Abstract
Introduction
In the UK, National Health Service (NHS) guidelines recommend that informal carers of people living with dementia should be offered training to help them develop care skills and manage their own physical and mental health. The WHO recommends access to affordable, proven, well-designed, online technologies for education, skills training and support for dementia carers. In response to these recommendations, this multisite randomised controlled trial (RCT) is the first study in the UK to evaluate the clinical and cost-effectiveness of an online support programme developed by the WHO called ‘iSupport for dementia carers’.
Methods and analysis
350 informal carers (age 18+ years) living in Britain who self-identify as experiencing stress and depression will be recruited. They will be randomised to receive ‘iSupport’, or standardised information about caring for someone with dementia (control–comparison). Data will be collected via videoconferencing (eg, Zoom) or telephone interview at baseline, 3 months and 6 months. Intention-to-treat analysis will ascertain effectiveness in the primary outcomes (distress and depression) and combined cost, and quality-adjusted life-year data will be used to assess cost-effectiveness compared with usual care from a public sector and wider societal perspective. A mixed-methods process evaluation with a subgroup of carers in the intervention (~N=50) will explore the barriers and facilitators to implementing ‘iSupport’. A non-randomised feasibility study will adapt ‘iSupport’ for young carers (n=38 participants, age 11–17 years).
Ethics and dissemination
The research plan was scrutinised by National Institute for Health Research reviewers ahead of funding being awarded. Ethical approval was granted by Bangor University’s School of Health and Medical Sciences Academic Ethics Committee, reference number 2021-16915. Dissemination plans include delivering events for stakeholders, social media, a project website, developing policy briefings, presenting at conferences and producing articles for open access publications.
Trial registration number
ISRCTN17420703.
Keywords: dementia, telemedicine, health economics
Strengths and limitations of this study.
iSupport for dementia carers was developed by experts at the WHO and is based on techniques with proven therapeutic efficacy; consequently, the content is informed by a considerable body of evidence.
The ‘real world’ application of the randomised controlled trial requires carers to self-identify as experiencing some level of stress or depression, but some may have mild symptoms, limiting the potential for improving these primary outcomes.
Although the research assistants will be ‘blind’ to the randomisation, a limitation of the study includes being unable to completely blind the participants to their respective allocation (iSupport or information about being a carer).
Remote data collection and intervention delivery will potentially reach a broader and more diverse range of carers beyond the geographical boundaries often experienced through in-person data collection; however, this could also create challenges for recruiting to target.
The feasibility study will work with young people to generate valuable information leading to an adapted version of ‘iSupport’ for young carers.
Introduction
‘Dementia’ is an umbrella term for a cluster of symptoms that characterise neurodegenerative changes, decline and loss of cognitive functioning. Dementia is one of the leading causes of care dependency, disability and death around the world.1 The number of people living with dementia is predicted to increase globally, and it is estimated the number of people living with dementia in the UK will increase 80% by 2040.2 The limited medical treatments available for people living with dementia mean that in the UK, most people living with dementia are cared for at home,3 supported by a family member or friend who often performs care tasks similar to those carried out by paid health or social service providers. The detrimental impact of caregiving on the physical and mental health of informal carers is well documented4 5; a meta-analysis found carers were more stressed, depressed and had lower levels of subjective well-being, physical health and self-efficacy than non-carers.6
Dementia carers have expressed a need for: (A) relevant information and knowledge; (B) support with the management of care recipients’ functioning, behavioural and psychological symptoms; (C) support with their own physical and mental health; and (D) support regarding their unbalanced social life.7 In the face of these significant challenges, Action Area 5 of the WHO’s Global Action Plan on Dementia 2017–2025 prioritises supporting carers, calling for the provision of accessible evidence-based information to improve knowledge and skills and prevent stress and health problems.8
To address these challenges, the WHO developed ‘iSupport’, an evidence-informed e-health intervention designed to help dementia carers provide good care and take care of themselves. The content reflects evidence that the most effective interventions for carers’ psychological health should incorporate both an educational component to enhance knowledge and a therapeutic component, such as cognitive–behavioural therapy/cognitive reframing.9 Such interventions are often delivered in-person; however, the ongoing COVID-19 pandemic led to reductions, delays and withdrawal of many support services for carers.10 Online interventions could be one solution to providing support, negating general accessibility barriers such as carers’ time constraints or needing to travel to receive care and support,11 due to their convenience of use, low delivery costs and the ability to negate geographical barriers.12 The potential for scalability is also relevant, as few e-health interventions for carers are implemented outside a research setting.13–15 However, despite their potential, the evidence base remains limited, and high-quality studies are required to enable definitive conclusions about their effectiveness.16 In response, this study aims to contribute to this growing area of healthcare delivery.
‘iSupport’ is in the process of global implementation, and there is research underway in The Netherlands, India and Portugal,17–19 but to date, there is no published evidence as to the effectiveness of ‘iSupport’. This will be the first study to examine the effectiveness and cost-effectiveness of a globally targeted e-health intervention in a majority English-speaking population of dementia carers. It will also evaluate the feasibility of adapting ‘iSupport’ for young carers (ages 11–17 years). It is vital that current and future carers have access to education programmes that are tailored to address their particular needs,20 as current generic dementia support services are not able to address the specific challenges young carers face.
