Abstract
Background
The issue around vaccination of children has brought divergent opinions among the populations across the globe and among the Arab population. There has been a low response rate to the calls for vaccination of children and this is reflective of the sentiments which parents may have towards their children being vaccinated. This study aims to explore the parents’ health beliefs, intentions, and strategies towards the COVID-19 vaccine for their children among Arab population.
Methods
A cross-sectional study using an online survey from October to December 2021, was carried out in five Arab countries in the Middle East. A reliable health belief model (HBM) including five domains: severity, susceptibility, benefits, barriers and cues to action, was adopted. Chi-square, Mann–Whitney test, and multivariable logistic regression were performed for data analysis.
Results
The survey response rate was 58 % (1154/2000). Only 56 % of Arab parents are intended to vaccinate their children against COVID-19. The mean scores of parental health belief are largely driven by their concern over the vaccine’s side effect (p = 0.001) followed by its efficacy, safety (p < 0.001), and scheduling difficulty (p = 0.029). However, strategies that were statistically encouraged parents to vaccinate their children included doctor’s recommendation, adequate information being provided, and acceptance of the vaccine by public (p < 0.001). Parents with one child were almost three times most likely to vaccinate their children (OR = 2.660, 95 %CI = 1.572–4.504, p < 0.001). Parents' desire to vaccinate their children is also influenced by other factors such as job loss owing to COVID-19 and the presence of a health worker in the family.
Conclusion
Intention of Arab parents to vaccinate their children via COVID-19 vaccine is still limited. Thus, it is essential for health care authorities to avail the information which will debunk the erroneous beliefs which some parents have developed towards the vaccination of children against COVID-19.
Keywords: COVID-19, Vaccination, Intention, Children, Parents
1. Introduction
When the COVID-19 pandemic broke out the fatality level was high and there was need for urgent medical solutions to curb the disease [1]. The pandemic broke out in a sudden method and the health sector worldwide had no facilities to cater to the treatment of this disease so contingency measures were placed. Some of these contingency measures were the abrupt closure of non-essential businesses and schools, social distancing, wearing of masks and increased hand sanitization at entry and exit points of buildings [2]. In the hospitals, medications such as dexamethasone and oxygen therapy were used to treat critically ill patients. When the COVID-19 virus showed high levels of fatality, the formulation of vaccines was abruptly undertaken to provide protection from future infections with the virus [3].
The Arab population has been affected severely by the COVID-19 pandemic; with >2.2 million people being infected by the virus. Both adults and the younger people in the Arab countries have been infected with COVID-19 which has prompted the healthcare sector and local authorities to place measures to contain the virus and reduce the mortality rate. According to previous literature studies, studies of Rosen et al., [4] and Muhsen & Cohen [5], it has been reported that the rates of vaccination are still low which points towards the resistance and hesitance to be vaccinated [4], [5]. For example, only 16 % of children aged between 12 and 15 have been vaccinated, which shows the low vaccination rates among the younger population. The level of compliance has been compromised by some of the health beliefs and perceptions of how the phenomenon of the disease should be treated in particular [5].
Initially, vaccination against the COVID-19 vaccine was only suitable for adults and severe ill patients [6]. However, with the recent emerge of different variants of COVID-19 including delta and omicron variant, world health organization (WHO) and Centers for Disease Control and Prevention (CDC) have recommended that every one ages 5 years and older get a COVID-19 vaccine to help protect against COVID-19 [7]. Pfizer BioNTech COVID-19 vaccine is the vaccine which was first approved for emergency use in children aged between 5 and 15. COVID-19 vaccines for children between 5 and 11 were availed from November 2021 [8]. As of this writing, some people still believe that the rate of COVID-19 infection in children is minimal. However, current data suggests otherwise [9]. >8,300 COVID-19-related hospitalizations and about 100 COVID-19-related deaths have been documented in children aged 5 to 11 years as of mid-October 2021 [10]. One of the leading causes of death in children between the ages of 5 and 11 is COVID-19. Multisystem inflammatory syndrome (MIS-C), an illness in which numerous body components such as the heart, lungs, kidneys, brain, skin, eyes, or digestive organs become inflammatory, can occur in children infected with COVID-19. Since the outbreak of the pandemic, there have been >2,300 cases of MIS-C in children aged 5 to 11 years. COVID-19 is more likely to induce severe illness in children with preexisting medical disorders than it is in those who don't [10], [11].
Vaccination among children is a common issue, with some vaccinations performed at birth and other vaccines administered in the subsequent months of their early life [12]. This stresses that the concept of vaccination among children is a notion which parents are highly familiar with. However, when it comes to the vaccination of children against the COVID-19 virus, the parents have been highly hesitant towards this initiative [13]. This hesitancy has been traced to various origins; ranging from inadequate evidence of the efficacy of vaccines to the lack of time and facilities to undergo the vaccination process with their children [14].
