Abstract
Background: Adenotonsillectomy is a safe and common operation to remove adenoids and tonsils. Here we decided to compare the two dosages of tranexamic acid and their effects on hemodynamic changes and anesthesia-related indexes during surgical interventions. Methods: This is a double-blinded clinical trial performed in 2019-2020 on 64 children who were candidates for adenotonsillectomy. The patients were randomly divided into two groups of 32 based on the table of random numbers. Group A received 5 mg/kg slowly tranexamic acid for 10 minutes and group B received 10 mg/kg tranexamic acid slowly for 10 minutes. The study protocol was approved by the Research committee of Isfahan University of Medical Sciences and the Ethics Committee has confirmed it (Ethics code: IR.MUI.MED.REC.1398.639) (Iranian Registry of Clinical Trials (IRCT) code: IRCT20171030037093N33, https://en.irct.ir/trial/46553). Results: The mean volume of intraoperative bleeding in children in group A is significantly higher than in children in group B (P < 0.05). However, no significant difference was observed between the length of stay in recovery and the duration of extubation and the mean dose of propofol in the two groups (P > 0.05). The mean arterial oxygen saturation of children in both groups increased significantly over time (P < 0.05). However, no significant difference was observed between the two groups (P > 0.05). According to the results, the mean HR in both groups decreased significantly over time (P < 0.05). In addition, the mean HR in children in the group B was significantly lower than children in the group A (P < 0.05). Conclusion: Administration of 10 mg/kg of tranexamic acid during tonsillectomy is associated with lower amounts of bleeding and lower heart rate than 5 mg/kg dosage. These results were in line with most previous studies.
Keywords: Anesthesia, child, general anesthesia, surgery
Introduction
The lymphoid ring of the oropharynx and nasopharynx, or the Valder ring, in the anterior part contains the lingual tonsils, the lateral part contains the palatine tonsils (or so-called tonsils) and the upper posterior part contains the pharyngeal tonsils (adenoids) [1]. Adenoid growth continues until the fifth to seventh year after birth, leading to some degree of airway obstruction, usually symptomatic between the ages of 18 and 24 months [2]. The role of adenoids and tonsils is in the development of secretory immunity and the production of secretory immunoglobulin. With their position in the upper part of the airways and gastrointestinal tract, they are responsible for immunological protection against foreign antigens [3].
Although hypertrophy of lymphoid tissues in the early years of life is due to increased immunological activity, chronic bacterial infections, allergies, and exposure to secondhand smoke are other causes of adenotonsillar hypertrophy in children [4]. Symptoms include airway obstruction. Adenotonsillar hypertrophy is a common cause of sleep apnea in children [5]. Existence of episodes of apnea and severe snoring (which alone can confirm obstructive sleep apnea). Parents describe it as a metaphor for children snoring to adults or hearing a child snoring outside the bedroom [6]. Chronic mouth breathing, frequent wakefulness during sleep, drowsiness, nightmares, poor school performance, dysphagia, hyponasal speech, rarely FTT, hypernasal speech, and anorexia indicate severe sleep disorders. As a result, the patients would be candidates for adenotonsillectomy [4].
An adenotonsillectomy is a safe and common operation to remove the adenoids and tonsils mostly performed in children. Indications of adenotonsillectomy include adenotonsillar hyperplasia with obstructive sleep apnea, failure to thrive, or abnormal dentofacial growth; suspicion of malignant disease; and (for tonsillectomy) hemorrhagic tonsillitis [7]. Adenotonsillectomy in children is associated with complications such as heavy bleeding after surgery, hematoma and inflammation of the pharynx after surgery, and severe pain after surgery, which increases morbidity, prolonged hospitalization, and tends to increase Infections and increased risk of chronic pain [8,9].
Tranexamic acid is an antifibrinolytic drug that reduces blood loss during surgery and mortality and morbidity due to bleeding following trauma [10]. Tranexamic acid is a useful medication in reducing bleeding in variable situations such as epistaxis, tooth extraction, and rhinoplasty in patients with hemophilia [11]. Tranexamic acid has antifibrinolytic characteristics and inhibits transformations of plasminogen into plasmin. It also acts by impacting fibrin and forming hemostasis. As a result, tranexamic acid might be an appropriate medication for reducing bleeding during surgeries. This drug is indicated in surgical bleeding and blood transfusion patients and can also be used topically to reduce bleeding [12].