Research questions
Are carer distress and depression (primary outcomes) significantly reduced in participants allocated to receive ‘iSupport’ compared with participants allocated to a control–comparison group receiving standardised information about caring for someone with dementia?
Are symptoms of anxiety (secondary outcome) significantly reduced and resilience, relationship quality and dementia knowledge (secondary outcomes) significantly increased in participants allocated to receive ‘iSupport’ compared with participants allocated to the control–comparison group?
3. What are participant and contextual barriers and facilitators to implementation of ‘iSupport’?
4. What potential mechanisms might underpin changes in outcomes from using ‘iSupport’?
5. What is the cost-effectiveness of ‘iSupport’ compared with standardised information about dementia?
6. Is it feasible and acceptable to digitally deliver a refined ‘iSupport’ to young carers?
7. What are the carers’ perspectives of ‘iSupport’ in relation to supporting them in an ongoing or future repeated pandemic such as COVID-19?
Methods and analysis
Study design
‘iSupport’ for dementia carers is a multicentre randomised controlled trial (RCT) and feasibility study composed of four workstreams (WS). WS1 will evaluate the effectiveness of ‘iSupport’ (compared with a control–comparison) in reducing carer distress and symptoms of depression (multiple primary outcomes), reductions in anxiety, improvements in resilience, relationship quality and dementia knowledge (secondary outcomes). WS2 (process evaluation) will examine how participants engaged with ‘iSupport’, whether there are any barriers to its uptake, and any perceived benefits for the carer. WS3 (health economic evaluation) will calculate the cost-effectiveness of ‘iSupport’ from a public sector perspective21 and from a wider societal perspective. WS4 (feasibility study) will adapt ‘iSupport’ for young carers and assesses the feasibility, acceptability and uptake of conducting a larger trial. Online supplemental file 1 contains the objectives for each workstream. This protocol was developed according to the SPIRIT (2013) checklist.22 The study runs for 36 months (1 January 2021–31 December 2023). At the end of their involvement in the study, all participants will receive information about regional support services and a £20 voucher.
bmjopen-2022-064314supp001.pdf (617.7KB, pdf)
RCT participant recruitment
Carers living in England, Scotland and Wales will be recruited between December 2021 and January 2023 by researchers working from Bangor University (coordinating centre), University College London or University of Strathclyde (collaborating sites). Researchers will advertise the study through social media; our study partners (Alzheimer Scotland and Carers Trust Wales) and other non-statutory organisations will advertise the study to regional groups through their networks, and the Join Dementia Research23 register will be used to identify potential participants (online supplemental file 2). All carers who express an interest in taking part will be sent a consent form, information sheet and be invited to discuss their involvement with a researcher in a one-to-one videoconferencing or phone meeting, when the researcher would also assess their eligibility (table 1).
Table 1.
Eligibility criteria for the RCT
| Inclusion criteria | (1) Adults (age 18+ years) who self-identify as an unpaid carer of a person with dementia who is not living in a full-time care facility, caring at least weekly for at least 6 months. |
| (2) Self-identify as experiencing at least some stress, depression or anxiety. | |
| (3) The care recipient has to have a confirmed diagnosis of dementia through self-report of the carer. | |
| Exclusion criteria | (1) Receiving psychological treatment from a mental health specialist at the time of recruitment. |
| (2) Unable to comprehend written English. | |
| (3) No access to the internet. | |
| (4) Unable to give informed consent to the trial. | |
| (5) Have previously used ‘iSupport’ materials in the last 12 months. |
A nested internal pilot study at each site will monitor progression criteria over the first 6 months of recruitment. Go/review/stop criterion will be assessed by the study’s independent data monitoring committee, and decisions about the study conduct will be made in consultation with the trial steering committee and the Trial Management Group.
RCT sample size and randomisation
A meta-analysis reported that technology-based interventions for informal carers of people living with dementia are effective in reducing both depression and burden outcomes.24 Consequently, both are important outcomes for carers, and the sample size considers these as multiple primary endpoints at 6 months. The multiple primary endpoint estimator in the R package25 26 with power of 90% and significance set to 2.5%, established that 262 participants are required at 6 months to have the potential to detect an effect in at least one of these outcomes. The attrition rate was based on nine dementia intervention studies, where the mean retention rate was 15.33% (range 2%–24%). Accommodating a 25% attrition rate by 6 months, the RCT will recruit and randomise 350 participants. Randomisation uses dynamic allocation to protect against subversion.27 This ensures the trial maintains good balance to the allocation ratio of 1:1, both within each stratification variable and overall for the trial. Stratification variables will be site, along with age and gender, previously found to influence the outcome measure of caregiver distress.28
RCT ‘iSupport’ intervention iSupport is an internet-based psychoeducation and skills development intervention that can be accessed through a personal computer, tablet or mobile phone. The theoretical underpinnings of ‘iSupport’ are based on person-centred care, recognising that dementia care should reflect the individual’s needs, personality and abilities29 and are integrated into the interactive content of ‘iSupport’. The self-care techniques are based on theoretically informed programmes with some evidence for benefits, including psychoeducation, relaxation, behavioural activation, cognitive reframing and problem solving.30 Participants will access iSupport in their own homes or a place where they are able to access the internet.
