these agents may stall disease progression and delay or obviate the need for LTx in some.
In contrast, the majority of patients with IPF experience an aggressive course, and the progressive disease in some with non-IPF ILD resembles that of IPF [25, 27, 32–34]. Moreover, the unpredictability and severe consequences of ILD exacerbations should be appreciated, as should the potential for diagnostic uncertainty. Finally, certain barriers to LTx may disproportionately impact candidates with ILD, including small chest cavity in combination with short stature, as well as allosensitisation in those with CTD; although not generally considered when determining LTx referral timing, these factors do have the potential to increase waiting-list times and mortality and thus impact the optimal timing of listing [35–37].
Referral and listing guidelines generalise between forms of ILD and incorporate factors associated with worse outcomes including lower/declining pulmonary function (particularly FVC and diffusing capacity of the lung for carbon monoxide (DLCO)), higher oxygen needs, lower 6-min walk distance (6MWD), pulmonary hypertension (PH), history of pneumothorax or other respiratory hospitalisation, usual interstitial pneumonia pattern on HRCT, frailty and low performance status [13, 27, 38–44] (table 1). Response or lack of response to antifibrotics should be considered. Upcoming guidelines do not alter referral and listing recommendations in patients treated with nintedanib and pirfenidone, but acknowledge the associated challenges in determining timing of LTx [13], and more data are needed to delineate the impacts of antifibrotics on optimal timing of transplantation. Clinical models may improve prediction, but are not widely used in practice [45], and various biomarkers hold promise, but are not yet validated [46]. It should be noted that FVC decline has been shown to be a less reliable predictor in patients with combined pulmonary fibrosis and emphysema [47].
TABLE 1.
Criteria for referral and listing for lung transplantation in patients with interstitial lung disease (ILD)
| Timing of referral# | Timing of listing |
| Histopathological UIP | Hospitalisation for respiratory decline, pneumothorax or acute exacerbation |
| Radiographic probable or definite UIP pattern | Desaturation to <88% on 6MWT or >50 m decline in 6MWD over 6 months |
| FVC <80% or DLCO <40% pred | Pulmonary hypertension on right heart catheterisation or echocardiography |
| Relative decline in pulmonary function over the past 2 years: FVC ≥10% or DLCO ≥15% or FVC ≥5% with symptomatic or radiographic progression |
Absolute decline in pulmonary function over the past 6 months despite appropriate treatment: FVC >10% or DLCO >10% or FVC >5% with radiographic progression |
| Any resting or exertional oxygen requirement | |
| For inflammatory ILDs, disease progression despite treatment |
Referral or listing should be considered if meeting any one criterion. UIP: usual interstitial pneumonia; FVC: forced vital capacity; DLCO: diffusing capacity of the lung for carbon monoxide; 6MWT: 6-min walk test; 6MWD: 6-min walk distance. #: earlier referral is recommended for patients with connective tissue disease or familial idiopathic pulmonary fibrosis to address potential extrapulmonary manifestations. Reproduced and modified from [13] with permission.
Acknowledging difficulties in predicting prognosis and higher waiting-list mortality among candidates with ILD compared to other diagnoses [3], the ISHLT emphasises the most conservative strategy of early referral. However, it is important to recognise that specific referral and listing practices vary significantly by ILD and transplant programme, influenced by nation and allocation system, usual waiting times for suitable organs, programme resources, as well as patient volumes and geographic distribution.
Unique risk factors and consideration for LTx in candidates with ILD
Emphasising the importance of long-term outcomes, guidelines currently under development by the ISHLT recommend that LTx be considered only in candidates with a high (>80%) likelihood of 5-year post-transplant survival from a general medical perspective, provided there is adequate graft function [13]. Some factors including recent malignancy, life-threatening extrapulmonary organ dysfunction and severe psychosocial problems are considered “absolute contraindications” due to the excessive associated risks of poor outcome (table 2). Accounting for significant variability in handling between transplant centres, the term “relative contraindications” has been replaced by a list of characteristics associated with worse outcomes, with the updated document also commenting on the additive nature of multiple risk factors (table 2) [13]. Many are common in ILD and warrant increased attention, focused management or discussions between referring providers and transplant centres (table 3; see also the section “Management while being considered or after listing for LTx”).
TABLE 2.
Risk factors for adverse post-transplant outcomes in candidates for lung transplantation
| General | High or substantially increased risk | Absolute contraindications |
| Age 65–70 years GFR 40–60 mL·min−1·1.73 m−2 CAD including prior CABG LV ejection fraction 40–50% Peripheral vascular disease Connective tissue disease Severe GOR Oesophageal dysmotility Bone marrow dysfunction Osteoporosis BMI 30–34.9 kg·m−2 BMI 16–17 kg·m−2 Frailty Hypoalbuminaemia Poorly controlled diabetes Edible marijuana Scedosporium apiospermum infection HIV with undetectable viral load Previous thoracic surgery including pleurodesis Mechanical ventilation Re-transplantation |
Age >70 years Severe CAD requiring CABG at transplant LV ejection fraction <40% Significant cerebrovascular disease Severe oesophageal dysmotility Untreatable haematological disorders (bleeding diathesis, thrombophilia, severe bone marrow dysfunction) BMI ≥35 kg·m−2 BMI <16 kg·m−2 Limited functional status with poor rehabilitation potential Psychiatric, psychological or cognitive conditions with potential to interfere with medical adherence Unreliable support system Lack of understanding of disease and/or transplant despite teaching Mycobacterium abscessus infection Lomentospora prolificans infection Burkholderia cenocepacia or gladioli infection Hepatitis B or C infection with detectable viral load and liver fibrosis Chest wall or spinal deformity expected to cause restriction after transplant Extracorporeal life support Re-transplantation for restrictive CLAD, antibody-mediated rejection or within 1 year following initial lung transplant |
Lack of patient willingness or acceptance of transplant Malignancy with high risk of death or recurrence GFR <40 mL·min−1·1.73 m−2 unless being considered for multi-organ transplant Acute coronary syndrome within 30 days (excluding demand ischaemia) Stroke within 30 days Liver cirrhosis with portal hypertension or synthetic dysfunction unless being considered for multi-organ transplant Acute liver failure Acute renal failure with rising creatinine or on dialysis and low likelihood of recovery Active extrapulmonary infection including septic shock Active tuberculosis infection HIV infection with detectable viral load Severely limited functional status with poor rehabilitation potential Progressive cognitive impairment Repeated episodes of nonadherence without evidence of improvement Active substance use or dependence including current tobacco use, vaping, marijuana smoking or intravenous drug use Other severe uncontrolled medical condition expected to limit survival after transplant |
GFR: glomerular filtration rate; CAD: coronary artery disease; CABG: coronary artery bypass grafting; LV: left ventricular; GOR: gastro-oesophageal reflux; BMI: body mass index; CLAD: chronic lung allograft dysfunction. Reproduced and modified from [13] with permission.
TABLE 3.
Common risk factors for adverse post-lung transplant outcomes in candidates with interstitial lung disease
| Advanced age |
| Overweight status |
| Telomere biology disorders |
| Prior thoracic surgery |
| Limited functional status, deconditioning, frailty |
| Gastro-oesophageal reflux |
| High-risk atherosclerotic disease |
| Connective tissue disease manifestations |
| Corticosteroids, other immunosuppressants |
| Acute exacerbations |
| Active mechanical ventilation |
Advanced age in IPF
Age remains a controversial selection criterion for LTx. Based on the ethical principles of justice and utility, the international transplant community has generally expressed a preference to prioritise organ allocation to younger patients [13, 48], and this may be particularly important in programmes and nations with the most pronounced donor shortages. Published literature reports worse survival in recipients older than 65–70 years [1, 49, 50], and elderly recipients appear to be at greater risk of malignancy, vascular events, drug toxicity and cognitive decline [51, 52]. Previous guidelines classified age >65 years with low physiological reserve as a relative contraindication to LTx, commenting also that patients aged >75 years are unlikely to be candidates [14].
Recent literature is more encouraging in the elderly, particularly pertaining to short-term LTx outcomes, where 1-year post-transplant survival appears comparable between recipients aged 70–79 years versus 60–69 years [50]. With an ageing population and increasing experience, the proportion of lung transplants performed in elderly patients is increasing. Worldwide data show an increase in the proportion of LTx recipients aged >65 years from 2.6% in 2004 to 17% in 2016 [51]. The trend appears most pronounced in the USA, where >30% of candidates on the waiting list are now aged >65 years [3]. This population largely comprises patients with IPF, and 2016 data show that >40% of IPF transplants are now in patients aged >65 years [51].
More data are needed to better risk-stratify older patients with IPF undergoing transplant. This is especially important in the antifibrotic era, where slowing of disease progression may delay the need for LTx in a subset of patients, and in turn lead to encroachment upon programmatic age limits for transplant. A recent study of 5815 patients aged >65 years (70% with restrictive lung disease) demonstrated that increasing age strata, creatinine, bilirubin, hospitalisation at time of transplant, and pre-transplant steroid use were all associated with increased mortality [53]. Other literature focuses on differentiating biological from chronological age, incorporating sarcopenia and frailty, each of which has been independently associated with worse outcomes [54]. Ultimately, no absolute upper age limit for LTx is endorsed by the ISHLT, and candidacy in elderly patients remains a centre-specific decision [13].
Overweight status
Biological factors, reduced activity and/or corticosteroids lead to weight gain in many with advanced ILD. One study from the USA of 5978 LTx recipients showed that 67% of the 1246 transplanted patients with ILD were overweight (body mass index (BMI) ≥25 kg·m−2) prior to LTx. Compared to normal-weight recipients, those who were overweight or obese had a 15% or 22% higher multivariable-adjusted rate of post-transplant death, respectively [55]. In addition to improving pre-transplant symptoms, weight loss before LTx in overweight candidates has been associated with dose–response improvements in post-transplant survival [56], and many transplant programmes utilise BMI thresholds of 30–35 kg·m−2 as criteria for active listing.
CTD-associated ILD
LTx has been used for advanced lung disease in rheumatoid arthritis, mixed CTD, systemic sclerosis, Sjogren syndrome, systemic lupus erythematosus, polymyositis/dermatomyositis/antisynthetase syndrome and pulmonary vasculitis. Although data are limited in CTD-ILD, several cohort studies report post-transplant survival similar to IPF, with no differences in primary graft dysfunction or rejection rates [57–60]. Functional status has been shown to improve [58], and recurrent or progressive nonpulmonary disease after LTx appears to be rare [57, 59, 61]. Even in systemic sclerosis, where some may be considered ineligible for LTx due to aspiration risks, several studies show post-transplant survival similar to IPF without increased risk of chronic lung allograft dysfunction (CLAD) [62–66].
