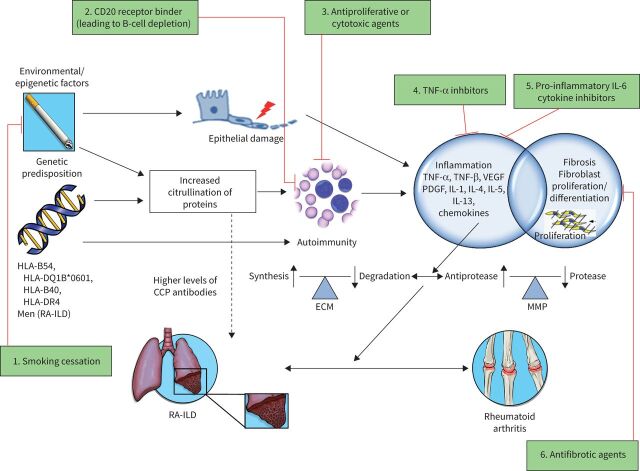
FIGURE 3.
Schematic illustration of the concepts in the pathogenesis of rheumatoid arthritis (RA)-associated interstitial lung disease (ILD) with various therapeutic targets. The pathogenesis of RA is thought to involve an interplay between various risk factors (including smoking history, male sex and older age) and genetic predisposition (such as the shared epitope HLA-DRB1). In the lung, various environmental exposures causing airway and alveolar epithelial cell damage may lead to increased citrullination of proteins which, in an individual who is genetically predisposed, is thought to trigger an inflammatory process characterised by activation of cytokines, chemokines and growth factors, such as tumour necrosis factor (TNF), vascular endothelial growth factor (VEGF), platelet-derived growth factor (PDGF) and interleukins (IL). These contribute to both proliferation and differentiation of fibroblasts, increased synthesis and deposition of extracellular matrix (ECM), and increased activity of matrix metalloproteinases (MMP), resulting in the development of ILD and pulmonary fibrosis. Fibroblasts in the synovial lining play a similar role in the pathogenesis of joint manifestations of RA. Various therapeutic targets include: 1) exposure avoidance via smoking cessation; 2) binding of CD20 receptor, leading to B-cell depletion (e.g. rituximab); 3) antiproliferative or cytotoxic agents (e.g. cyclophosphamide and mycophenolate); 4) TNF-α inhibitors (e.g. adalimumab, etanercept and infliximab); 5) pro-inflammatory IL-6 cytokine inhibitors (e.g. tocilizumab); and 6) antifibrotic agents (nintedanib and pirfenidone). Therapeutic agents not included in the figure include corticosteroids, which promote an anti-inflammatory response via inhibition of prostaglandin and leukotriene synthesis, and reduction of the number of circulating monocytes, as well as inhibiting the release of collagenase and lysosomal enzymes [71]. Also not pictured are nonbiologic (i.e. traditional or conventional) disease-modifying anti-rheumatic drugs, such as methotrexate, for which the exact mechanism in RA is unknown, but is thought to involve adenosine signalling via increase of adenosine levels leading to an intracellular cascade promoting an overall anti-inflammatory state [72]. CCP: cyclic citrullinated peptide; HLA: human leukocyte antigen. Reproduced and modified from [60] with permission.