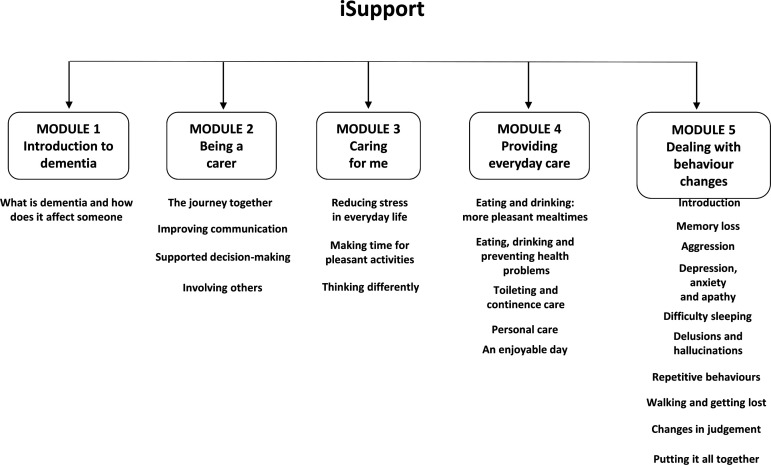
‘iSupport’ consists of five main themes and 23 accompanying exercises (figure 1). Each exercise takes approximately 5–15 min and follows the same format: information about a topic presented, short interactive exercises and questions with instant feedback on responses, a summary of the lesson and a relaxation exercise. ‘iSupport’ is based on personal choice: carers can construct their own personalised plan and access which sessions they feel are most relevant to them at that point in time. Participants will be advised to use ‘iSupport’ regularly in order to obtain the most benefit. They will be provided with the contact details of an ‘e-coach’ (member of the research team), who will explain anything that is not clear about the ‘iSupport’ programme. The ‘e-coach’ will contact participants allocated to intervention shortly after randomisation, 1 month later and 2 months later (if required by the participant). ‘iSupport’ will be translated into Welsh following WHO adaptation guidelines. Approximately one-fifth of the Welsh population speak Welsh,31 and the Welsh Government is committed to offering bilingual services as part of healthcare provision. To improve access, an audio/read aloud function is included in the iSupport programme.
Figure 1.
iSupport content.
RCT control–comparison to iSupport
The control–comparison group will receive an information booklet (online and/or hard copy) about caring for someone with dementia, developed by the Alzheimer’s Society.32 Alongside this education, carers will receive care-as-usual. They can search for other information or seek help from other providers. Participants allocated to the controlcomparison group will be provided with access to ‘iSupport’ at the end of data collection.
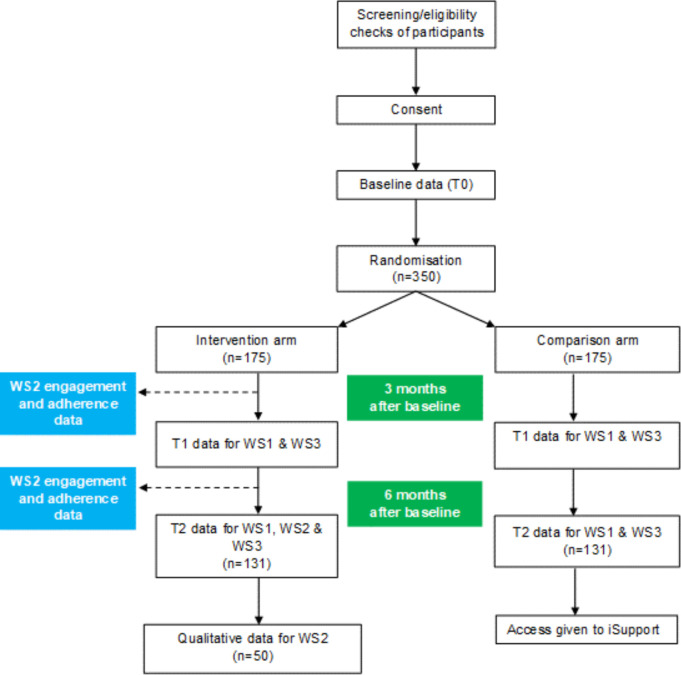
RCT data collection
Case report forms (CRFs) were initially piloted by researchers, and adjustments made to reduce the time burden to participants without affecting the study’s ability to address the research questions. Data will be collected at three time-points: baseline (T0), 3 months postbaseline (T1 follow-up) and 6 months postbaseline (T2 follow-up). Researchers will interview participants by videoconferencing or phone. Following the baseline interview, researchers will perform the randomisation and the CI, or trial manager will email the participant their group allocation details. Follow-up interviews will be administered by researchers who are blinded to group allocation. An acceptable tolerance for follow-ups will be up to 2 weeks earlier and up to 4 weeks later than the exact T1 or T2 date. Figure 2 shows the flow of the participants through the study.
Figure 2.
Recruitment flow chart.
All data will be entered into an electronic database (MACRO),33 and the study statistician will periodically monitor data quality. Table 2 shows the outcome measures, order of administration and the relevance for each workstream.
Table 2.