It should be recognised that available studies on LTx for CTD are retrospective and limited by selection bias. In this context, the ISHLT considers CTD to be a risk factor for poorer outcomes and recommends screening for extrapulmonary disease in collaboration with rheumatology when possible [13]. Although post-transplantation immunosuppression generally renders extrapulmonary inflammatory disease quiescent, efforts should be made to control pre-transplant disease at the lowest levels possible to reduce peri-operative infectious risks, while also ensuring that any nonreversible disease does not pose excessive threat to post-transplant outcomes or rehabilitation potential. Systemic sclerosis with severe oesophageal dysmotility may be considered a contraindication at some centres; assessment of swallowing and oesophageal function is crucial, and patients should also undergo evaluation for skin thickening, digital ulceration, renal insufficiency and cardiomyopathy. For inflammatory myopathies, comprehensive cancer screening is required [13, 60]. Comprehensive ISHLT guidelines on LTx for CTD have recently been published [13].
Considerations in other ILDs including sarcoidosis
LTx is an option for several other ILDs including Langerhans cell histiocytosis [67], occupational ILD including silicosis [68, 69], pleuroparenchymal fibroelastosis (PPFE) [70], chronic hypersensitivity pneumonitis [71] and sarcoidosis. Sarcoidosis is the most common of these less-frequent indications for LTx, accounting for 2.4% of worldwide transplants between 1995 and 2018 [1]. LTx candidacy in sarcoidosis is generally approached similarly to other ILDs, with the addition of careful pre-transplant screening for conductive and/or infiltrative cardiac disease based on the clinical scenario [72]. Patients with advanced cardiac dysfunction may require heart–lung transplantation, with sarcoidosis accounting for 1.9% of worldwide heart–lung transplants between 1998 and 2018 [1]. Transplant for sarcoidosis appear to yield similar outcomes compared to the general transplant population [72, 73]. One study analysed 695 patients with sarcoidosis transplanted between 1987 and 2012 and found no difference in survival or bronchiolitis obliterans syndrome (BOS) compared to nonsarcoidosis controls, with the sarcoidosis cohort having a median survival of 63.1 months and a 10-year survival of ∼30% [74]. Sarcoidosis does recur in the allograft in up to 35% of lung transplants, but rarely impacts clinical outcomes (see also the section “Outcomes and considerations after LTx for ILD”) [75].
Although data are limited, other ILDs have also been shown to have similar, if not better, survival after LTx compared to IPF and other control groups [71]. Evaluation of LTx candidacy is also similar, although surgical complexity can be increased in those with dense pleural adhesions. For example, one study compared outcomes of LTx for occupational lung disease versus other diagnoses, and demonstrated similar long-term survival, but a higher need for cardiopulmonary bypass and delayed chest closure in the occupational lung disease cohort [69]. PPFE, presenting either as its own entity or co-existing with other patterns of ILD, can be particularly challenging operatively, with dense adhesions often leading to thoracic contraction and increased bleeding risk [76]. LTx for PPFE or other disorders associated with dense pleural adhesions should be performed only in experienced centres [69, 76].
Telomere disorders (pre-transplant considerations)
Chromosomal telomeres protect against loss of genetic information during normal cell division. Critical shortening, often associated with specific mutations in telomere maintenance (including telomerase (TERC/TERT)), can lead to cell-cycle arrest with associated bone marrow failure and cancer predisposition [77]. A tendency toward both haematological and other forms of cancer, including of the head and neck, is reported [78]. In addition, telomere disorders have been implicated in ILD pathogenesis. A leukocyte telomere length <10th percentile is found in up to 25% of patients with sporadic and 37% of familial IPF [79], with disorders also recognised in several other forms of ILD [80]. Pre-transplant, telomere shortening is associated with earlier age of presentation and a progressive phenotype [81], and predicts poor response to immunosuppressants in IPF [82].
Reduced telomere length has been linked with worse post-transplant outcomes. Among 86 patients transplanted for ILD, one study demonstrated that pre-transplant telomere length <10th percentile was independently associated with worse survival (hazard ratio 10.9, 95% CI 2.7–44.8; p=0.001) and higher risks of primary graft dysfunction and CLAD [83]. Haematological and several other post-transplant medical complications are also more common in this cohort [81, 84–86]. With these associations in mind, haematological abnormalities in the context of telomere disorders are now recognised by the ISHLT as a risk factor for poor LTx outcomes [13]. Testing for telomere length and the associated mutations in candidates with ILD is now performed in some centres and may be particularly useful in early-onset or familial ILD. More data are needed to determine whether and how best to integrate testing into the routine pre-transplant evaluation, but it may assist in determining pre-transplant prognosis, risk-stratifying candidates, and predicting post-transplant complications (see also the section “Outcomes and considerations after LTx for ILD”).
Management while being considered or after listing for LTx
In addition to determining timing of LTx referral (and listing), management of progressive ILD should take place in an experienced ILD centre and requires a comprehensive approach aimed at 1) slowing disease progression and improving symptoms; 2) mitigating risks to improve the likelihood of successful LTx; and 3) optimising candidacy for LTx (figure 1). If the ILD expert is different from the lung transplant pulmonologist, the teams must work in a concerted manner to optimise care and communication (figure 1). Coordination of care may be facilitated if the ILD and transplant pulmonologists are at the same centre, but this may not be required, assuming frequent and close communication can be achieved.
Many recommendations from the ATS/ERS/JRS/ALAT 2011 and 2015 IPF management guidelines apply broadly to advanced ILD, including regular assessment of oxygenation, consideration of antifibrotics, and pulmonary rehabilitation [10, 11]. Palliative care should be considered and advance directives addressed while the candidate is an outpatient, and these steps should not be construed as mutually exclusive from treatment-oriented care including LTx [87, 88]. Psychosocial support may be valuable, and caregiver and financial planning are required prior to LTx to improve the likelihood of successful outcome.
Finally, evaluation for and management of common comorbidities can be beneficial, including obstructive sleep apnoea, coronary artery disease (CAD), gastro-oesophageal reflux (GOR), venous thromboembolism and associated PH [89, 90]. For patients with PH, sildenafil, including in a placebo-controlled trial of 274 IPF patients with DLCO <35%, has been shown not to improve dyspnoea or 6MWD [91], and received a conditional recommendation against their use in the 2015 guidelines [11]. However, PH can guide transplant timing and appears to be common in this population, with one study showing right ventricular dysfunction in >40% of those with IPF and DLCO <35% [91], and another showing pre-transplant mean pulmonary artery pressure >40 mmHg in nearly 20% of patients with restrictive lung disease who underwent double LTx (DLTx) [92]. Functional 6MWD benefits have been demonstrated with sildenafil in IPF patients with right ventricular dysfunction [93]. From a transplant perspective, PH is associated with increased risk of primary graft dysfunction and early post-operative mortality after LTx and its presence impacts surgical planning [94, 95], use of mechanical circulatory support and anaesthetic management, although it is unknown how pre-transplant treatment impacts these considerations. Therefore, evaluation for PH should be considered in progressive ILD, particularly in patients with suggestive signs exceeding those expected from their lung disease alone, or in those with systemic sclerosis or other CTDs in which an overlapping component of vasodilator-responsive (World Health Organization group 1) PH is more likely [96, 97].
Relative risks associated with ILD pharmacotherapies
Specific treatments may impact peri-operative risks in ILD patients approaching LTx. Chronic, high-dose corticosteroids in particular may increase wound healing complications and risk of anastomotic dehiscence, and one study demonstrated increased mortality among 62 patients (38% with ILD) treated with pre-transplant prednisone doses >0.42 mg·kg−1·day−1 [98]. Other data suggest that doses <40 mg or 0.3 mg·kg−1·day−1 are probably safe [99]. Based on potential risks, many LTx programmes consider maintenance prednisone-equivalent doses >20 mg·day−1 to be a contraindication (excluding augmented doses for acute exacerbations), and discussions between ILD and transplant programmes on specific corticosteroid policies are necessary. There are no data on the impact of other immunomodulating agents on LTx outcomes, but in general it is best to limit immunosuppressants for ILD to the lowest effective doses while a patient is listed for transplant.
Lastly, despite early attention, recent studies have not demonstrated differences in survival, anastomotic dehiscence or other complications among ILD patients treated with pre-transplant pirfenidone or nintedanib [100, 101]. The use of antifibrotics leading up to the day of LTx is not considered a contraindication.
Proactive management of obesity and deconditioning
As described earlier, overweight status is common in patients with ILD approaching LTx. Nutritional counselling and appropriate weight loss can increase the likelihood of successful LTx [56] and improve candidacy, while also potentially improving pre-transplant symptoms. Deconditioning, reduced functional status, frailty and sarcopenia have also been shown to impact pre-transplant trajectory and post-transplant outcomes [102–105]. All appear to be common in advanced ILD, with frailty demonstrated in ∼30% of candidates with restrictive lung disease [103, 106, 107], and small studies showing reduced muscle mass by imaging criteria in 20–40% of candidates [105, 108]. Frailty and impaired functional status are considered risk factors for poor outcomes with LTx [13], and patients with advanced ILD warrant a thorough assessment of conditioning and functional status. Pulmonary rehabilitation has been associated with improved (pre-transplant) symptoms, quality of life and 6MWD, along with more favourable early post-transplant outcomes [13, 109, 110]. It should be considered in all patients with advanced ILD and may be required for LTx.
Anti-reflux surgery for abnormal GOR
GOR has been demonstrated in up to 90% of people with IPF and has been implicated in ILD pathogenesis [111–113]. The impact of GOR may be amplified in those with co-existing gastrointestinal dysmotility, most notably in systemic sclerosis [114, 115]. In the WRAP-IPF study, 58 patients with IPF and FVC >50% predicted (mean 76.5% pred) were randomised to laparoscopic fundoplication versus medical management alone. There was no difference in FVC change over 48 weeks, but the surgical cohort had numerically fewer acute exacerbations, respiratory hospitalisations and deaths, without major complications [116].
Reflux and oesophageal motility evaluation is generally required by transplant programmes during evaluation based on associations between GOR and oesophageal dysfunction and post-transplant early allograft injury, infection, acute rejection and CLAD [117–119]. Pre- or early post-transplant fundoplication has been shown to mitigate these risks [120, 121]. Although pre-transplant surgery probably carries increased risks compared to those with less severe ILD, it has been shown to be safe in well-selected patients approaching LTx, including in one cohort with mean FVC 50% pred [120]. Surgical management may serve several purposes, including slowing pre-transplant disease progression, fulfilling candidacy requirements and improving post-transplant outcomes, although more data are needed, especially in advanced ILD. It should be noted that patients with co-existing GOR and oesophageal dysmotility may require modified (Toupet) fundoplication. Ultimately, surgical decisions are generally made on a case-by-case basis in multidisciplinary fashion.