There are few side effects from using tranexamic acid other than pain at high doses. It has been found that hemodynamic stability during surgery is associated with reduced postoperative complications, including pediatric agitation [13]. There have also been controversial results on using different dosages of tranexamic acid in patients. Since no studies have been performed to compare the hemodynamic effects of tranexamic acid in different dosages in adenotonsillectomy surgery, we decided to compare the two dosages of tranexamic acid and their effects on anesthesia-related indexes.
Methods and material
Study design
This is a double-blinded clinical trial performed in 2019-2020 in Imam Hossein pediatric hospital affiliated with Isfahan University of Medical Sciences. The current study was conducted on 64 children that were candidates for adenotonsillectomy. The study protocol was approved by the Research Committee of Isfahan University of Medical Sciences, and the Ethics committee has confirmed it (Ethics code: IR.MUI.MED.REC.1398.639) (Iranian Registry of Clinical Trials (IRCT) code: IRCT20171030037093N33).
Inclusion and exclusion criteria
The inclusion criteria were age between 5-10 years, candidates for adenotonsillectomy, American Society of Anesthesiologists (ASA) classification I and II and signing the written informed consent by the parents. Criteria for non-entry were a history of medical diseases, hemorrhagic disorders, metabolic disorders and disruption of coagulation tests (PT, PTT and INR). The exclusion criteria were any complications or abnormal bleeding during the surgery.
Premedication
After premedication, patients were separated from their parents with 0.1 mg/kg midazolam and brought to the operating room. The patients were then induced under anesthesia with 2 g/kg fentanyl, 5 mg/kg sodium thiopental and 0.5 mg/kg atracurium. They were intubated with a suitable tube, connected to a ventilator, and placed under anesthesia with a 1% isoflurane preservative. Then the patients were randomly divided into two groups of 32 based on the table of random numbers. In this method, all patients were assigned a number and, using Random Allocation Software, were divided into two groups.
Interventions
Group A received 5 mg/kg slowly tranexamic acid for 10 minutes, and group B received 10 mg/kg of tranexamic acid slowly for 10 minutes. As explained in the following, tranexamic acid with the dosage of 10 and 5 mg/kg has been used in different studies, and different results have been reported. So far, no study has compared these two dosages. Therefore, we selected 10 and 5 mg/kg dosages as interventions.
Blinding and data gathering
The method of blinding was that the drugs were drawn and coded by the researcher in equal volumes in similar syringes. The anesthetist prescribing the drugs and the nurse recording the data did not know the placement of the patients in the groups. Patients were extubated after surgery and transferred to recovery. The measured indicators in this study were: mean arterial pressure (MAP), heart rate (HR) and SPO2 before induction and during anesthesia every 15 minutes, bleeding volume during surgery based on ml, the duration of extubation (from the time of discontinuation of anesthesia to the time of extubation of patients), in recovery room, MAP, HR, and SPO2 were recorded every 15 minutes. The length of stay in recovery based on the Modified Aldrete Score was recorded in two groups and compared with each other.
Data assessments
In the recovery room, the patient’s agitation was recorded every 15 minutes according to the Pediatric Anesthesia Emergence Delirium (PAED) scale in two groups and compared with each other. A score equal to or greater than 10 was considered as emergence delirium and they were treated with propofol at a dose of 1 mg/kg. Sedation rate was recorded according to the Ramsay sedation score (RSS) in two groups every 15 minutes.
Data analysis
Data analysis was performed using descriptive and inferential statistical methods. Quantitative variables are reported as mean (standard deviation) and qualitative variables as frequency (percentage). The Chi-square-Pearson test and correlation test are used to determine the factors affecting weight disorders in children under two years of age, according to the nature of the variables under study. The significance level in all tests is considered < 0.05. All analyzes are performed using SPSS version 18 software (SW Statistics for Windows, Chicago: SPSS, Inc.).