Data collection for iSupport RCT
| Questionnaire or study-specific questions | Time point | Workstream |
| Local COVID-19 alert level at date of assessment | T0, T1, T2 | 1,2,3 |
| Demographic questions | T0 | 1,2,3 |
| Employment, marital status and living situation questions | T0, T1, T2 | 1,2,3 |
| 12-item Zarit Burden Interview (ZBI-12)48* | T0, T1, T2 | 1,3 |
| 10-item Centre for Epidemiological Studies Depression Scale (CES-D-10)*49 | T0, T1, T2 | 1,3 |
| EQ-5D-5L50 | T0, T1, T2 | 3 |
| Resilience Scale-1451 | T0, T1, T2 | 1 |
| Generalised Anxiety Disorder Questionnaire52 | T0, T1, T2 | 1 |
| Dementia Knowledge Assessment Scale53 | T0, T1, T2 | 1 |
| Adapted Erasumus iMTA informal care questionnaire54 | T0, T1, T2 | 3 |
| Service use questions | T0, T1, T2 | 3 |
| Quality of the Carer-Patient Relationship55 | T0, T1, T2 | 1 |
| Dementia Quality of Life – Proxy measure56 | T0, T1, T2 | 1,3 |
| Researcher remains blinded to allocation question | T1, T2 | 1 |
*Indicates primary outcome measure for WS1.
RCT, randomised controlled trial; WS, workstream.
WS2 process evaluation sampling and data collection
The process evaluation uses three different approaches to data collection:
Semistructured interviews will be undertaken with up to 50 of carers in the intervention group following their T2 interview. The choice of sample size in qualitative research is an area of debate34; however, our decision was informed by Ritchie and colleagues,35 who recommend that studies employing individual interviews should undertake no more than 50 interviews in order to manage the complexity of the analysis. Baseline data will inform a purposive sampling strategy, and a qualitative sampling matrix will be developed. This matrix will include a diverse range of participant demographic characteristics such as age, gender and caring responsibilities and differences in scores across the the 12-item Zarit Burden Interview (ZBI-12) and the 10-item Centre for Epidemiological Studies Depression Scale (CES-D-10) scores (low, medium and high).
The interview topics will be guided by the process evaluation parameters described in recognised frameworks36 37 and drawing on theoretical models such as Normalisation Process Theory.38 Motives for declining participation will also be noted where consent is given to understand any barriers to participation and potential selection bias.
Data from the online platform will be collected regarding usability (eg, frequency and length of use, which modules/sessions/pages users most frequently visit, average time spend on each module/session/page, whether accessed from tablet, PC or mobile phone). The number of contacts with the e-coach will be recorded.
An online evaluation questionnaire will collect quantitative data from all study participants in the intervention arm and will be administered at 6-month follow-up (T2).39 This questionnaire will evaluate the overall usability and acceptability of the ‘iSupport’ platform in conjunction with all other data collection methods.
WS4 feasibility study: participant recruitment
Young carers and professionals who have regular contact with young carers will be recruited through stakeholders’ networks, social media and national carers associations (table 3). Researchers will approach parents or legal guardians of participants under the age of 16 years to explain their child’s involvement and obtain their consent from them. Online supplemental file 3 visualises the phases of the feasibility study.
Table 3.
Feasibility study eligibility criteria
| Inclusion criteria | Young carers (1) Young people between the ages of 11 and 17 years who self-identify as a carer of a person with dementia who is not living in a full-time care facility, caring at least weekly for at least 6 months. |
Professionals (1) Have regular contact with young people and young carers (eg, teaching staff involved in pastoral care, young carer charity workers and social workers in children’s services. |
| (2) The care recipient has to have a confirmed diagnosis of dementia (through self-report of the carer). | ||
| Exclusion criteria | (1) Receiving treatment from Child and Adolescent Mental Health Services at the time of recruitment. |
|
| (2) Unable to comprehend written English. | ||
| (3) No access to the internet. | ||
| (4) Have previously used ‘iSupport’ materials in the last 12 months. |
WS4: data collection
Phase 1: Adapting ‘iSupport’ for young carers
Three × 3-hour workshops will be conducted either in person or using videoconferencing software (eg, Zoom, Teams or Skype) depending on the government guidelines regarding COVID-19 and safety. At least 2 weeks before the workshops, participants will be given online access to ‘iSupport’ and printed materials for annotations. Workshop 1 will recruit six to eight young carers to discuss their caregiving experiences, which aspects are reflected or missing in ‘iSupport’, and opinions on the content and style of the intervention. Workshop 2 will undertake a similar exercise with six to eight professionals who work with young carers. Feedback will be used to refine ‘iSupport’, which will be shared in workshop 3 with all participants who attended the first two workshops in order to produce a ‘final’ version. Discussions around which outcomes are most important for young carers in relation to ‘iSupport’ will be used to adapt the CRF from the RCT for phase 2.
Phase 2: feasibility testing ‘iSupport’ for younger dementia carers
Young carers will test the feasibility of using the refined ‘iSupport’ and following the RCT procedures (except randomisation will not be required). After T2 data collection, participants will complete an online evaluation of their experience using ‘iSupport’. Informed by a methodological framework,40 a sample of 30 for phase 2 will provide enough information on the acceptability of the intervention, the appropriateness of data collection forms, the feasibility of recruitment and consent procedures and the most appropriate primary outcome measures.
