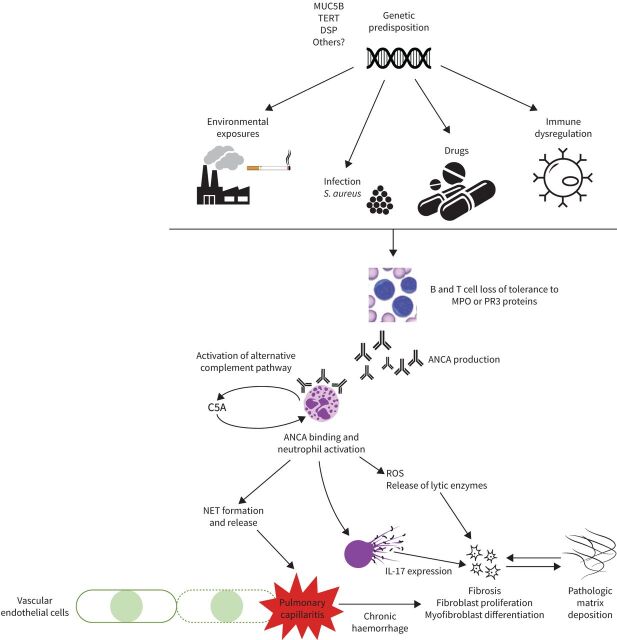
FIGURE 1.
Schematic illustration of proposed concepts of pathogenesis in antineutrophil cytoplasmic antibody (ANCA)-mediated lung disease including pulmonary capillaritis and interstitial lung disease (ILD). The pathogenesis of ANCA-ILD is thought to involve an interplay of factors (including environmental exposures such as silica or cigarette smoke, drugs including hydralazine, infection, immune dysregulation) and genetic predisposition (such as MUC5B, telomerase reverse transcriptase, desmoplakin and others). These factors lead to the generation of an aberrant autoimmune response including loss of T- and B-cell tolerance and ANCA production. ANCA induces neutrophils to secrete chemoattractants which lead to activation of the alternative complement pathway, with anaphylatoxin C5A as an important player, leading to amplification loops and further priming of neutrophils [19, 57]. ANCA-activated neutrophils locally release reactive oxygen species (ROS), proteolytic enzymes such as elastase or neutrophil extracellular trap (NET) formation, which injures vascular endothelial cells leading to pulmonary capillaritis. Furthermore, interleukin-17 (IL-17)-bearing NETs have been shown to trigger human lung fibroblast activation and differentiation into myofibroblasts [60]. Other proposed mechanisms for the development of ILD in AAV include repeated episodes of alveolar haemorrhage leading to pulmonary fibrosis.