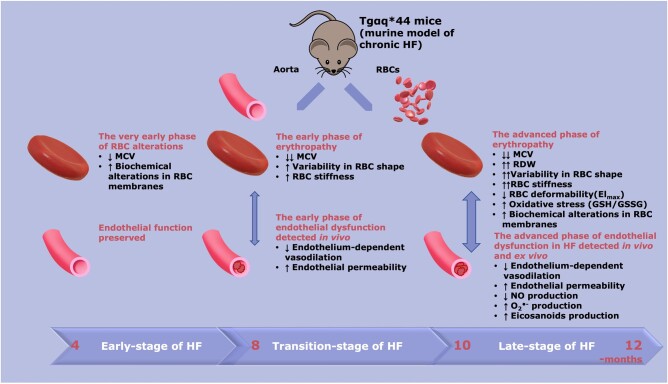
Figure 7.
Schematic diagram summarizing the temporal relationship between the progression of endothelial dysfunction and erythropathy in Tgαq*44 mice, representing the murine model of chronic HF. At early stages of HF (4 months) a decrease in MCV (P < 0.05), biochemical alterations in RBC membranes [decreased phospholipids (P < 0.0001), and unsaturation (P < 0.001)] were present; however, these changes were not associated with functional alterations of RBCs and endothelial function was fully preserved. At the transition phase of HF, apart from a decrease in MCV (P < 0.0001), a substantial increase in RBC stiffness (P < 0.0001), and alteration in RBC shape were noted (early phase of erythropathy), as well as impaired endothelium-dependent vasodilation in the aorta and an increase in endothelial permeability (P < 0.01) (early phase of endothelial dysfunction). At the end stage of HF, a number of RBC indices were greatly altered, including MCV (P < 0.0001), RDW (P < 0.05), RBC shape (P < 0.0001), RBC deformability (P < 0.01), and oxidative stress (increased GSH/GSSG ratio, P < 0.05) (advanced phase of erythropathy), and were associated with an advanced phase of endothelial dysfunction, characterized not only by functionally impaired endothelium-dependent vasodilation and increased endothelial permeability (P < 0.05) but also impaired NO production (P < 0.05), increased superoxide anion () (P < 0.05), and increased eicosanoid (P < 0.05) production. HF, heart failure; MCV, mean corpuscular volume; NO, nitric oxide; RBC, red blood cell; RDW, red blood cell distribution width.