Data analysis plans
WS1 (research questions 1 and 2)
WS1 primary analysis is an intention-to-treat (ITT) analysis, blinded to treatment allocation. The primary assessment for effectiveness will be adjusted estimates of the ZBI-12 and CES-D-10 scores between the two groups assessed at 6 months. A linear mixed-effects model adjusting for baseline scores, randomising site (random effect) and stratification variables will be fitted for each of the two primary outcomes. Similar models will be fitted for all continuous secondary outcomes. All estimates of effect will be presented together with 95% CIs. The aim is to minimse missing data; however, predictors of missingness will be investigated using regression models, and any predictors found will be considered for inclusion in the models. Multiple imputation will address missing scores where appropriate. Complier Average Causal Effect analysis will assess the impact of the number of times the ‘iSupport’ intervention was accessed. A sensitivity analysis will assess any impact of the outcome measures being completed in Welsh. A full statistical analysis plan will be written and agreed with the independent committees before completion of the data collection.
WS2 process evaluation (research questions 3, 4 and 7)
Qualitative interview data analysis will be professionally transcribed verbatim and thematically analysed41 using NVivo. Results will also be applied to aspects of the Context and Implementation of Complex Interventions checklist,42 which may reflect implementation in a ‘real world’ setting. This analysis will reveal the experiences of using iSupport and its delivery, the barriers and facilitators to its uptake and continued use and the perceived benefits for the carer participating in iSupport and the person they are caring for. Descriptive analyses will profile the System Usability Scale and intervention platform metrics regarding usability (eg, most/least frequently visited pages, the most ‘popular’ modules/sessions).
WS3 health economic evaluation (research question 5)
Primary analysis will be an ITT analysis as per WS1. Cost and quality-adjusted life-years data will be combined to calculate an incremental cost-effectiveness ratio. Cost-effectiveness acceptability curves43 will show the probability that ‘iSupport’ is cost-effective compared with the control–comparison for a range of willingness-to-pay thresholds. Secondary cost-effectiveness analyses will calculate the cost per unit change in the primary outcome measures. A subgroup analysis will be conducted on the number of times that carers in the intervention group accessed ‘iSupport’. Deterministic sensitivity analyses will be conducted to vary the costs of inputs.
WS4 feasibility study (research question 6)
Data from phase 1 workshops will be selectively transcribed, analysed and reported according to established guidance.44 All quantitative data collected during phase 2 will be presented descriptively. No inferential testing will be undertaken for this data. The mean change from baseline, associated variances and 95% CIs will be calculated for all selected outcomes. Consideration will be given to the applicability of these outcomes for development into a protocol for a future RCT if the acceptability of the intervention is proven. Success will be defined as acceptability of the recruitment and consent procedure, data collection tools, intervention content and delivery to participants, as well as compliance.
Patient and public involvement
We involved people living with dementia and their carers in the development of this research. This was achieved by collaborating with the ‘Caban group of dementia educators’, established and supported by the lead applicant’s research centre. The group raised a number of points for the team to consider, with ‘fear of using the internet’ being one area of concern. The group felt a person should be available to help people with iSupport. In response, we built in provision for an ‘e-coach’ to support participants randomised to receive iSupport. Coapplicant Hughes is a young adult carer for her father living with Vascular Dementia and felt the needs of young carers are often overlooked and neglected. She has contributed to the development of this research, especially the conceptualisation of the study design and suggestions for the delivery of WS4, and is assisting with this phase. We will meet with the CABAN group on a regular basis over the study duration, and at a previous meeting, we discussed how a visual participant information sheet could aid recruitment in line with dementia research standards45 and that using videoconferencing software would be preferrable to phone calls for arranging and conducting remote interviews. Feedback from this meeting was further referred to when drafting other study materials for consistency.
Ethics and dissemination
iSupport was granted ethical approval by Bangor University’s School of Medical and Health Sciences Academic Ethics Committee (AEC), reference number 2021-16915. All researchers are fully trained in the study procedures and receive regular supervision. A data management and monitoring plan ensure adherence to the principles of Good Clinical Practice and relevant regulations over the course of the study and to effectively audit the day-to-day conduct at each site. Carers will be provided with clear information and given time to ask questions and consider whether to participate before providing consent (online supplemental file 4). Through the content of our information sheets and consent forms, as well as contact with the research team, participants will understand that they can refuse to participate or withdraw at any time. Changes to the study protocol will be agreed by the funder and an ethics amendment submitted to the Academic Ethics Committee (AEC).
Our research products will include peer-reviewed academic papers, Plain English/Cymraeg Clir summaries of findings, articles for practitioner magazines and a project website. All academic outputs will conform to the reporting procedures in the relevant methodology guidelines (eg, Consolidated Standards of Reporting Trials e-health).46 Economic evaluation findings will be reported according to the recently updated Consolidating Health Economic Evaluation Reporting Standards (CHEERS) checklist, highlighting the role of Patient and Public Involvement and Engagement (PPIE) relating to health economics.47 We will present at conferences, conduct public and stakeholder events and produce policy briefings.
Our research activities will generate new versions of the iSupport platform for Welsh-language speakers, young carers and a UK-focused version with audio function. If our research shows iSupport is effective, health and care providers, pastoral care teams in schools and charitable organisations will be able to recommend an evidence-based online support service to dementia carers that will be publicly available for use at no cost. We hope this will improve policy and practice around delivering support to dementia carers. For example, UK health and social care could recommend the adapted versions of iSupport in their dementia guidelines. This could reduce demand on community teams at post/diagnosis and initial stages of dementia.
