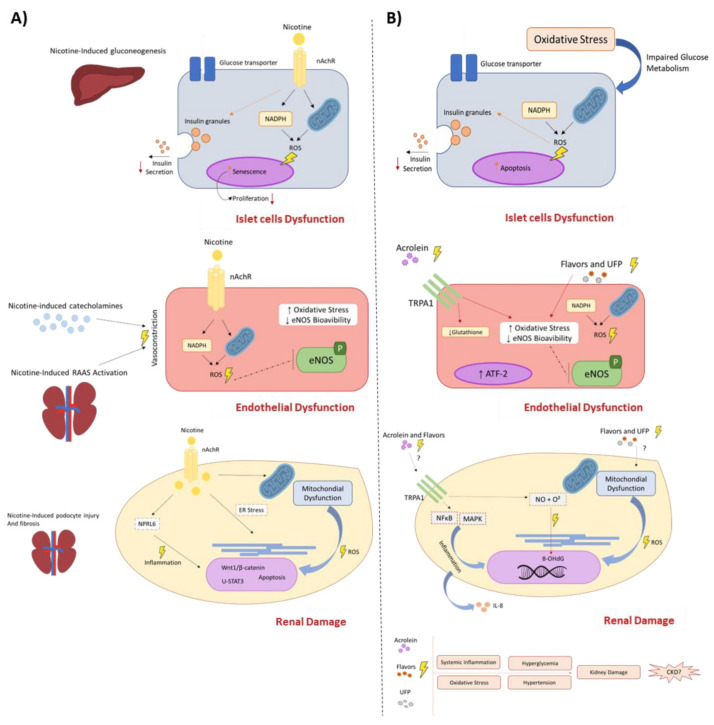
Figure 1.
Potential cellular and molecular mechanism triggered by nicotine and compounds generated by ENDS and their role on CKD pathophysiology. ENDS release several chemical compounds, including nicotine, ultrafine particles, flavoring, and other harmful and potentially harmful constituents generated by thermal degradation. Thus, these compounds are absorbed by the lungs and reach systemic circulation to exert their toxicity and favor the onset of CKD and its related disorders. Although the harmful and direct effects of nicotine are well known and reported in clinical and experimental studies (A), other xenobiotics released by ENDS, such as acrolein, ultrafine particles (UFP), and flavorings possess the potential to trigger deleterious effects, leading to cumulative damages and favor CKD onset (B), however further data are required. The direct interaction of tobacco-released compounds with the endothelium increase reactive oxygen species (ROS), decreases endothelial nitric oxide species (eNOS) [73,74,126,127,128,129,170] and leads to an inflammatory response mediated or not by nicotinic receptor activation (nAChRs) or stress sensors receptors (TRPA1) [75,123,124,125,146,147], evoking endothelial dysfunction, impaired vascular relaxation, and increasing blood pressure. Directly or indirectly, these xenobiotics can impair glucose metabolism by affecting β islet cell homeostasis [85,86,90] and mitochondrial function in an ROS-dependent manner, culminating in insulin resistance and Diabetes Mellitus type II onset [95,100,135]. Finally, the kidneys are affected by the systemic inflammatory response, increased blood pressure, and higher levels of ROS, which increase mesangial cell proliferation, activate programmed cell death pathways on tubular cells, and impair mitochondrial function [109,110,111,112,113,114,115,135,136,137]. Once the kidneys are responsible for filtration, these xenobiotics accumulate on renal structures and cause inflammation and oxidative stress. Altogether, these mechanisms decrease glomerular filtration rate (GFR) and kidney function, leading to the late establishment of CKD.