Results
Study population
A total number of 66 pediatrics entered this study in 2020-2021. The mean age of the patients was 7.06 ± 1.7 years. In addition, 47% of the participants were girls and 53% were boys. Patients were randomly divided into two groups of 32 and 34 patients. Group A received 5 mg/kg of slow tranexamic acid for 10 minutes and group B received 10 mg/kg of slow tranexamic acid for 10 minutes. The demographic characteristics of the patients in the present study are given separately in Table 1. As Table 1 shows, no significant differences were observed between the variables of age, weight and sex of children participating in the two groups (P > 0.05).
Table 1.
Comparison of demographic variables in study groups
| Group A (N = 34) | Group B (N = 32) | P-value | |
|---|---|---|---|
| age (years)* | 6.4 ± 1.7 | 7.5 ± 1.7 | 0.051 |
| weight (Kg)* | 22.7 ± 5.3 | 24.2 ± 5.06 | 0.24 |
| gender** | |||
| girl | 15 (44%) | 16 (50%) | 0.63 |
| boy | 19 (56%) | 16 (50%) |
Quantitative variables were reported as (Mean ± Sd) and independent t-test was used to compare the means in the groups.
Qualitative variables were expressed in frequency and percentage and Chi-square test was used for intergroup comparison.
Significance level is less than 0.05.
Different parameters during surgery
Table 2 also examines the parameters measured during surgery in children participating in the present study. This table calculates the bleeding volume, extubation duration and length of stay in recovery, and the average dose of propofol in the two groups. As the results of Table 2 show, the mean volume of intraoperative bleeding in children in group A is significantly higher than in children in group B (P < 0.05). However, no significant difference was observed between the length of stay in recovery and the duration of extubation, the mean dose of propofol in the two groups (P > 0.05).
Table 2.
Comparison of the mean of variables measured during the operation in the two groups
| Group A (N = 30) | Group B (N = 30) | P-value | |
|---|---|---|---|
| Bleeding volume (cc) | 70.58 ± 21.06 | 59.4 ± 33.7 | 0.006 |
| Extubation time (min) | 10.17 ± 3.5 | 9.9 ± 3.4 | 0.89 |
| Recovery time (min) | 49.85 ± 7.12 | 50.1 ± 7.23 | 0.86 |
| The average dose of propofol (mg) | 21.5 ± 6.7 | 24.1 ± 4.5 | 0.32 |
Quantitative variables were reported as (Mean ± Sd) and independent t-test was used to compare the means in the groups. Significance level is less than 0.05.
Comparison of intraoperative hemodynamic changes
Table 3 and Figure 1 examine the two groups’ determination and comparison of intraoperative hemodynamic changes in patients undergoing adenotonsillectomy. As Table 3 and Figure 1 show, the mean arterial oxygen saturation of children in both groups increased significantly over time (P < 0.05) (Figure 1). However, no significant difference was observed between the two groups (P > 0.05). According to the results, the mean HR in both groups decreased significantly over time (P < 0.05). Also, the mean HR in children in group B was significantly lower than children in group A (P < 0.05). Table 3 show that the mean MAP in the two groups did not differ significantly over time (P > 0.05). There were also no significant differences between the two groups regarding MAP (P = 0.35).
Table 3.
Evaluation and comparison of intraoperative hemodynamic changes in patients undergoing adenotonsillectomy in two groups
| Variable | Measuring times | Group A | Group B | P-value* | P-value** |
|---|---|---|---|---|---|
| Arterial oxygen saturation (SPO2) (%) | Before injection | 95.54 ± 1.29 | 96 ± 1.61 | Intergroup 0.001 | 0.41 |
| after 15 minutes | 96.54 ± 1.12 | 96 ± 1.84 | |||
| after 30 minutes | 97 ± 1.61 | 96.8 ± 0.87 | |||
| after 45 minutes | 97.81 ± 1.07 | 97.18 ± 0.87 | |||
| after 60 minutes | 98.36 ± 0.67 | 97.72 ± 1.1 | |||
| Heart rate (per min) | Before injection | 122.09 ± 18.98 | 112.4 ± 21.5 | 0.02 | 0.01 |
| after 15 minutes | 120 ± 17.82 | 109.4 ± 25.33 | |||
| after 30 minutes | 116.8 ± 15.4 | 103.6 ± 24.9 | |||
| after 45 minutes | 114.81 ± 15.05 | 101.5 ± 24.9 | |||
| after 60 minutes | 118 ± 14.05 | 104.8 ± 22.7 | |||
| Mean arterial pressure (MAP) (mmHg) | Before injection | 70.7 ± 21.6 | 71.5 ± 15.7 | 0.36 | 0.35 |
| after 15 minutes | 77.6 ± 21.3 | 69.09 ± 14.5 | |||
| after 30 minutes | 76.6 ± 21.01 | 70.09 ± 12.6 | |||
| after 45 minutes | 77.09 ± 20.7 | 69.9 ± 12.09 | |||
| after 60 minutes | 78.9 ± 22.9 | 72.2 ± 13.1 |
Analysis of variance of repeated measures was used to compare the means of variables in the two groups.