Pre-transplant acute exacerbations
Most literature on acute ILD exacerbations pertains to IPF (AE-IPF), defined as acute (typically less than 1 month's duration) respiratory deterioration with widespread alveolar abnormality, and exclusion of alternative diagnoses including pulmonary oedema [122]. The prognosis of AE-IPF is poor, with in-hospital mortality nearly 50% and as high as 90% in those requiring mechanical ventilation [10], along with a median survival following AE-IPF of only 3–4 months [122]. Corticosteroids may be beneficial in some cases including non-IPF ILD, but supportive evidence in AE-IPF is limited, and without other effective treatments management is largely supportive.
For listed patients, data from the USA show that waiting-list mortality is highest for candidates with restrictive lung disease and with lung allocation scores (LAS) ≥50, at 29.7 and 121.8 deaths per 100 waitlist-years [3], respectively. Many deaths are attributable to acute exacerbations, but transplant in the setting of AE-IPF is also associated with worse outcomes. A 2018 analysis of 89 listed IPF patients showed 1- and 3-year post-transplant survival of 71% and 60%, respectively, for those transplanted in the midst of an AE-IPF, compared to 94% and 90% for those with stable pre-transplant disease [123]. This and other studies have documented an association between higher LAS at transplant and worse post-transplant outcomes [124], further reinforcing the need for timely transplant referral in ILD.
During an acute exacerbation, close communication with a LTx centre is required to review candidacy and listing status. Currently >60% of worldwide lung transplants are allocated based on the LAS, including in Eurotransplant and the USA [125], and scores should be updated upon presentation and during exacerbations. Some nations use other forms of high-emergency allocation systems with varying criteria that a patient may qualify for during acute exacerbations, a practice that has been shown to reduce waiting-list mortality [125, 126].
Potential options for bridging with mechanical support should also be reviewed. With improvements in technologies and experience, extracorporeal life support (ECLS) bridging is being increasingly used with improving outcomes [127, 128]. In a 2018 propensity-matched analysis, 49 patients (mean age 44 years; 29 (59%) with restrictive lung disease) bridged to LTx with mechanical ventilation plus ECLS were compared with unbridged controls, as well as a cohort bridged with mechanical ventilation alone [127]. 1-year post-transplant survival was 79.5% in those bridged with mechanical ventilation plus ECLS, which was not statistically different from controls. However, bridging is resource-intensive and certainly an important risk factor for poor post-transplant outcomes [13]. Patient selection is critical, with outcomes having shown to be best in experienced centres, age ≤40 years, awake/ambulatory systems and shorter bridging duration [129–131]. Extrapulmonary organ dysfunction and uncontrolled sepsis are contraindications, and the ISHLT emphasises that patients presenting de novo (without previous evaluation for LTx) represent higher-risk candidates [13, 14].
Single versus double LTx for ILD
The growth in worldwide LTx volume over the past two decades is largely composed of DLTx, which comprised 81% of total transplants in 2018, compared to only 50% in 2000 [1]. That said, the decision on single LTx (SLTx) versus DLTx continues to garner debate in ILD. SLTx provides an opportunity to serve two recipients, a very important advantage given the growing supply–demand mismatch in LTx in the modern era. Moreover, in patients who may be candidates for SLTx or DLTx, studies have demonstrated that listing for either option, as opposed to only DLTx, is associated with decreased waiting-list mortality and increased transplant rate, without compromising 1- or 5-year post-transplant survival [132–134]. Surgically, compared to DLTX, SLTx leads to decreased use of cardiopulmonary bypass, operative and ischaemic times, and duration of mechanical ventilation and intensive care unit stays, factors that may be particularly advantageous for older or more frail patients [135, 136]. SLTx has shown comparable or even superior post-transplant outcomes in the first 3–12 months and in older patients, with lower rates of death from primary graft dysfunction [136, 137]. Longer-term, despite lower lung function, recipients of SLTx versus DLTx have been shown to have similar improvements in health-related quality of life [138].
Other literature supports DLTx as the optimal procedure choice in ILD. Among >60 000 transplants (1992–2017), the ISHLT median survival after DLTx was 7.8 years, compared to 4.8 years after SLTx [1]. In 4134 patients with IPF, a 2015 analysis demonstrated adjusted median survival of 65.2 months versus 50.4 months (p<0.001) with DLTx and SLTx, respectively [139]. A 2018 analysis confirmed these findings among patients with restrictive lung disease, demonstrating 10-year survival rates of 55% versus 32%, respectively [140]. Contrary to earlier reports in older patients, in a 2015 study of nearly 1000 patients with IPF aged ≥65 years, DLTx after propensity-matching was associated with no difference in early survival, and significantly improved 5-year survival (48.7% versus 35.2%, p<0.01) compared to SLTx [141]. The potential advantages of DLTx for ILD are probably most pronounced in younger patients, and those with associated PH or higher LAS [140, 142].
Ultimately, a flexible approach is warranted in ILD, with the choice of procedure best determined by individual programmes on a case-by-case basis factoring in age, frailty, overall disease severity including LAS and pulmonary artery pressures, anatomic factors and availability and suitability of donor lung(s).
Outcomes and considerations after LTx for ILD
Although improving, outcomes following LTx are inferior to transplantation of other solid organs, with the majority of deaths related to infections or CLAD [1]. ISHLT registry data show that among ILD recipients surviving >5 years, ∼25% of deaths are due to malignancy including lymphoma, and nearly 7% are due to cardiovascular causes [143]. Although the general management of patients transplanted for ILD is similar to the overall LTx population, several medical comorbidities warrant increased attention for their ability to impact morbidity and long-term survival (table 4, figure 1) [143].
TABLE 4.
Morbidity rates in survivors at 5 years after lung transplantation for interstitial lung disease
| Idiopathic interstitial pneumonia % of survivors with listed diagnosis | Other interstitial lung diseases % of survivors with listed diagnosis | |
| Hypertension | 79.5 | 80.0 |
| Creatinine >2.5 mg·dL−1 | 35.8 | 34.4 |
| Chronic dialysis or renal transplant | 2.7 | 2.7 |
| Hyperlipidaemia | 63.4 | 57.1 |
| Diabetes | 37.7 | 33.2 |
Data from the International Society for Heart and Lung Transplantation 2016 registry [143].
Coronary artery disease
Cardiovascular disease is common in ILD, probably due to inflammation, endothelial injury, lipid abnormalities and/or disease treatments [144, 145]. CAD in particular has increased incidence in IPF and some CTDs including systemic lupus erythematosus and rheumatoid arthritis, where it is recognised as an important cause of mortality [144–147]. The prevalence of CAD is as high as 68% in IPF patients undergoing cardiac catheterisation during a pre-transplant evaluation [133], and in patients referred for LTx, after adjustment for traditional risk factors fibrotic lung disease has been independently associated with increased CAD risk compared to other diagnoses [148]. Carefully selected patients with CAD can undergo successful LTx without increased mortality, but a vigilant approach is required after transplant to monitor symptoms and optimise cardiovascular risk factors [149].
Gastrointestinal disease
Many candidates with ILD may be considered for antireflux surgery before LTx [120]. Fundoplication is often considered after LTx if pre-transplant surgery is deemed unsafe, or if a patient develops post-transplant GOR symptoms or lung function decline. For those with early post-transplant GOR, observational studies of mixed populations including ILD have shown antireflux surgery to improve mortality, lung function and freedom from BOS [121, 150–152], with the effects most pronounced if performed early after LTx. Additionally, guidelines recommend considering GOR as a cause of post-transplant pulmonary decline including CLAD [150], where antireflux surgery has been associated with improved lung function [153].
Gastrointestinal dysmotility is common after LTx, with one study showing delayed gastric emptying in >50% of patients transplanted for restrictive lung disease [154]. Dysmotility has been associated with increased risk of BOS [155], and although this finding has not been consistent, it can certainly increase symptoms, impact drug absorption and render conventional antireflux surgery unsafe in those with co-existing GOR [13]. Particularly important for CTDs including systemic sclerosis, in experienced centres, carefully selected patients with severe oesophageal dysmotility can have reasonable outcomes after LTx using a cautious, multidisciplinary approach including speech pathology, nutrition and thorough education on GOR and aspiration precautions [62, 64]. After LTx for systemic sclerosis, some centres describe a prolonged nil-per-mouth approach with post-pyloric tube feeding until a patient demonstrates pulmonary stability and adequate swallowing function on objective studies [64]. Others use a time-based approach, extending enteral nutrition to ≥6 months post-transplant [65].
Post-transplant complications of telomere biology disorders
The post-transplant risks related to chromosomal telomere shortening in both sporadic and familial ILD are being increasingly recognised. Anaemia occurs after LTx in nearly all recipients with known telomere shortening and can require recurrent transfusions and/or erythropoietin supplementation [83, 85, 86]. Small studies have shown leukopenia, filgrastim requirement and thrombocytopenia in up to 83%, 33% and 88% of patients, respectively [84, 86]. Myelodysplastic syndrome has been reported and should be considered in refractory cases [85], and general cancer risk also appears to be increased [78]. Infectious complications are common, including cytomegalovirus, for which treatment can be challenging, particularly given the associated bone marrow toxicities [85]. Chronic renal disease and elevations in transaminase levels have been demonstrated in up to 80–85% of patients [86]. Together, the various complications often lead to intolerance of immunosuppression, most frequently leading to reductions or complete cessation of the antiproliferative agent [85, 86].
Somewhat paradoxically, patients with ILD and known telomere shortening also appear to be at greater risk of CLAD after LTx, with one study showing incidence of 50% versus 23% (p=0.022) in recipients with telomere length less than or greater than the 10th percentile, respectively [83]. The authors suggested potential mechanisms for this finding including general immune dysregulation, altered adaptive immunity and propensity for lower respiratory tract infections driving airway inflammation [83], and it is also conceivable that reduced immunosuppression itself may contribute.
Optimal management after LTx in patients with telomere disorders is unclear, but requires closer monitoring for haematological, malignant and other complications, and reduced immunosuppression is often required. Consultation from a haematologist familiar with telomere disorders should be considered, and care may also require co-management with infectious diseases, particularly in cases of persistent or resistant cytomegalovirus.
Native lung considerations in SLTx recipients
Progression of fibrotic lung disease in the native lung is common anecdotally and was shown to occur in all patients receiving SLTx for IPF in one small series [156]. Despite this, hypoxic vasoconstriction leads to appropriate diversion of 60–90% of blood flow to the allograft in most ILD patients receiving SLTx [157], lessening the clinical importance of native lung function after transplant.