Forthcoming in 2022 in a related project, we will be working in partnership with community organisations to translate and adapt iSupport into three South-Asian languages (Urdu, Punjabi and Bengali) to ensure minority ethnic groups in the UK can also access the support in a way that is culturally appropriate for them.
Supplementary Material
Acknowledgments
The authors are extremely grateful to Professor Anne Magriet Pot, Erasmus School of Policy and Health Management, Erasmus University, the Netherlands for her inspiration and encouragement to seek funding for this project, the Caban Group for their thoughtful and useful insights and the research assistants (Danielle Proctor, Gwenllian Hughes, John Connaghan, Fatene Abakar Ismail) for piloting the case report forms and to Stéfanie Freel and Katrin Seeher of the WHO for their comments on the funding application and ongoing support for the project delivery.
Footnotes
Twitter: @PMasterson_80, @kat_algar
Contributors: GW leads the project and is responsible for study integrity. GW, JS, ZH, KE, PM-A, KA-S, RTE, CJ, PB and GH critically reviewed the study proposal and secured the research funding. JS, AS and KE lead collaboration sites. PM-A leads workstreams 2 and 4. RTE leads workstream 3. GF manages the study and led the ethics submission. NG is the trial statistician. DS advised on quality assurance. GW, JS, ZH, KE, PM-A, KAS, RTE, CJ, PB, GH, NG and DS contributed to the research protocol, provided edits and critiqued the manuscript for intellectual content.
Funding: This project is funded by the National Institute for Health Research (NIHR) Public Health Research programme (project reference NIHR130914).
Disclaimer: The views expressed are those of the authors and not necessarily those of the NIHR or the Department of Health and Social Care.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were involved in the design, or conduct, or reporting, or dissemination plans of this research. Refer to the Methods section for further details.
Provenance and peer review: Not commissioned; peer reviewed for ethical and funding approval prior to submission.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study involves human participants and was approved by School of Medical and Health Sciences Research Ethics Committee, Bangor University. Ref: 2021-16915. Participants gave informed consent to participate in the study before taking part.
References
- 1.World Health Organization . Global status report on the public health response to dementia, 2021. Available: https://www.who.int/publications/i/item/9789240033245
- 2.Wittenberg R, Hu B, Barraza-Araiza L. Projections of older people with dementia and costs of dementia care in the United Kingdom, 2019–2040: working paper. London: Care Policy and Evaluation Centre; 2019. https://www.alzheimers.org.uk/sites/default/files/2019-11/cpec_report_november_2019.pdf [Google Scholar]
- 3.Lewis F, Karlsberg S, Sussex J. Trajectory of dementia in the UK – making a difference: consulting report. London: Office of Health Economics; 2014. https://www.alzheimersresearchuk.org/wp-content/uploads/2015/01/OHE-report-Full.pdf [Google Scholar]
- 4.Gilhooly KJ, Gilhooly MLM, Sullivan MP, et al. A meta-review of stress, coping and interventions in dementia and dementia caregiving. BMC Geriatr 2016;16:106. 10.1186/s12877-016-0280-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bremer P, Cabrera E, Leino-Kilpi H, et al. Informal dementia care: consequences for caregivers' health and health care use in 8 European countries. Health Policy 2015;119:1459–71. 10.1016/j.healthpol.2015.09.014 [DOI] [PubMed] [Google Scholar]
- 6.Pinquart M, Sörensen S. Differences between caregivers and noncaregivers in psychological health and physical health: a meta-analysis. Psychol Aging 2003;18:250–67. 10.1037/0882-7974.18.2.250 [DOI] [PubMed] [Google Scholar]
- 7.McCabe M, You E, Tatangelo G. Hearing their voice: a systematic review of dementia family caregivers' needs. Gerontologist 2016;56:e70–88. 10.1093/geront/gnw078 [DOI] [PubMed] [Google Scholar]
- 8.World Health Organization . Global action plan on the public health response to dementia 2017–2025, 2017. Available: https://apps.who.int/iris/bitstream/handle/10665/259615/9789241513487-eng.pdf?sequence=1
- 9.Dickinson C, Dow J, Gibson G, et al. Psychosocial intervention for carers of people with dementia: what components are most effective and when? A systematic review of systematic reviews. Int Psychogeriatr 2017;29:31–43. 10.1017/S1041610216001447 [DOI] [PubMed] [Google Scholar]
- 10.Masterson-Algar P, Allen MC, Hyde M, et al. Exploring the impact of Covid-19 on the care and quality of life of people with dementia and their carers: a scoping review. Dementia 2022;21:648–76. 10.1177/14713012211053971 [DOI] [Google Scholar]
- 11.Egan KJ, Pinto-Bruno Ángel C, Bighelli I, et al. Online training and support programs designed to improve mental health and reduce burden among caregivers of people with dementia: a systematic review. J Am Med Dir Assoc 2018;19:200–6. 10.1016/j.jamda.2017.10.023 [DOI] [PubMed] [Google Scholar]