Intergroup test results.
Intragroup test results.
Values of P < 0.05 indicate the significance of the test.
Figure 1.
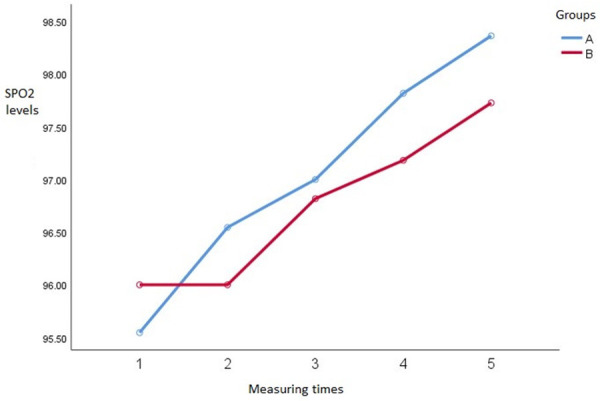
Trend of changes in mean SPO2 in two groups.
Discussion
The main aim of this study was to compare the two dosages of tranexamic acid and their effects on hemodynamic changes and anesthesia-related indexes during surgical interventions.
As mentioned earlier, adenotonsillectomy is a safe and common surgical procedure in pediatrics and intra-operative bleeding is the most important complication of this surgery that could lead to increased heart rate and disturbance in clinical conditions of the patients. There have been several strategies to minimize the amounts of bleeding in pediatrics undergoing adenotonsillectomy. The beneficial effects of tranexamic acid for reducing bleeding during various surgeries have been previously well established [14,15].
Chan and colleagues also performed a systematic review and meta-analysis of tranexamic acid in tonsillectomy. It was indicated that tranexamic acid could significantly reduce tonsillectomy blood loss volume but has no impact on the rate of patients with post-tonsillectomy hemorrhage. They also suggested that new, large and well-designed randomized controlled trials are required [16]. George and colleagues conducted another study in 2011 on 100 cases undergoing adenotonsillectomy. In this clinical trial, the intervention group received 10 mg/kg of tranexamic acid and the case group received a placebo. It was shown that this dosage of tranexamic acid is significantly effective in controlling tonsillectomy bleeding [17]. Our results also aligned with these findings showing the effectiveness of 10 mg/kg of tranexamic acid.
Robb and others evaluated bleeding during the initial 24 hours following tonsillectomy among 476 pediatrics receiving tranexamic acid at a 10-15 mg/kg. They showed that the amounts of bleeding were significantly low and = declared that perioperative tranexamic acid in a single, parenteral dose might reduce the incidence of primary hemorrhage following pediatric tonsillectomy [18].
Another study by Koizumi and colleagues in 2019 in Japan evaluated 117598 patients retrospectively. Most of the studied cases had received 5 mg/kg of tranexamic acid during the surgeries. This study showed that administration of TXA from the day of tonsillectomy was not associated with a reduction in reoperation or blood transfusion rates [19]. In the present study, we showed that the mean volume of intraoperative bleeding in children that received 5 mg/kg of tranexamic acid was significantly higher than in children that received 10 mg/kg of tranexamic acid. However, there were no significant differences in the length of stay in recovery, the duration of extubation, and the mean dose of propofol in the two groups. Our data also showed that the mean HR in both groups decreased significantly over time. The mean HR was significantly lower in children who received 10 mg/kg of tranexamic acid than in group A. The mean MAP in the two groups did not differ significantly over time. These data indicate the beneficial effects of 10 mg/kg of tranexamic acid in reducing the amounts of bleeding and also stabilizing the HR in children. The critical point of our study was that we compared two different dosages of tranexamic acid in pediatrics. Based on the results of our study, the man bleeding volume was significantly lower in patients receiving 10 mg/kg of tranexamic acid compared to 5 mg/kg. These results were consistent with previous studies.