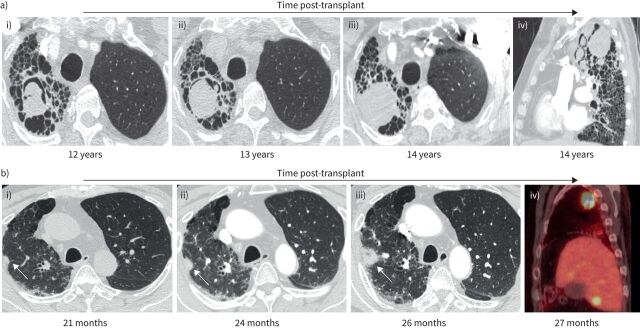
Several specific complications in the native fibrotic lung have been reported after SLTx for ILD including infections, mycetomas, pneumothorax and bronchopleural fistula [7, 157, 158] (figure 2). Most importantly, with fibrotic disease carrying a five-fold increased risk of malignancy compared to the general population that may be amplified with post-transplant immunosuppression, native lung cancers have been reported in up to 10% of ILD SLTx recipients [158–160]. Detection can be difficult due to fibrosis and outcomes are poor, with reported survival after diagnosis <1 year [160, 161]. With these risks in mind, some programmes perform routine CT imaging in SLTx recipients, though more data are needed to guide the optimal approach.
FIGURE 2.
Examples of post-transplant complications in the native fibrotic lung after single lung transplantation (SLTx). a) Images from a 57-year-old male 12 years after left SLTx for familial idiopathic pulmonary fibrosis; i) demonstrates a mycetoma in the native right upper lobe on axial computed tomography images. Bronchoalveolar lavage cultures from the (native) right upper lobe as well as from the (allograft) left upper lobe grew Aspergillus fumigatus. He was treated with prolonged voriconazole, but surveillance imaging showed increasing size of the mycetoma at ii) 13 and iii) 14 years post-transplant, with iv) sagittal imaging also demonstrating several new, smaller mycetomas. b) Images from a 62-year-old male 21 months after left SLTx for rheumatoid arthritis-associated interstitial lung disease. On axial computed tomography, i) demonstrates a small nodule versus focus of scarring superimposed upon underlying fibrosis in the native lung (arrow). ii, iii) Surveillance imaging demonstrated evolution into a clear nodule which increased in size over 5 months (arrows). iv) Positron emission tomography (sagittal image) confirmed a hypermetabolic right upper lobe nodule, along with multiple hypermetabolic lesions in the liver consistent with metastases. Percutaneous biopsy of the lung nodule confirmed adenocarcinoma. The patient died at 29 months post-transplant due to complications from brain metastases.
Disease recurrence in the allograft
Recurrence of native disease in the lung allograft is rare, probably due to post-transplant immunosuppression, and, particularly in older recipients a relatively short average graft survival compared to typical disease onset. One study reported that only 1% of 1934 LTx recipients developed disease recurrence [75]. Incidence was highest in sarcoidosis, with nine (35%) out of 26 developing recurrent radiographic or pathological signs. In a more recent analysis, among 30 recipients of LTx for sarcoidosis, histological and radiographic recurrence were documented in seven (23.3%) and one (0.4%), respectively [162]. Interestingly, acute rejection rate was significantly lower in those that developed recurrent sarcoidosis, and recurrence did not impact 1- or 5-year survival. Recurrence of hypersensitivity pneumonitis [71], Langerhans cell histiocytosis [75], desquamative interstitial pneumonitis [163] and NSIP have all been reported in the allograft, and an index of suspicion should be maintained after LTx for these entities [164], but clinically relevant disease is quite rare. Recurrence of IPF in the allograft lung has not been reported to date.
Conclusions
LTx offers the potential for vastly improved quality and duration of life for patients with advanced and/or progressive fibrotic ILD. With an increasing proportion of transplants for ILD it is important for both general and transplant pulmonologists to appreciate the complexities specific to this population that impact candidacy, pre-transplant risks and post-transplant management. In most cases, disease progression should prompt early referral to a LTx centre concurrent with care at an ILD centre to guide slowing the fibrotic lung disease, stabilising overall clinical status and optimising a candidate for LTx. Candidacy and procedure choice remain influenced by centre-specific policies. Recognition of common comorbidities in ILD is also required after LTx to optimise the chance of long-term survival.
Future directions
Further study is needed to optimise care and improve outcomes with LTx for ILD. The shortage of adequate donor lungs is especially important to recognise with increasing transplant volumes and proportion of transplants for ILD. Particularly with antifibrotics, improved methods are needed to determine prognosis in candidates with various types of ILD and identify those in greatest need of LTx. The use of marginal lungs, including with ex vivo lung perfusion, and how expanded-criteria lungs may be used in sicker candidates with ILD warrants attention. Serving two candidates with SLTx (versus DLTx) also provides an opportunity to reduce the number of patients dying without transplant; determining which patients may be best suited for SLTx, how to ensure that both donor lungs are used and the optimal management strategies after SLTx all represent areas of interest.
Finally, the transplant community is transitioning toward higher-risk, sicker candidates, and more data are needed to guide optimal practice in those with ILD and advanced age, frailty, CTD-associated issues including oesophageal dysmotility, respiratory failure requiring bridging and telomere biology disorders. This includes not only candidacy for LTx, but also personalising post-transplant care including immunosuppression to reduce infectious and malignant complications while still protecting against CLAD. Based on the antiproliferative characteristics of antifibrotic agents, treatment clinical trials with antifibrotic agents for CLAD are worthwhile considerations to pursue biological plausibility.
Footnotes
Provenance: Commissioned article, peer reviewed.
Conflict of interest: S.G. Kapnadak has nothing to disclose.
Conflict of interest: G. Raghu reports personal fees and other funding from Boehringer Ingelheim, and other funding from Roche-Genentech, outside the submitted work.
References
- 1.Chambers DC, Cherikh WS, Harhay MO, et al. . The International Thoracic Organ Transplant Registry of the International Society for Heart and Lung Transplantation: thirty-sixth adult lung and heart–lung transplantation report – 2019; focus theme: donor and recipient size match. J Heart Lung Transplant 2019; 38: 1042–1055. doi: 10.1016/j.healun.2019.08.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chambers DC, Zuckermann A, Cherikh WS, et al. . The International Thoracic Organ Transplant Registry of the International Society for Heart and Lung Transplantation: 37th adult lung transplantation report – 2020; focus on deceased donor characteristics. J Heart Lung Transplant 2020; 39: 1016–1027. doi: 10.1016/j.healun.2020.07.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Valapour M, Lehr CJ, Skeans MA, et al. . OPTN/SRTR 2018 annual data report: lung. Am J Transplant 2020; 20: Suppl. s1, 427–508. [DOI] [PubMed] [Google Scholar]
- 4.Lehr CJ, Skeans M, Valapour M. Validating thoracic simulated allocation model predictions for impact of broader geographic sharing of donor lungs on transplant waitlist outcomes. J Heart Lung Transplant 2020; 39: 433–440. doi: 10.1016/j.healun.2019.11.003 [DOI] [PubMed] [Google Scholar]
- 5.Mooney JJ, Bhattacharya J, Dhillon GS. Effect of broader geographic sharing of donor lungs on lung transplant waitlist outcomes. J Heart Lung Transplant 2019; 38: 136–144. doi: 10.1016/j.healun.2018.09.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Riou J, Boëlle PY, Christie JD, et al. . High emergency organ allocation rule in lung transplantation: a simulation study. ERJ Open Res 2017; 3: 00020-2017. doi: 10.1183/23120541.00020-2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Thabut G, Mal H, Castier Y, et al. . Survival benefit of lung transplantation for patients with idiopathic pulmonary fibrosis. J Thorac Cardiovasc Surg 2003; 126: 469–475. doi: 10.1016/S0022-5223(03)00600-7 [DOI] [PubMed] [Google Scholar]
- 8.Vock DM, Durheim MT, Tsuang WM, et al. . Survival benefit of lung transplantation in the modern era of lung allocation. Ann Am Thorac Soc 2017; 14: 172–181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hosenpud JD, Bennett LE, Keck BM, et al. . Effect of diagnosis on survival benefit of lung transplantation for end-stage lung disease. Lancet 1998; 351: 24–27. doi: 10.1016/S0140-6736(97)06405-2 [DOI] [PubMed] [Google Scholar]
- 10.Raghu G, Collard HR, Egan JJ, et al. . An official ATS/ERS/JRS/ALAT statement: idiopathic pulmonary fibrosis: evidence-based guidelines for diagnosis and management. Am J Respir Crit Care Med 2011; 183: 788–824. doi: 10.1164/rccm.2009-040GL [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Raghu G, Rochwerg B, Zhang Y, et al. . An official ATS/ERS/JRS/ALAT clinical practice guideline: treatment of idiopathic pulmonary fibrosis. an update of the 2011 clinical practice guideline. Am J Respir Crit Care Med 2015; 192: e3–e19. doi: 10.1164/rccm.201506-1063ST [DOI] [PubMed] [Google Scholar]
- 12.Glanville AR. Counterpoint: should every patient with idiopathic pulmonary fibrosis be referred for transplant evaluation? No. Chest 2020; 157: 1413–1414. doi: 10.1016/j.chest.2019.12.031 [DOI] [PubMed] [Google Scholar]
