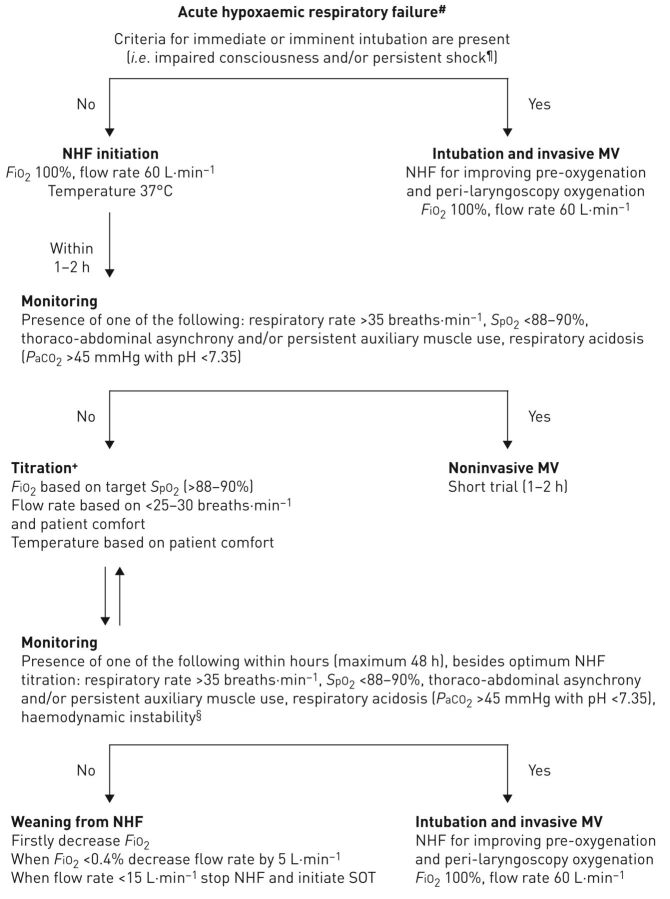
FIGURE 1.
Recommended algorithm for high-flow nasal cannula use in acute hypoxaemic respiratory failure in immunocompetent or immunocompromised patients. #: arterial oxygen tension (PaO2)/inspiratory oxygen fraction (FiO2) <300 (patients with arterial carbon dioxide tension (PaCO2) >45 mmHg and pH <7.35 are excluded); ¶: systolic arterial blood pressure <90 mmHg despite adequate fluid administration; +: the rationale for change in nasal high flow (NHF) settings are as follows. 1) Flow rate could be adjusted downwards by 5–10 L·min−1 per 1–2 h if none of the negative prognostic factors are present. However, if targets of arterial oxygen saturation measured by pulse oximetry (SpO2) and respiratory rate are not achieved, while the flow rate is <60 L·min−1, increase of flow rate by 5–10 L·min−1 is preferred to raising FiO2; 2) increase in FiO2 causes increases in PaO2 and SpO2; 3) temperature can be set at 37°C or lower (31–34°C), based on the patient's comfort; §: haemodynamic instability is defined by heart rate >140 beats·min−1 or change >20% from baseline and/or systolic arterial blood pressure >180 mmHg, <90 mmHg or decrease >40 mmHg from baseline. MV: mechanical ventilation; SOT: standard oxygen treatment.