So far, various studies have evaluated the effectiveness of tranexamic acid on bleeding during a tonsillectomy. Still, to the best of our knowledge, this is the first documented clinical trial in the English literature that compares two different dosages of tranexamic acid in pediatrics undergoing tonsillectomy. Goobie and colleagues recommended that a dosing regimen of between 10 to 30 mg/kg loading dose followed by a 5 to 10 mg/kg/h maintenance infusion rate could bring the maximum reduction in the bleeding during pediatric surgeries [20]. But on the other hand, the study by Pabinger and others did not confirm these data [21]. We believe that such differences could be due to variations in the study populations and their risk factors for bleeding. It has been shown that pediatrics of the male sex, older age, emergency hospitalization and prolonged anesthesia are vulnerable to higher bleeding [19]. As a result, more attention should be given to such patients.
The shortcomings of this study were limited study population and comparing only two dosages of tranexamic acid. Due to ethical issues, administering a placebo is contraindicated in patients undergoing this type of surgery and at high risk of bleeding. Nevertheless, we believe that further investigations on various dosages and larger populations could reveal more valuable data.
Conclusion
Based on our results, administration of 10 mg/kg of tranexamic acid during tonsillectomy is associated with lower amounts of bleeding and lower heart rate than a 5 mg/kg dosage. These results were in line with most previous studies, and we recommend using 10 mg/kg of tranexamic acid to reduce bleeding during tonsillectomy.
Acknowledgements
This study was granted by Isfahan University of Medical Sciences.
Disclosure of conflict of interest
None.
References
- 1.Ma S, Jug R, Shen S, Zhang WL, Xu HT, Yang LH. Marginal zone lymphoma of palatine tonsil with prominent plasmacytic differentiation: a CARE-compliant article and review of literature. Medicine (Baltimore) 2018;97:e9648. doi: 10.1097/MD.0000000000009648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ishida T, Manabe A, Yang SS, Yoon HS, Kanda E, Ono T. Patterns of adenoid and tonsil growth in Japanese children and adolescents: a longitudinal study. Sci Rep. 2018;8:1–7. doi: 10.1038/s41598-018-35272-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Byars SG, Stearns SC, Boomsma JJ. Association of long-term risk of respiratory, allergic, and infectious diseases with removal of adenoids and tonsils in childhood. JAMA Otolaryngol Head Neck Surg. 2018;144:594–603. doi: 10.1001/jamaoto.2018.0614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yildirim N, Şahan M, Karslioğlu Y. Adenoid hypertrophy in adults: clinical and morphological characteristics. J Int Med Res. 2008;36:157–162. doi: 10.1177/147323000803600120. [DOI] [PubMed] [Google Scholar]
- 5.Lesinskas E, Drigotas M. The incidence of adenoidal regrowth after adenoidectomy and its effect on persistent nasal symptoms. Eur Arch Otorhinolaryngol. 2009;266:469–473. doi: 10.1007/s00405-008-0892-5. [DOI] [PubMed] [Google Scholar]
- 6.Arambula A, Brown JR, Neff L. Anatomy and physiology of the palatine tonsils, adenoids, and lingual tonsils. World J Otorhinolaryngol Head Neck Surg. 2021;7:155–160. doi: 10.1016/j.wjorl.2021.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Clements AC, Dai X, Walsh JM, Sterni LM, Prichett L, Boss EF, Seal SM, Ryan MA. Outcomes of adenotonsillectomy for obstructive sleep apnea in Prader-Willi syndrome: systematic review and meta-analysis. Laryngoscope. 2021;131:898–906. doi: 10.1002/lary.28922. [DOI] [PubMed] [Google Scholar]