- 13.Leard LE, Holm A, Valapour M, et al. . Consensus document for the selection of lung transplant candidates: an update from the International Society for Heart and Lung Transplantation. J Heart Lung Transplant 2021; in press [ 10.1016/j.healun.2021.07.005]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Weill D, Benden C, Corris PA, et al. . A consensus document for the selection of lung transplant candidates: 2014 – an update from the Pulmonary Transplantation Council of the International Society for Heart and Lung Transplantation. J Heart Lung Transplant 2015; 34: 1–15. doi: 10.1016/j.healun.2014.06.014 [DOI] [PubMed] [Google Scholar]
- 15.Fernández Pérez ER, Daniels CE, Schroeder DR, et al. . Incidence, prevalence, and clinical course of idiopathic pulmonary fibrosis: a population-based study. Chest 2010; 137: 129–137. doi: 10.1378/chest.09-1002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Flaherty KR, Toews GB, Travis WD, et al. . Clinical significance of histological classification of idiopathic interstitial pneumonia. Eur RespirJ 2002; 19: 275–283. doi: 10.1183/09031936.02.00182002 [DOI] [PubMed] [Google Scholar]
- 17.Bjoraker JA, Ryu JH, Edwin MK, et al. . Prognostic significance of histopathologic subsets in idiopathic pulmonary fibrosis. Am J Respir Crit Care Med 1998; 157: 199–203. doi: 10.1164/ajrccm.157.1.9704130 [DOI] [PubMed] [Google Scholar]
- 18.Brown AW, Shlobin OA, Weir N, et al. . Dynamic patient counseling: a novel concept in idiopathic pulmonary fibrosis. Chest 2012; 142: 1005–1010. doi: 10.1378/chest.12-0298 [DOI] [PubMed] [Google Scholar]
- 19.King TE Jr, Bradford WZ, Castro-Bernardini S, et al. . A phase 3 trial of pirfenidone in patients with idiopathic pulmonary fibrosis. N Engl J Med 2014; 370: 2083–2092. doi: 10.1056/NEJMoa1402582 [DOI] [PubMed] [Google Scholar]
- 20.Richeldi L, du Bois RM, Raghu G, et al. . Efficacy and safety of nintedanib in idiopathic pulmonary fibrosis. N Engl J Med 2014; 370: 2071–2082. doi: 10.1056/NEJMoa1402584 [DOI] [PubMed] [Google Scholar]
- 21.Nathan SD, Albera C, Bradford WZ, et al. . Effect of pirfenidone on mortality: pooled analyses and meta-analyses of clinical trials in idiopathic pulmonary fibrosis. Lancet Respir Med 2017; 5: 33–41. doi: 10.1016/S2213-2600(16)30326-5 [DOI] [PubMed] [Google Scholar]
- 22.Richeldi L, Costabel U, Selman M, et al. . Efficacy of a tyrosine kinase inhibitor in idiopathic pulmonary fibrosis. N Engl J Med 2011; 365: 1079–1087. doi: 10.1056/NEJMoa1103690 [DOI] [PubMed] [Google Scholar]
- 23.Richeldi L, Kreuter M, Selman M, et al. . Long-term treatment of patients with idiopathic pulmonary fibrosis with nintedanib: results from the TOMORROW trial and its open-label extension. Thorax 2018; 73: 581–583. doi: 10.1136/thoraxjnl-2016-209701 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Thomeer MJ, Vansteenkiste J, Verbeken EK, et al. . Interstitial lung diseases: characteristics at diagnosis and mortality risk assessment. Respir Med 2004; 98: 567–573. doi: 10.1016/j.rmed.2003.10.015 [DOI] [PubMed] [Google Scholar]
- 25.Cottin V, Hirani NA, Hotchkin DL, et al. . Presentation, diagnosis and clinical course of the spectrum of progressive-fibrosing interstitial lung diseases. Eur Respir Rev 2018; 27: 180076. doi: 10.1183/16000617.0076-2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Park JH, Kim DS, Park IN, et al. . Prognosis of fibrotic interstitial pneumonia: idiopathic versus collagen vascular disease-related subtypes. Am J Respir Crit Care Med 2007; 175: 705–711. [DOI] [PubMed] [Google Scholar]
- 27.Nasser M, Larrieu S, Si-Mohamed S, et al. . Progressive fibrosing interstitial lung disease: a clinical cohort (the PROGRESS study). Eur Respir J 2021; 57: 2002718. doi: 10.1183/13993003.02718-2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Flaherty KR, Wells AU, Cottin V, et al. . Nintedanib in progressive fibrosing interstitial lung diseases. N Engl J Med 2019; 381: 1718–1727. doi: 10.1056/NEJMoa1908681 [DOI] [PubMed] [Google Scholar]
- 29.Maher TM, Corte TJ, Fischer A, et al. . Pirfenidone in patients with unclassifiable progressive fibrosing interstitial lung disease: a double-blind, randomised, placebo-controlled, phase 2 trial. Lancet Respir Med 2020; 8: 147–157. doi: 10.1016/S2213-2600(19)30341-8 [DOI] [PubMed] [Google Scholar]
- 30.Behr J, Neuser P, Prasse A, et al. . Exploring efficacy and safety of oral pirfenidone for progressive, non-IPF lung fibrosis (RELIEF) – a randomized, double-blind, placebo-controlled, parallel group, multi-center, phase II trial. BMC Pulm Med 2017; 17: 122. doi: 10.1186/s12890-017-0462-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Distler O, Highland KB, Gahlemann M, et al. . Nintedanib for systemic sclerosis-associated interstitial lung disease. N Engl J Med 2019; 380: 2518–2528. doi: 10.1056/NEJMoa1903076 [DOI] [PubMed] [Google Scholar]
- 32.Wijsenbeek M, Cottin V. Spectrum of fibrotic lung diseases. N Engl J Med 2020; 383: 958–968. doi: 10.1056/NEJMra2005230 [DOI] [PubMed] [Google Scholar]
- 33.Nunes H, Schubel K, Piver D, et al. . Nonspecific interstitial pneumonia: survival is influenced by the underlying cause. Eur Respir J 2015; 45: 746–755. doi: 10.1183/09031936.00148613 [DOI] [PubMed] [Google Scholar]
- 34.Alberti ML, Malet Ruiz JM, Fernández ME, et al. . Comparative survival analysis between idiopathic pulmonary fibrosis and chronic hypersensitivity pneumonitis. Pulmonology 2020; 26: 3–9. doi: 10.1016/j.pulmoe.2019.08.007 [DOI] [PubMed] [Google Scholar]
- 35.Ganapathi AM, Mulvihill MS, Englum BR, et al. . Transplant size mismatch in restrictive lung disease. Transpl Int 2017; 30: 378–387. doi: 10.1111/tri.12913 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tague LK, Witt CA, Byers DE, et al. . Association between allosensitization and waiting list outcomes among adult lung transplant candidates in the United States. Ann Am Thorac Soc 2019; 16: 846–852. doi: 10.1513/AnnalsATS.201810-713OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sell JL, Bacchetta M, Goldfarb SB, et al. . Short stature and access to lung transplantation in the United States. A cohort study. Am J Respir Crit Care Med 2016; 193: 681–688. doi: 10.1164/rccm.201507-1279OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Raghu G, Ley B, Brown KK, et al. . Risk factors for disease progression in idiopathic pulmonary fibrosis. Thorax 2020; 75: 78–80. doi: 10.1136/thoraxjnl-2019-213620 [DOI] [PubMed] [Google Scholar]
- 39.Snyder L, Neely ML, Hellkamp AS, et al. . Predictors of death or lung transplant after a diagnosis of idiopathic pulmonary fibrosis: insights from the IPF-PRO Registry. Respir Res 2019; 20: 105. doi: 10.1186/s12931-019-1043-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hayes D Jr, Black SM, Tobias JD, et al. . Influence of pulmonary hypertension on patients with idiopathic pulmonary fibrosis awaiting lung transplantation. Ann Thorac Surg 2016; 101: 246–252. doi: 10.1016/j.athoracsur.2015.06.024 [DOI] [PubMed] [Google Scholar]
- 41.Collard HR, King TE Jr, Bartelson BB, et al. . Changes in clinical and physiologic variables predict survival in idiopathic pulmonary fibrosis. Am J Respir Crit Care Med 2003; 168: 538–542. doi: 10.1164/rccm.200211-1311OC [DOI] [PubMed] [Google Scholar]
- 42.Ratwani AP, Ahmad KI, Barnett SD, et al. . Connective tissue disease-associated interstitial lung disease and outcomes after hospitalization: a cohort study. Respir Med 2019; 154: 1–5. doi: 10.1016/j.rmed.2019.05.020 [DOI] [PubMed] [Google Scholar]
- 43.Kirkil G, Lower EE, Baughman RP. Predictors of mortality in pulmonary sarcoidosis. Chest 2018; 153: 105–113. doi: 10.1016/j.chest.2017.07.008 [DOI] [PubMed] [Google Scholar]
- 44.du Bois RM, Weycker D, Albera C, et al. . Six-minute-walk test in idiopathic pulmonary fibrosis: test validation and minimal clinically important difference. Am J Respir Crit Care Med 2011; 183: 1231–1237. doi: 10.1164/rccm.201007-1179OC [DOI] [PubMed] [Google Scholar]
- 45.du Bois RM, Weycker D, Albera C, et al. . Ascertainment of individual risk of mortality for patients with idiopathic pulmonary fibrosis. Am J Respir Crit Care Med 2011; 184: 459–466. doi: 10.1164/rccm.201011-1790OC [DOI] [PubMed] [Google Scholar]
- 46.Inoue Y, Kaner RJ, Guiot J, et al. . Diagnostic and prognostic biomarkers for chronic fibrosing interstitial lung diseases with a progressive phenotype. Chest 2020; 158: 646–659. doi: 10.1016/j.chest.2020.03.037 [DOI] [PubMed] [Google Scholar]
- 47.Yoon HY, Kim TH, Seo JB, et al. . Effects of emphysema on physiological and prognostic characteristics of lung function in idiopathic pulmonary fibrosis. Respirology 2019; 24: 55–62. doi: 10.1111/resp.13387 [DOI] [PubMed] [Google Scholar]
- 48.Tong A, Howard K, Jan S, et al. . Community preferences for the allocation of solid organs for transplantation: a systematic review. Transplantation 2010; 89: 796–805. doi: 10.1097/TP.0b013e3181cf1ee1 [DOI] [PubMed] [Google Scholar]
- 49.Gutierrez C, Al-Faifi S, Chaparro C, et al. . The effect of recipient's age on lung transplant outcome. Am J Transplant 2007; 7: 1271–1277. doi: 10.1111/j.1600-6143.2006.01681.x [DOI] [PubMed] [Google Scholar]
- 50.Hayanga AJ, Aboagye JK, Hayanga HE, et al. . Contemporary analysis of early outcomes after lung transplantation in the elderly using a national registry. J Heart Lung Transplant 2015; 34: 182–188. doi: 10.1016/j.healun.2014.09.028 [DOI] [PubMed] [Google Scholar]
- 51.Courtwright A, Cantu E. Lung transplantation in elderly patients. J Thorac Dis 2017; 9: 3346–3351. doi: 10.21037/jtd.2017.08.31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Vadnerkar A, Toyoda Y, Crespo M, et al. . Age-specific complications among lung transplant recipients 60 years and older. J Heart Lung Transplant 2011; 30: 273–281. doi: 10.1016/j.healun.2010.08.032 [DOI] [PubMed] [Google Scholar]