- 12.Godwin KM, Mills WL, Anderson JA, et al. Technology-driven interventions for caregivers of persons with dementia: a systematic review. Am J Alzheimers Dis Other Demen 2013;28:216–22. 10.1177/1533317513481091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gitlin LN, Marx K, Stanley IH, et al. Translating evidence-based dementia caregiving interventions into practice: State-of-the-Science and next steps. Gerontologist 2015;55:210–26. 10.1093/geront/gnu123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Peterson K, Hahn H, Lee AJ, et al. In the information age, do dementia caregivers get the information they need? Semi-structured interviews to determine informal caregivers' education needs, barriers, and preferences. BMC Geriatr 2016;16:164. 10.1186/s12877-016-0338-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Christie HL, Martin JL, Connor J, et al. eHealth interventions to support caregivers of people with dementia may be proven effective, but are they implementation-ready? Internet Interv 2019;18:100260. 10.1016/j.invent.2019.100260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hopwood J, Walker N, McDonagh L, et al. Internet-Based interventions aimed at supporting family caregivers of people with dementia: systematic review. J Med Internet Res 2018;20:e216. 10.2196/jmir.9548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pinto-Bruno Ángel C, Pot AM, Kleiboer A, et al. An online minimally guided intervention to support family and other unpaid carers of people with dementia: protocol for a randomized controlled trial. JMIR Res Protoc 2019;8:e14106. 10.2196/14106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mehta KM, Gallagher-Thompson D, Varghese M, et al. iSupport, an online training and support program for caregivers of people with dementia: study protocol for a randomized controlled trial in India. Trials 2018;19:271. 10.1186/s13063-018-2604-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Teles S, Ferreira A, Seeher K, et al. Online training and support program (iSupport) for informal dementia caregivers: protocol for an intervention study in Portugal. BMC Geriatr 2020;20:10. 10.1186/s12877-019-1364-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Baker JR, Jeon Y-H, Goodenough B, et al. What do children need to know about dementia? The perspectives of children and people with personal experience of dementia. Int Psychogeriatr 2018;30:673–84. 10.1017/S1041610217002022 [DOI] [PubMed] [Google Scholar]
- 21.National Institute for Health and Care Excellence (NICE) . Methods for the development of NICE public health guidance (3rd ed), 2012. Available: https://www.nice.org.uk/process/pmg4/resources/methods-for-the-development-of-nice-public-health-guidance-third-edition-pdf-2007967445701 [PubMed]
- 22.Chan A-W, Tetzlaff JM, Altman DG, et al. SPIRIT 2013 statement: defining standard protocol items for clinical trials. Ann Intern Med 2013;158:200–7. 10.7326/0003-4819-158-3-201302050-00583 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Join dementia research is funded by the Department of health and delivered by the National Institute for health research in partnership with Alzheimer Scotland, Alzheimer's research UK and Alzheimer's society. Available: www.joindementiaresearch.nihr.ac.uk [Accessed 10 Mar 2021].
- 24.Deeken F, Rezo A, Hinz M, et al. Evaluation of technology-based interventions for informal caregivers of patients with Dementia-A meta-analysis of randomized controlled trials. Am J Geriatr Psychiatry 2019;27:426–45. 10.1016/j.jagp.2018.12.003 [DOI] [PubMed] [Google Scholar]
- 25.Sugimoto T, Sozu T, Hamasaki T. A convenient formula for sample size calculations in clinical trials with multiple co-primary continuous endpoints. Pharm Stat 2012;11:118–28. 10.1002/pst.505 [DOI] [PubMed] [Google Scholar]
- 26.Sozu T, Sugimoto T, Hamasaki T. Sample size determination in clinical trials with multiple endpoints. Springer International Publishing, 2015. 10.1007/978-3-319-22005-5 [DOI] [Google Scholar]
- 27.Russell D, Hoare ZSJ, Whitaker R, et al. Generalized method for adaptive randomization in clinical trials. Stat Med 2011;30:922–34. 10.1002/sim.4175 [DOI] [PubMed] [Google Scholar]
- 28.Sörensen S, Pinquart M, Duberstein P. How effective are interventions with caregivers? an updated meta-analysis. Gerontologist 2002;42:356–72. 10.1093/geront/42.3.356 [DOI] [PubMed] [Google Scholar]
- 29.Kitwood T. Dementia reconsidered: the person comes first. UK: Open University Press, 1997. [Google Scholar]
- 30.Pot AM, Gallagher-Thompson D, Xiao LD, et al. iSupport: a WHO global online intervention for informal caregivers of people with dementia. World Psychiatry 2019;18:365–6. 10.1002/wps.20684 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Office for National Statistics (ONS) . 2011 census: key statistics for Wales, March 2011. section 10. proficiency in Welsh, 2012. Available: https://www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationestimates/bulletins/2011censuskeystatisticsforwales/2012-12-11#proficiency-in-welsh
- 32.Alzheimer’s Society . Caring for a person with dementia: a practical guide, 2002. Available: https://www.alzheimers.org.uk/get-support/publications-factsheets/caring-person-dementia-practical-guide
- 33.Elsevier Ltd . MACRO (Version 4.9.0.8594) [Computer software]. London; c2018. [Google Scholar]
