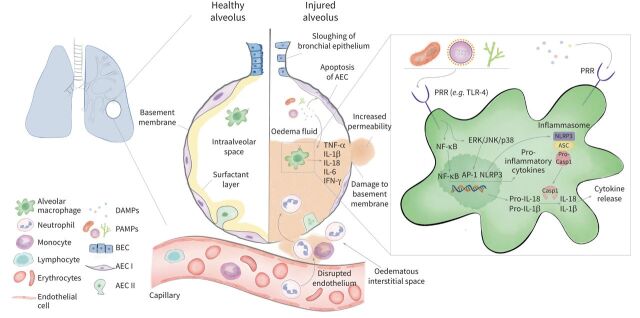
FIGURE 1.
Immuno-pathogenesis of acute respiratory distress syndrome (ARDS). In the healthy alveolus the epithelium consists of a continuous monolayer of type I and type II alveolar epithelial cells covered by a surfactant layer. Resident alveolar macrophages populate the intraalveolar space and orchestrate the inflammatory response induced by direct (pulmonary) or indirect (extrapulmonary) insults. Conserved microbial motifs so called pathogen-associated molecular patterns (PAMPs) or cell injury-associated endogenous molecules referred to as damage-associated molecular patterns (DAMPs) are recognised by pattern recognition receptors (PRRs), such as Toll-like receptors (TLRs), which are located on macrophages and various other immune cells. The subsequent activation of downstream signalling pathways including NF-κB and mitogen-activated protein kinases (extracellular signal-regulated kinase (ERK), c-Jun N-terminal kinase (JNK), p38) induces the upregulation of proinflammatory cytokines and chemokines which stimulate the transepithelial migration of neutrophils and monocytes. Excess inflammation causes alveolar cell and capillary endothelial injury resulting in the disruption of the blood–air barrier that causes the accumulation of protein-rich oedema fluid within the lungs. A key driver of the inflammatory response is the NLRP3 inflammasome which is composed of a sensor NOD-, LRR- and pyrin domain-containing protein 3 (NLRP3), an adaptor apoptosis-associated speck-like protein containing caspase-recruitment domain-containing protein (ASC) and an effector (caspase-1) and leads to the release of proinflammatory cytokines interleukin (IL)-1β and IL-18. The activation of NLRP3 requires two steps. Signal 1 is mediated by PRRs and NF-κB-regulated transcription of pro-caspase-1, pro-IL-1β and pro-IL-18. The activation signal (signal 2) is provided by a wide range of stimuli including ATP, viral RNA and pore-forming toxins, which lead to the assembly of the NLRP3 inflammasome-caspase-1 complex. This complex proteolytically cleaves pro-IL-1β and pro-IL-18 into their active forms and causes a highly inflammatory form of programmed cell death called pyroptosis. AEC I: type I alveolar epithelial cell; AEC II: type II alveolar epithelial cell; BEC: bronchial epithelial cell; CASP1: caspase-1; IFN: interferon; MAPKs: mitogen activated protein kinases.