- 53.Mosher CL, Weber JM, Frankel CW, et al. . Risk factors for mortality in lung transplant recipients aged ≥65 years: a retrospective cohort study of 5,815 patients in the scientific registry of transplant recipients. J Heart Lung Transplant 2020; 40: 42–55. doi: 10.1016/j.healun.2020.10.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Schweiger T, Hoetzenecker K. Is chronological age still a hard selection criterion for lung transplantation? J Heart Lung Transplant 2021; 40: 99–100. doi: 10.1016/j.healun.2020.11.011 [DOI] [PubMed] [Google Scholar]
- 55.Lederer DJ, Wilt JS, D'Ovidio F, et al. . Obesity and underweight are associated with an increased risk of death after lung transplantation. Am J Respir Crit Care Med 2009; 180: 887–895. doi: 10.1164/rccm.200903-0425OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Clausen ES, Frankel C, Palmer SM, et al. . Pre-transplant weight loss and clinical outcomes after lung transplantation. J Heart Lung Transplant 2018; 37: 1443–1447. doi: 10.1016/j.healun.2018.07.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Park JE, Kim SY, Song JH, et al. . Comparison of short-term outcomes for connective tissue disease-related interstitial lung disease and idiopathic pulmonary fibrosis after lung transplantation. J Thorac Dis 2018; 10: 1538–1547. doi: 10.21037/jtd.2018.02.50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Yazdani A, Singer LG, Strand V, et al. . Survival and quality of life in rheumatoid arthritis-associated interstitial lung disease after lung transplantation. J Heart Lung Transplant 2014; 33: 514–520. doi: 10.1016/j.healun.2014.01.858 [DOI] [PubMed] [Google Scholar]
- 59.Courtwright AM, El-Chemaly S, Dellaripa PF, et al. . Survival and outcomes after lung transplantation for non-scleroderma connective tissue-related interstitial lung disease. J Heart Lung Transplant 2017; 36: 763–769. doi: 10.1016/j.healun.2016.12.013 [DOI] [PubMed] [Google Scholar]
- 60.Ameye H, Ruttens D, Benveniste O, et al. . Is lung transplantation a valuable therapeutic option for patients with pulmonary polymyositis? Experiences from the Leuven transplant cohort. Transplant Proc 2014; 46: 3147–3153. doi: 10.1016/j.transproceed.2014.09.163 [DOI] [PubMed] [Google Scholar]
- 61.Takagishi T, Ostrowski R, Alex C, et al. . Survival and extrapulmonary course of connective tissue disease after lung transplantation. J Clin Rheumatol 2012; 18: 283–289. doi: 10.1097/RHU.0b013e3182676089 [DOI] [PubMed] [Google Scholar]
- 62.Sottile PD, Iturbe D, Katsumoto TR, et al. . Outcomes in systemic sclerosis-related lung disease after lung transplantation. Transplantation 2013; 95: 975–980. doi: 10.1097/TP.0b013e3182845f23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Miele CH, Schwab K, Saggar R, et al. . Lung transplant outcomes in systemic sclerosis with significant esophageal dysfunction. A comprehensive single-center experience. Ann Am Thorac Soc 2016; 13: 793–802. doi: 10.1513/AnnalsATS.201512-806OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Crespo MM, Bermudez CA, Dew MA, et al. . Lung transplant in patients with scleroderma compared with pulmonary fibrosis. Short- and long-term outcomes. Ann Am Thorac Soc 2016; 13: 784–792. doi: 10.1513/AnnalsATS.201503-177OC [DOI] [PubMed] [Google Scholar]
- 65.Chan EY, Goodarzi A, Sinha N, et al. . Long-term survival in bilateral lung transplantation for scleroderma-related lung disease. Ann Thorac Surg 2018; 105: 893–900. doi: 10.1016/j.athoracsur.2017.09.038 [DOI] [PubMed] [Google Scholar]
- 66.Pradère P, Tudorache I, Magnusson J, et al. . Lung transplantation for scleroderma lung disease: an international, multicenter, observational cohort study. J Heart Lung Transplant 2018; 37: 903–911. doi: 10.1016/j.healun.2018.03.003 [DOI] [PubMed] [Google Scholar]
- 67.Wajda N, Zhu Z, Jandarov R, et al. . Clinical outcomes and survival following lung transplantation in patients with pulmonary Langerhans cell histiocytosis. Respirology 2020; 25: 644–650. doi: 10.1111/resp.13671 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Hayes D Jr, Hayes KT, Hayes HC, et al. . Long-term survival after lung transplantation in patients with silicosis and other occupational lung disease. Lung 2015; 193: 927–931. doi: 10.1007/s00408-015-9781-z [DOI] [PubMed] [Google Scholar]
- 69.Joubert KD, Awori Hayanga J, Strollo DC, et al. . Outcomes after lung transplantation for patients with occupational lung diseases. Clin Transplant 2019; 33: e13460. doi: 10.1111/ctr.13460 [DOI] [PubMed] [Google Scholar]
- 70.Ali MS, Ramalingam VS, Haasler G, et al. . Pleuroparenchymal fibroelastosis (PPFE) treated with lung transplantation and review of the literature. BMJ Case Rep 2019; 12: e229402. doi: 10.1136/bcr-2019-229402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Kern RM, Singer JP, Koth L, et al. . Lung transplantation for hypersensitivity pneumonitis. Chest 2015; 147: 1558–1565. doi: 10.1378/chest.14-1543 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Meyer KC. Lung transplantation for pulmonary sarcoidosis. Sarcoidosis Vasc Diffuse Lung Dis 2019; 36: 92–107. doi: 10.36141/svdld.v36i2.7163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Wille KM, Gaggar A, Hajari AS, et al. . Bronchiolitis obliterans syndrome and survival following lung transplantation for patients with sarcoidosis. Sarcoidosis Vasc Diffuse Lung Dis 2008; 25: 117–124. [PubMed] [Google Scholar]
- 74.Taimeh Z, Hertz MI, Shumway S, et al. . Lung transplantation for pulmonary sarcoidosis. Twenty-five years of experience in the USA. Thorax 2016; 71: 378–379. doi: 10.1136/thoraxjnl-2015-207497 [DOI] [PubMed] [Google Scholar]
- 75.Collins J, Hartman MJ, Warner TF, et al. . Frequency and CT findings of recurrent disease after lung transplantation. Radiology 2001; 219: 503–509. doi: 10.1148/radiology.219.2.r01ma12503 [DOI] [PubMed] [Google Scholar]
- 76.George PM, Patterson CM, Reed AK, et al. . Lung transplantation for idiopathic pulmonary fibrosis. Lancet Respir Med 2019; 7: 271–282. doi: 10.1016/S2213-2600(18)30502-2 [DOI] [PubMed] [Google Scholar]
- 77.Armanios M. Telomeres and age-related disease: how telomere biology informs clinical paradigms. J Clin Invest 2013; 123: 996–1002. doi: 10.1172/JCI66370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Boscolo-Rizzo P, Da Mosto MC, Rampazzo E, et al. . Telomeres and telomerase in head and neck squamous cell carcinoma: from pathogenesis to clinical implications. Cancer Metastasis Rev 2016; 35: 457–474. doi: 10.1007/s10555-016-9633-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Cronkhite JT, Xing C, Raghu G, et al. . Telomere shortening in familial and sporadic pulmonary fibrosis. Am J Respir Crit Care Med 2008; 178: 729–737. doi: 10.1164/rccm.200804-550OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Snetselaar R, van Moorsel CHM, Kazemier KM, et al. . Telomere length in interstitial lung diseases. Chest 2015; 148: 1011–1018. doi: 10.1378/chest.14-3078 [DOI] [PubMed] [Google Scholar]
- 81.Newton CA, Batra K, Torrealba J, et al. . Telomere-related lung fibrosis is diagnostically heterogeneous but uniformly progressive. Eur Respir J 2016; 48: 1710–1720. doi: 10.1183/13993003.00308-2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Newton CA, Zhang D, Oldham JM, et al. . Telomere length and use of immunosuppressive medications in idiopathic pulmonary fibrosis. Am J Respir Crit Care Med 2019; 200: 336–347. doi: 10.1164/rccm.201809-1646OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Newton CA, Kozlitina J, Lines JR, et al. . Telomere length in patients with pulmonary fibrosis associated with chronic lung allograft dysfunction and post-lung transplantation survival. J Heart Lung Transplant 2017; 36: 845–853. doi: 10.1016/j.healun.2017.02.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Silhan LL, Shah PD, Chambers DC, et al. . Lung transplantation in telomerase mutation carriers with pulmonary fibrosis. Eur Respir J 2014; 44: 178–187. doi: 10.1183/09031936.00060014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Borie R, Kannengiesser C, Hirschi S, et al. . Severe hematologic complications after lung transplantation in patients with telomerase complex mutations. J Heart Lung Transplant 2015; 34: 538–546. doi: 10.1016/j.healun.2014.11.010 [DOI] [PubMed] [Google Scholar]
- 86.Tokman S, Singer JP, Devine MS, et al. . Clinical outcomes of lung transplant recipients with telomerase mutations. J Heart Lung Transplant 2015; 34: 1318–1324. doi: 10.1016/j.healun.2015.05.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Lanken PN, Terry PB, DeLisser HM, et al. . An Official American Thoracic Society clinical policy statement: palliative care for patients with respiratory diseases and critical illnesses. Am J Respir Crit Care Med 2008; 177: 912–927. doi: 10.1164/rccm.200605-587ST [DOI] [PubMed] [Google Scholar]
- 88.Bonella F, Wijsenbeek M, Molina-Molina M, et al. . European IPF Patient Charter: unmet needs and a call to action for healthcare policymakers. Eur Respir J 2016; 47: 597–606. doi: 10.1183/13993003.01204-2015 [DOI] [PubMed] [Google Scholar]
- 89.Singh S, Sharma BB, Bairwa M, et al. . Management of interstitial lung diseases: a consensus statement of the Indian Chest Society (ICS) and National College of Chest Physicians (NCCP). Lung India 2020; 37: 359–378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Caminati A, Lonati C, Cassandro R, et al. . Comorbidities in idiopathic pulmonary fibrosis: an underestimated issue. Eur Respir Rev 2019; 28: 190044. doi: 10.1183/16000617.0044-2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Kolb M, Raghu G, Wells AU, et al. . Nintedanib plus sildenafil in patients with idiopathic pulmonary fibrosis. N Engl J Med 2018; 379: 1722–1731. doi: 10.1056/NEJMoa1811737 [DOI] [PubMed] [Google Scholar]
