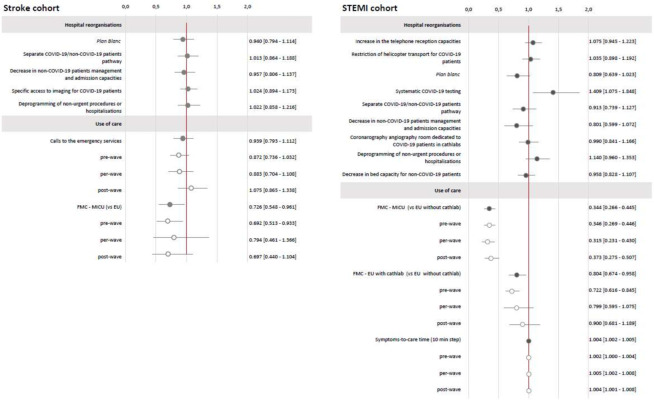
Figure 2.
Stroke and STEMI cohorts. Estimation of the reorganisations and use of care effects (95% CI) on care management times. Stroke cohort (N=4603)—estimated overall effects expressed as exp(β) with 95% CI; results of multivariate linear regression mixed models; variable to be explained: Y=log (EU admission-to-imaging time); results adjusted on period, age, gender, urbanicity of residence, FDep15, APL MG 18, residence-EU distance, presence of stroke unit, MRI 24 hours a day, presence of interventional neuroradiology unit, care during on-call activity, mode of transport, calls to emergency services activity, mRS less than 1 before stroke, NIHSS at entry, previous stroke or transient ischaemic attack. STEMI cohort (N=1843)—estimated overall effects expressed as exp(β) with 95% CI; results of multivariate linear regression mixed models; variable to be explained: Y=log (FMC-to-procedure time); results adjusted on period, age, gender, urbanicity of residence, FDep15, APL MG 18, residence-to-cathlab distance, cathlab hospital status, care during on-call activity, mode of transport, calls to emergency services activity, FMC-to-cathlab distance, diabetes mellitus, coronary artery disease or STEMI history). Light grey: interaction with the COVID-19 period, Dark grey: raw results without interaction with the COVID-19 period. APL MG 2018, potential accessibility to general practitioners; EU, emergency unit; FDep15, deprivation index; FMC, first medical contact; MICU, mobile intensive care units; mRS, modified Rankin Scale; NIHSS, National Institute of Health Stroke Score; plan blanc, emergency plan to cope with a sudden increase of activity; STEMI, ST-segment elevation myocardial infarction.