- 34.Vasileiou K, Barnett J, Thorpe S, et al. Characterising and justifying sample size sufficiency in Interview-Based studies: systematic analysis of qualitative health research over a 15-year period. BMC Med Res Methodol 2018;18:148. 10.1186/s12874-018-0594-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ritchie J, Lewis J, Elam G. Designing and selecting samples. In: Ritchie J, Lewis J, eds. Qualitative research practice: a guide for social science students and researchers. London: SAGE Publications Ltd, 2003: 77–108. [Google Scholar]
- 36.Moore GF, Audrey S, Barker M, et al. Process evaluation of complex interventions: medical Research Council guidance. BMJ 2015;350:h1258. 10.1136/bmj.h1258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.O'Cathain A, Croot L, Duncan E, et al. Guidance on how to develop complex interventions to improve health and healthcare. BMJ Open 2019;9:e029954. 10.1136/bmjopen-2019-029954 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.May C, Finch T, Mair F, et al. Understanding the implementation of complex interventions in health care: the normalization process model. BMC Health Serv Res 2007;7:148. 10.1186/1472-6963-7-148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Brooke J. SUS: A ‘quick and dirty’ usability scale. In: Jordan PW, Thomas B, Weerdmeester BA, et al., eds. Usability evaluation in industry. London: Taylor Francis, 1996: 189–94. [Google Scholar]
- 40.Lancaster GA, Dodd S, Williamson PR. Design and analysis of pilot studies: recommendations for good practice. J Eval Clin Pract 2004;10:307–12. 10.1111/j.2002.384.doc.x [DOI] [PubMed] [Google Scholar]
- 41.Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77–101. 10.1191/1478088706qp063oa [DOI] [Google Scholar]
- 42.Pfadenhauer LM, Gerhardus A, Mozygemba K, et al. Making sense of complexity in context and implementation: the context and implementation of complex interventions (CICI) framework. Implement Sci 2017;12:21. 10.1186/s13012-017-0552-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Fenwick E, O'Brien BJ, Briggs A. Cost-effectiveness acceptability curves--facts, fallacies and frequently asked questions. Health Econ 2004;13:405–15. 10.1002/hec.903 [DOI] [PubMed] [Google Scholar]
- 44.Wiltsey Stirman S, Baumann AA, Miller CJ. The FRAME: an expanded framework for reporting adaptations and modifications to evidence-based interventions. Implement Sci 2019;14:58. 10.1186/s13012-019-0898-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Dementia Engagement and Empowerment Project (DEEP) . The DEEP-Ethics gold standards for dementia research. version 1.: innovations in dementia. Exeter, UK; 2020. https://www.dementiavoices.org.uk/wp-content/uploads/2020/07/The-DEEP-Ethics-Gold-Standards-for-Dementia-Research.pdf [Google Scholar]
- 46.Eysenbach G, CONSORT-EHEALTH Group . CONSORT-EHEALTH: improving and standardizing evaluation reports of web-based and mobile health interventions. J Med Internet Res 2011;13:e126. 10.2196/jmir.1923 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Husereau D, Drummond M, Augustovski F, et al. Consolidated health economic evaluation reporting standards 2022 (CHEERS 2022) statement: updated reporting guidance for health economic evaluations. Value Health 2022;25:3–9. 10.1016/j.jval.2021.11.1351 [DOI] [PubMed] [Google Scholar]
- 48.Bédard M, Molloy DW, Squire L, et al. The Zarit burden interview: a new short version and screening version. Gerontologist 2001;41:652–7. 10.1093/geront/41.5.652 [DOI] [PubMed] [Google Scholar]
- 49.Andresen EM, Byers K, Friary J, et al. Performance of the 10-item center for epidemiologic studies depression scale for caregiving research. SAGE Open Med 2013;1:205031211351457. 10.1177/2050312113514576 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Herdman M, Gudex C, Lloyd A, et al. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res 2011;20:1727–36. 10.1007/s11136-011-9903-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wagnild G. The Resilience Scale User’s Guide for the US English version of the Resilience Scale and the 14-item Resilience Scale (RS-14). Worden, MT: The Resilience Center; 2009. [Google Scholar]
- 52.Spitzer RL, Kroenke K, Williams JBW, et al. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med 2006;166:1092–7. 10.1001/archinte.166.10.1092 [DOI] [PubMed] [Google Scholar]
- 53.Annear MJ, Toye C, Elliott K-EJ, et al. Dementia knowledge assessment scale (DKAS): confirmatory factor analysis and comparative subscale scores among an international cohort. BMC Geriatr 2017;17:168. 10.1186/s12877-017-0552-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Hoefman RJ, Van Exel NJA, Brouwer WBF. iMTA valuation of informal care questionnaire (iVICQ). version 1.0. Rotterdam: iBMG / iMTA; 2011. [Google Scholar]
- 55.Spruytte N, Van Audenhove C, Lammertyn F. The scale for the quality of the current relationship. internal report. Leuven: LUCAS-KULeuven, 2000. [Google Scholar]
- 56.Mulhern B, Rowen D, Brazier J, et al. Development of DEMQOL-U and DEMQOL-PROXY-U: generation of preference-based indices from DEMQOL and DEMQOL-PROXY for use in economic evaluation. Health Technol Assess 2013;17:1–140. 10.3310/hta17050 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2022-064314supp001.pdf (617.7KB, pdf)