- 92.Nasir BS, Mulvihill MS, Barac YD, et al. . Single lung transplantation in patients with severe secondary pulmonary hypertension. J Heart Lung Transplant 2019; 38: 939–948. doi: 10.1016/j.healun.2019.06.014 [DOI] [PubMed] [Google Scholar]
- 93.Han MK, Bach DS, Hagan PG, et al. . Sildenafil preserves exercise capacity in patients with idiopathic pulmonary fibrosis and right-sided ventricular dysfunction. Chest 2013; 143: 1699–1708. doi: 10.1378/chest.12-1594 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Hayes D Jr, Higgins RS, Black SM, et al. . Effect of pulmonary hypertension on survival in patients with idiopathic pulmonary fibrosis after lung transplantation: an analysis of the United Network of Organ Sharing registry. J Heart Lung Transplant 2015, 34: 430–437. doi: 10.1016/j.healun.2014.09.004 [DOI] [PubMed] [Google Scholar]
- 95.Whelan TP, Dunitz JM, Kelly RF, et al. . Effect of preoperative pulmonary artery pressure on early survival after lung transplantation for idiopathic pulmonary fibrosis. J Heart Lung Transplant 2005; 24: 1269–1274. doi: 10.1016/j.healun.2004.10.014 [DOI] [PubMed] [Google Scholar]
- 96.Simonneau G, Montani D, Celermajer DS, et al. . Haemodynamic definitions and updated clinical classification of pulmonary hypertension. Eur Respir J 2019; 53: 1801913. doi: 10.1183/13993003.01913-2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Nathan SD, Barbera JA, Gaine SP, et al. . Pulmonary hypertension in chronic lung disease and hypoxia. Eur Respir J 2019; 53: 1801914. doi: 10.1183/13993003.01914-2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.McAnally KJ, Valentine VG, LaPlace SG, et al. . Effect of pre-transplantation prednisone on survival after lung transplantation. J Heart Lung Transplant 2006; 25: 67–74. doi: 10.1016/j.healun.2005.07.012 [DOI] [PubMed] [Google Scholar]
- 99.Park SJ, Nguyen DQ, Savik K, et al. . Pre-transplant corticosteroid use and outcome in lung transplantation. J Heart Lung Transplant 2001; 20: 304–309. doi: 10.1016/S1053-2498(00)00316-8 [DOI] [PubMed] [Google Scholar]
- 100.Leuschner G, Stocker F, Veit T, et al. . Outcome of lung transplantation in idiopathic pulmonary fibrosis with previous anti-fibrotic therapy. J Heart Lung Transplant 2017; 37: P268–P274. [DOI] [PubMed] [Google Scholar]
- 101.Mackintosh JA, Munsif M, Ranzenbacher L, et al. . Risk of anastomotic dehiscence in patients with pulmonary fibrosis transplanted while receiving antifibrotics: experience of the Australian Lung Transplant Collaborative. J Heart Lung Transplant 2019; 38: 553–559. doi: 10.1016/j.healun.2019.02.005 [DOI] [PubMed] [Google Scholar]
- 102.Singer JP, Diamond JM, Anderson MR, et al. . Frailty phenotypes and mortality after lung transplantation: a prospective cohort study. Am J Transplant 2018; 18: 1995–2004. doi: 10.1111/ajt.14873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Singer JP, Diamond JM, Gries CJ, et al. . Frailty phenotypes, disability, and outcomes in adult candidates for lung transplantation. Am J Respir Crit Care Med 2015; 192: 1325–1334. doi: 10.1164/rccm.201506-1150OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Castleberry AW, Englum BR, Snyder LD, et al. . The utility of preoperative six-minute-walk distance in lung transplantation. Am J Respir Crit Care Med 2015; 192: 843–852. doi: 10.1164/rccm.201409-1698OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Weig T, Milger K, Langhans B, et al. . Core muscle size predicts postoperative outcome in lung transplant candidates. Ann Thorac Surg 2016; 101: 1318–1325. doi: 10.1016/j.athoracsur.2015.10.041 [DOI] [PubMed] [Google Scholar]
- 106.Rozenberg D, Mathur S, Wickerson L, et al. . Frailty and clinical benefits with lung transplantation. J Heart Lung Transplant 2018; 37: 1245–1253. doi: 10.1016/j.healun.2018.06.005 [DOI] [PubMed] [Google Scholar]
- 107.Venado A, McCulloch C, Greenland JR, et al. . Frailty trajectories in adult lung transplantation: a cohort study. J Heart Lung Transplant 2019; 38: 699–707. doi: 10.1016/j.healun.2019.03.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Lee S, Paik HC, Haam SJ, et al. . Sarcopenia of thoracic muscle mass is not a risk factor for survival in lung transplant recipients. J Thorac Dis 2016; 8: 2011–2017. doi: 10.21037/jtd.2016.07.06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Li M, Mathur S, Chowdhury NA, et al. . Pulmonary rehabilitation in lung transplant candidates. J Heart Lung Transplant 2013; 32: 626–632. doi: 10.1016/j.healun.2013.04.002 [DOI] [PubMed] [Google Scholar]
- 110.Wickerson L, Rozenberg D, Janaudis-Ferreira T, et al. . Physical rehabilitation for lung transplant candidates and recipients: an evidence-informed clinical approach. World J Transplant 2016; 6: 517–531. doi: 10.5500/wjt.v6.i3.517 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Tobin RW, Pope CE. 2nd, Pellegrini CA,, et al. Increased prevalence of gastroesophageal reflux in patients with idiopathic pulmonary fibrosis. Am J Respir Crit Care Med 1998; 158: 1804–1808. doi: 10.1164/ajrccm.158.6.9804105 [DOI] [PubMed] [Google Scholar]
- 112.Schachter LM, Dixon J, Pierce RJ, et al. . Severe gastroesophageal reflux is associated with reduced carbon monoxide diffusing capacity. Chest 2003; 123: 1932–1938. doi: 10.1378/chest.123.6.1932 [DOI] [PubMed] [Google Scholar]
- 113.Lee JS, Collard HR, Raghu G, et al. . Does chronic microaspiration cause idiopathic pulmonary fibrosis? Am J Med 2010, 123: 304–311. doi: 10.1016/j.amjmed.2009.07.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Richardson C, Agrawal R, Lee J, et al. . Esophageal dilatation and interstitial lung disease in systemic sclerosis: a cross-sectional study. Semin Arthritis Rheum 2016; 46: 109–114. doi: 10.1016/j.semarthrit.2016.02.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Lock G, Pfeifer M, Straub RH, et al. . Association of esophageal dysfunction and pulmonary function impairment in systemic sclerosis. Am J Gastroenterol 1998; 93: 341–345. doi: 10.1111/j.1572-0241.1998.00341.x [DOI] [PubMed] [Google Scholar]
- 116.Raghu G, Pellegrini CA, Yow E, et al. . Laparoscopic anti-reflux surgery for the treatment of idiopathic pulmonary fibrosis (WRAP-IPF): a multicentre, randomised, controlled phase 2 trial. Lancet Respir Med 2018; 6: 707–714. doi: 10.1016/S2213-2600(18)30301-1 [DOI] [PubMed] [Google Scholar]
- 117.Lo WK, Burakoff R, Goldberg HJ, et al. . Pre-transplant impedance measures of reflux are associated with early allograft injury after lung transplantation. J Heart Lung Transplant 2015; 34: 26–35. doi: 10.1016/j.healun.2014.09.005 [DOI] [PubMed] [Google Scholar]
- 118.Hartwig MG, Anderson DJ, Onaitis MW, et al. . Fundoplication after lung transplantation prevents the allograft dysfunction associated with reflux. Ann Thorac Surg 2011; 92: 462–468. doi: 10.1016/j.athoracsur.2011.04.035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.King BJ, Iyer H, Leidi AA, et al. . Gastroesophageal reflux in bronchiolitis obliterans syndrome: a new perspective. J Heart Lung Transplant 2009; 28: 870–875. doi: 10.1016/j.healun.2009.05.040 [DOI] [PubMed] [Google Scholar]
- 120.Lo WK, Goldberg HJ, Wee J, et al. . Both pre-transplant and early post-transplant antireflux surgery prevent development of early allograft injury after lung transplantation. J Gastrointest Surg 2016; 20: 111–118. doi: 10.1007/s11605-015-2983-0 [DOI] [PubMed] [Google Scholar]
- 121.Biswas Roy S, Elnahas S, Serrone R, et al. . Early fundoplication is associated with slower decline in lung function after lung transplantation in patients with gastroesophageal reflux disease. J Thorac Cardiovasc Surg 2018; 155: 2762–2771. doi: 10.1016/j.jtcvs.2018.02.009 [DOI] [PubMed] [Google Scholar]
- 122.Collard HR, Ryerson CJ, Corte TJ, et al. . Acute exacerbation of idiopathic pulmonary fibrosis. An international working group report. Am J Respir Crit Care Med 2016; 194: 265–275. doi: 10.1164/rccm.201604-0801CI [DOI] [PubMed] [Google Scholar]
- 123.Dotan Y, Vaidy A, Shapiro WB, et al. . Effect of acute exacerbation of idiopathic pulmonary fibrosis on lung transplantation outcome. Chest 2018; 154: 818–826. doi: 10.1016/j.chest.2018.06.027 [DOI] [PubMed] [Google Scholar]
- 124.Russo MJ, Iribarne A, Hong KN, et al. . High lung allocation score is associated with increased morbidity and mortality following transplantation. Chest 2010; 137: 651–657. doi: 10.1378/chest.09-0319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.van der Mark SC, Hoek RAS, Hellemons ME. Developments in lung transplantation over the past decade. Eur Respir Rev 2020; 29: 190132. doi: 10.1183/16000617.0132-2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Román A, Calvo V, Ussetti P, et al. . Urgent lung transplantation in Spain. Transplant Proc 2005; 37: 3987–3990. doi: 10.1016/j.transproceed.2005.09.117 [DOI] [PubMed] [Google Scholar]
- 127.Hayanga AJ, Du AL, Joubert K, et al. . Mechanical ventilation and extracorporeal membrane oxygenation as a bridging strategy to lung transplantation: significant gains in survival. Am J Transplant 2018; 18: 125–135. doi: 10.1111/ajt.14422 [DOI] [PubMed] [Google Scholar]
- 128.Hayanga JWA, Hayanga HK, Holmes SD, et al. . Mechanical ventilation and extracorporeal membrane oxygenation as a bridge to lung transplantation: closing the gap. J Heart Lung Transplant 2019; 38: 1104–1111. doi: 10.1016/j.healun.2019.06.026 [DOI] [PubMed] [Google Scholar]
