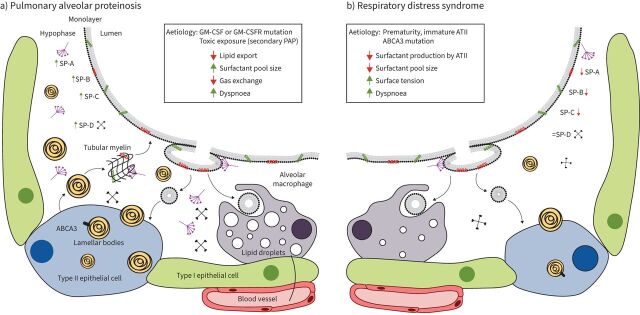
FIGURE 2.
Schematic of the alveolus and pulmonary surfactant homeostasis in primary surfactant diseases. At the air–liquid interface, a surfactant monolayer helps reduce pulmonary surface tension and separates the alveolar airspace from the aqueous hypophase. Surfactant is produced by alveolar type II epithelial cells (ATII) and secreted as lamellar bodies which organise into tubular myelin structures. Surfactant is recycled and degraded by ATII cells and alveolar macrophages, respectively, and replaced using surfactant reserves stored in the tubular myelin. a) In patients suffering from pulmonary alveolar proteinosis (PAP), failure to catabolise and export surfactant, typically due to impaired granulocyte-monocyte colony stimulating factor (GM-CSF) signalling, leads to lipid-laden alveolar macrophages and surfactant accumulation. b) On the other hand, premature birth is associated with impaired ATII cell development leading to diminished surfactant production, thus reducing surfactant phospholipid and protein secretion and increasing alveolar surface tension. Despite their inverse impacts on surfactant pool size, patients suffering from both PAP and respiratory distress syndrome experience significant dyspnoea due to impaired gas exchange and increased difficulty breathing. ABCA3: ATP binding cassette subfamily A member 3; GM-CSFR: granulocyte-monocyte colony-stimulating factor receptor; SP: surfactant protein.