- 8.De Luca Canto G, Pachêco-Pereira C, Aydinoz S, Bhattacharjee R, Tan HL, Kheirandish-Gozal L, Flores-Mir C, Gozal D. Adenotonsillectomy complications: a meta-analysis. Pediatrics. 2015;136:702–718. doi: 10.1542/peds.2015-1283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Konstantinopoulou S, Gallagher P, Elden L, Garetz SL, Mitchell RB, Redline S, Rosen CL, Katz ES, Chervin RD, Amin R. Complications of adenotonsillectomy for obstructive sleep apnea in school-aged children. Int J Pediatr Otorhinolaryngol. 2015;79:240–245. doi: 10.1016/j.ijporl.2014.12.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kim HJ, Moon SH, Cho SH, Lee JD, Kim HS. Efficacy and safety of tranexamic acid in melasma: a meta-analysis and systematic review. Acta Derm Venereol. 2017;97:776–781. doi: 10.2340/00015555-2668. [DOI] [PubMed] [Google Scholar]
- 11.Myles PS, Smith JA, Forbes A, Silbert B, Jayarajah M, Painter T, Cooper DJ, Marasco S, McNeil J, Bussières JS. Tranexamic acid in patients undergoing coronary-artery surgery. N Engl J Med. 2017;376:136–148. doi: 10.1056/NEJMoa1606424. [DOI] [PubMed] [Google Scholar]
- 12.Ng W, Jerath A, Wasowicz M. Tranexamic acid: a clinical review. Anaesthesiol Intensive Ther. 2015;47:339–350. doi: 10.5603/AIT.a2015.0011. [DOI] [PubMed] [Google Scholar]
- 13.Soliman R, Alshehri A. Assessment of the effect of tranexamic acid on perioperative bleeding in pediatric patients undergoing tonsillectomy. Egypt J Anaesth. 2015;31:297–301. [Google Scholar]
- 14.Ziaei S, Joni SS, Shahriar R, Shahzamani M. Does intravenous tranexamic acid reduce bleeding during mastoidectomy? Am J Blood Res. 2020;10:46. [PMC free article] [PubMed] [Google Scholar]
- 15.Sun Q, Yu X, Nie X, Gong J, Cai M. The efficacy comparison of tranexamic acid for reducing blood loss in total knee arthroplasty at different dosage time. J Arthroplasty. 2017;32:33–36. doi: 10.1016/j.arth.2016.06.021. [DOI] [PubMed] [Google Scholar]
- 16.Chan CC, Chan YY, Tanweer F. Systematic review and meta-analysis of the use of tranexamic acid in tonsillectomy. Eur Arch Otorhinolaryngol. 2013;270:735–748. doi: 10.1007/s00405-012-2184-3. [DOI] [PubMed] [Google Scholar]
- 17.George A, Kumar R, Kumar S, Shetty S. A randomized control trial to verify the efficacy of pre-operative intra venous tranexamic acid in the control of tonsillectomy bleeding. Indian J Otolaryngol Head Neck Surg. 2011;63:20–26. doi: 10.1007/s12070-010-0095-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Robb P, Thorning G. Perioperative tranexamic acid in day-case paediatric tonsillectomy. Ann R Coll Surg Engl. 2014;96:127–129. doi: 10.1308/003588414X13814021676477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Koizumi M, Ishimaru M, Matsui H, Fushimi K, Yamasoba T, Yasunaga H. Tranexamic acid and post-tonsillectomy hemorrhage: propensity score and instrumental variable analyses. Eur Arch Otorhinolaryngol. 2019;276:249–254. doi: 10.1007/s00405-018-5192-0. [DOI] [PubMed] [Google Scholar]
- 20.Goobie SM, Faraoni D. Tranexamic acid and perioperative bleeding in children: what do we still need to know? Curr Opin Anaesthesiol. 2019;32:343–352. doi: 10.1097/ACO.0000000000000728. [DOI] [PubMed] [Google Scholar]
- 21.Pabinger I, Fries D, Schöchl H, Streif W, Toller W. Tranexamic acid for treatment and prophylaxis of bleeding and hyperfibrinolysis. Wien Klin Wochenschr. 2017;129:303–316. doi: 10.1007/s00508-017-1194-y. [DOI] [PMC free article] [PubMed] [Google Scholar]