- 129.Fuehner T, Kuehn C, Hadem J, et al. . Extracorporeal membrane oxygenation in awake patients as bridge to lung transplantation. Am J Respir Crit Care Med 2012; 185: 763–768. doi: 10.1164/rccm.201109-1599OC [DOI] [PubMed] [Google Scholar]
- 130.Lafarge M, Mordant P, Thabut G, et al. . Experience of extracorporeal membrane oxygenation as a bridge to lung transplantation in France. J Heart Lung Transplant 2013; 32: 905–913. doi: 10.1016/j.healun.2013.06.009 [DOI] [PubMed] [Google Scholar]
- 131.Biscotti M, Gannon WD, Agerstrand C, et al. . Awake extracorporeal membrane oxygenation as bridge to lung transplantation: a 9-year experience. Ann Thorac Surg 2017; 104: 412–419. doi: 10.1016/j.athoracsur.2016.11.056 [DOI] [PubMed] [Google Scholar]
- 132.Anderson MR, Tabah A, RoyChoudhury A, et al. . Procedure preference and intention-to-treat outcomes after listing for lung transplantation among U.S. adults. A cohort study. Ann Am Thorac Soc 2019; 16: 231–239. doi: 10.1513/AnnalsATS.201804-258OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Nathan SD, Shlobin OA, Ahmad S, et al. . Comparison of wait times and mortality for idiopathic pulmonary fibrosis patients listed for single or bilateral lung transplantation. J Heart Lung Transplant 2010; 29: 1165–1171. doi: 10.1016/j.healun.2010.05.014 [DOI] [PubMed] [Google Scholar]
- 134.Chauhan D, Karanam AB, Merlo A, et al. . Post-transplant survival in idiopathic pulmonary fibrosis patients concurrently listed for single and double lung transplantation. J Heart Lung Transplant 2016; 35: 657–660. doi: 10.1016/j.healun.2015.12.030 [DOI] [PubMed] [Google Scholar]
- 135.Nwakanma LU, Simpkins CE, Williams JA, et al. . Impact of bilateral versus single lung transplantation on survival in recipients 60 years of age and older: analysis of United Network for Organ Sharing database. J Thorac Cardiovasc Surg 2007; 133: 541–547. doi: 10.1016/j.jtcvs.2006.09.062 [DOI] [PubMed] [Google Scholar]
- 136.De Oliveira NC, Osaki S, Maloney J, et al. . Lung transplant for interstitial lung disease: outcomes for single versus bilateral lung transplantation. Interact Cardiovasc Thorac Surg 2012; 14: 263–267. doi: 10.1093/icvts/ivr085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Thabut G, Christie JD, Ravaud P, et al. . Survival after bilateral versus single-lung transplantation for idiopathic pulmonary fibrosis. Ann Intern Med 2009; 151: 767–774. doi: 10.7326/0003-4819-151-11-200912010-00004 [DOI] [PubMed] [Google Scholar]
- 138.Gerbase MW, Spiliopoulos A, Rochat T, et al. . Health-related quality of life following single or bilateral lung transplantation: a 7-year comparison to functional outcome. Chest 2005; 128: 1371–1378. doi: 10.1378/chest.128.3.1371 [DOI] [PubMed] [Google Scholar]
- 139.Schaffer JM, Singh SK, Reitz BA, et al. . Single- vs double-lung transplantation in patients with chronic obstructive pulmonary disease and idiopathic pulmonary fibrosis since the implementation of lung allocation based on medical need. JAMA 2015; 313: 936–948. doi: 10.1001/jama.2015.1175 [DOI] [PubMed] [Google Scholar]
- 140.Villavicencio MA, Axtell AL, Osho A, et al. . Single- versus double-lung transplantation in pulmonary fibrosis: impact of age and pulmonary hypertension. Ann Thorac Surg 2018; 106: 856–863. doi: 10.1016/j.athoracsur.2018.04.060 [DOI] [PubMed] [Google Scholar]
- 141.Gulack BC, Ganapathi AM, Speicher PJ, et al. . What is the optimal transplant for older patients with idiopathic pulmonary fibrosis? Ann Thorac Surg 2015; 100: 1826–1833. doi: 10.1016/j.athoracsur.2015.05.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Black MC, Trivedi J, Schumer EM, et al. . Double lung transplants have significantly improved survival compared with single lung transplants in high lung allocation score patients. Ann Thorac Surg 2014, 98: 1737–1741. doi: 10.1016/j.athoracsur.2014.05.072 [DOI] [PubMed] [Google Scholar]
- 143.Yusen RD, Edwards LB, Dipchand AI, et al. . The registry of the International Society for Heart and Lung Transplantation: thirty-third adult lung and heart-lung transplant report – 2016; focus theme: primary diagnostic indications for transplant. J Heart Lung Transplant 2016; 35: 1170–1184. doi: 10.1016/j.healun.2016.09.001 [DOI] [PubMed] [Google Scholar]
- 144.Clarson LE, Bajpai R, Whittle R, et al. . Interstitial lung disease is a risk factor for ischaemic heart disease and myocardial infarction. Heart 2020; 106: 916–922. doi: 10.1136/heartjnl-2019-315511 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Hubbard RB, Smith C, Le Jeune I, et al. . The association between idiopathic pulmonary fibrosis and vascular disease: a population-based study. Am J Respir Crit Care Med 2008; 178: 1257–1261. doi: 10.1164/rccm.200805-725OC [DOI] [PubMed] [Google Scholar]
- 146.Mantel Ä, Holmqvist M, Jernberg T, et al. . Rheumatoid arthritis is associated with a more severe presentation of acute coronary syndrome and worse short-term outcome. Eur Heart J 2015; 36: 3413–3422. doi: 10.1093/eurheartj/ehv461 [DOI] [PubMed] [Google Scholar]
- 147.Asanuma Y, Oeser A, Shintani AK, et al. . Premature coronary-artery atherosclerosis in systemic lupus erythematosus. N Engl J Med 2003; 349: 2407–2415. doi: 10.1056/NEJMoa035611 [DOI] [PubMed] [Google Scholar]
- 148.Kizer JR, Zisman DA, Blumenthal NP, et al. . Association between pulmonary fibrosis and coronary artery disease. Arch Intern Med 2004; 164: 551–556. doi: 10.1001/archinte.164.5.551 [DOI] [PubMed] [Google Scholar]
- 149.Khandhar SJ, Althouse AD, Mulukutla S, et al. . Postoperative outcomes and management strategies for coronary artery disease in patients in need of a lung transplantation. Clin Transplant 2017, 31: e13026. doi: 10.1111/ctr.13026. [DOI] [PubMed] [Google Scholar]
- 150.Meyer KC, Raghu G, Verleden GM, et al. . An international ISHLT/ATS/ERS clinical practice guideline: diagnosis and management of bronchiolitis obliterans syndrome. Eur Respir J 2014; 44: 1479–1503. doi: 10.1183/09031936.00107514 [DOI] [PubMed] [Google Scholar]
- 151.Cantu E 3rd, Appel JZ 3rd, Hartwig MG, et al. . J. Maxwell Chamberlain Memorial Paper. Early fundoplication prevents chronic allograft dysfunction in patients with gastroesophageal reflux disease. Ann Thorac Surg 2004; 78: 1142–1151. doi: 10.1016/j.athoracsur.2004.04.044 [DOI] [PubMed] [Google Scholar]
- 152.Davidson JR, Franklin D, Kumar S, et al. . Fundoplication to preserve allograft function after lung transplant: systematic review and meta-analysis. J Thorac Cardiovasc Surg 2020; 160: 858–866. doi: 10.1016/j.jtcvs.2019.10.185 [DOI] [PubMed] [Google Scholar]
- 153.Davis RD Jr, Lau CL, Eubanks S, et al. . Improved lung allograft function after fundoplication in patients with gastroesophageal reflux disease undergoing lung transplantation. J Thorac Cardiovasc Surg 2003; 125: 533–542. doi: 10.1067/mtc.2003.166 [DOI] [PubMed] [Google Scholar]
- 154.Hirji SA, Gulack BC, Englum BR, et al. . Lung transplantation delays gastric motility in patients without prior gastrointestinal surgery – a single-center experience of 412 consecutive patients. Clin Transplant 2017, 31: e13065. doi: 10.1111/ctr.13065 [DOI] [PubMed] [Google Scholar]
- 155.Raviv Y, D'Ovidio F, Pierre A, et al. . Prevalence of gastroparesis before and after lung transplantation and its association with lung allograft outcomes. Clin Transplant 2012; 26: 133–142. doi: 10.1111/j.1399-0012.2011.01434.x [DOI] [PubMed] [Google Scholar]
- 156.Wahidi MM, Ravenel J, Palmer SM, et al. . Progression of idiopathic pulmonary fibrosis in native lungs after single lung transplantation. Chest 2002; 121: 2072–2076. doi: 10.1378/chest.121.6.2072 [DOI] [PubMed] [Google Scholar]
- 157.King CS, Khandhar S, Burton N, et al. . Native lung complications in single-lung transplant recipients and the role of pneumonectomy. J Heart Lung Transplant 2009; 28: 851–856. doi: 10.1016/j.healun.2009.04.023 [DOI] [PubMed] [Google Scholar]
- 158.Van Raemdonck D, Vos R, Yserbyt J, et al. . Lung cancer: a rare indication for, but frequent complication after lung transplantation. J Thorac Dis 2016; 8: Suppl. 11, S915–S924. doi: 10.21037/jtd.2016.11.05 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Oldham JM, Collard HR. Comorbid conditions in idiopathic pulmonary fibrosis: recognition and management. Front Med 2017; 4: 123. doi: 10.3389/fmed.2017.00123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Triplette M, Crothers K, Mahale P, et al. . Risk of lung cancer in lung transplant recipients in the United States. Am J Transplant 2019; 19: 1478–1490. doi: 10.1111/ajt.15181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Olland AB, Falcoz PE, Santelmo N, et al. . Primary lung cancer in lung transplant recipients. Ann Thorac Surg 2014; 98: 362–371. doi: 10.1016/j.athoracsur.2014.04.014 [DOI] [PubMed] [Google Scholar]
- 162.Banga A, Sahoo D, Lane CR, et al. . Disease recurrence and acute cellular rejection episodes during the first year after lung transplantation among patients with sarcoidosis. Transplantation 2015; 99: 1940–1945. doi: 10.1097/TP.0000000000000673 [DOI] [PubMed] [Google Scholar]
- 163.King MB, Jessurun J, Hertz MI. Recurrence of desquamative interstitial pneumonia after lung transplantation. Am J Respir Crit Care Med 1997; 156: 2003–2005. doi: 10.1164/ajrccm.156.6.9703001 [DOI] [PubMed] [Google Scholar]
- 164.Scallan C, Venado A, Han L, et al. . Recurrent pulmonary fibrosis in a lung allograft secondary to de novo antisynthetase syndrome. Ann Am Thorac Soc 2020; 17: 901–904. doi: 10.1513/AnnalsATS.202002-126RL [DOI] [PubMed] [Google Scholar]