Predominant parents’ health beliefs have been displayed in the vaccination of children against the COVID-19 virus. Some parents do not fully believe that the vaccination will protect their children thus it may be unnecessary [15]. There is also suspicion on the long terms effects of the vaccine in children, with several unconfirmed reports implying that the vaccination would have a negative effect on the future health and livelihood of the children [16], [17]. Up to date, Parents in the Arab world who choose or refuse to vaccinate their children face a knowledge gap that has yet to be bridged. As a result, recognizing the intent to vaccinate early is a crucial step in developing efforts to enhance COVID-19 vaccine uptake. The current study aimed to evaluate parental health beliefs of Arabs and their intention towards vaccination their children against COVID-19 and determine the factors, barriers, and strategies that have a significant role in influencing parents’ decision to vaccinate their children.
2. Methods
2.1. Study design and population
A quantitative, cross-sectional study was conducted in five Arab countries in the Middle East including Iraq, Jordan, United Arab Emirates, Oman, and Yemen. These countries were selected as a sample of Arab population as their societies have various cultures, habits, and beliefs [18] so that a general insight about their people’s health belief and intention to vaccinate their children against COVID-19 can be formed. There were no previous analogous studies conducted in Arab countries, so it was assumed that answers and response rates would be 50 percent for the majority of the primary questions. The sample size was calculated based on this assumption. The Raosoft® sample size calculator was used with a 5 % error margin, a 95 % confidence interval, and a 50 % expected response [19]. The minimum sample size estimated for the study was 385.
2.2. Inclusion and exclusion criteria
The included study population consisted of adult parents (fathers and mothers aged ≥ 18 years old) who are Arab and have at least one child aging between 5 and 17 years old. Parents, who a) are not Arab; b) don’t have any child; c) are working or studying in the medical field; and d) were with cognitive impairment such as unable to think, read and pay attention, were excluded from this study.
2.3. Study instrument
The study instrument was developed after conducting a literature assessment of similar studies. The study questionnaire was adapted from previously used, validated surveys based on the literature search, and its applicability was ensured [20]. The face and content validity of the adapted questionnaire were established by a research group from the selected Arab countries. The questionnaire was translated from English into Arabic and then reverse-translated. Both forward and backward translations were verified for accuracy and meaning, and any requested changes were debated before being approved. There were 20 Arab parents who completed the questionnaire to ensure that it was easy for them to understand while still providing correct information. The questionnaire consisted of sociodemographic characteristics of the study population and health belief models (HBM). Age, race, marital status and primary residence were some of the demographic variables gathered from participants. As part of our research, we looked into if any members of the household were involved in the healthcare sector, whether they had contracted COVID-19, and whether or not they had been affected by the pandemic in any way. Children’s characteristics were limited to how many children they have in the household and whether they had any chronic health conditions. The HBM components were tested using previously used items that matched our study. HBM is a method for identifying vaccine uptake parameters that can be improved. In order to better understand and predict health-related behaviours, the HBM was developed as a social- and psychological-based health behaviour change model. It is including several statements assessed perceived susceptibility (three items), perceived severity (three items), perceived benefits (two items), perceived barriers (five items), cues to action (four items) and intention (one item) (Supplementary Appendix 1). All constructs were measured on a 5-point Likert scale from strongly disagree (1) to strongly agree [5].
2.4. Data collection procedure
Data collection was performed online using the SurveyMonkey® platform for two months from October to December 2021. Participation was recruited anonymously via snowballing sampling technique and the call for participation was made on social media. We utilized several strategies to reach as many respondents as possible all over each of the selected Arab country within the data collection period. This included relying on professional and personal networks of the researchers, reaching out to community leaders and social media influencers to broadcast and share the survey. Two main platforms used in disseminating this survey were social media (Facebook®, Twitter® and Instagram®) and WhatsApp®. Facebook® and WhatsApp® were selected as two of the most popular communication and social platforms among Arab population. While Twitter® and Instagram® are more popular among the younger generation. A standardized general description about the survey was given in the WhatsApp message/social media postings before the link was provided to both English and Arabic language versions of the questionnaire. Two thousand participants (an average 400 parents from each selected country) were invited; however, only 1627 agreed to participate in the study. Three reminders were sent out to participants in a 3-week interval to enhance response rates. 473 participants did not complete answering 50 % of the questionnaire items so that their responses were excluded. The final number of participants who completed answering the survey was 1154 participants. All information collected from the study was anonymized and kept confidential.
2.5. Data analysis
Total responses collected from the questionnaires were encoded and analysed using IBM Statistical Package for the Social Sciences (SPSS) software version 26.0. Statistical methods such as descriptive and inferential statistics were used to examine the collected data and draw conclusions. All variables were subjected to descriptive statistics. For categorical variables, we used numbers and percentages, whereas for continuous variables, we used the mean and standard deviation. The Kolmogorov–Smirnov test of normality was used to determine the shape of the distribution in inferential data. Homogeneity among the participants was confirmed using Leven’s test where the equal variances assumed as the p value was >0.05. HBM constructs were generated by averaging the scores of each HBM construct's component elements, with a greater score suggesting a higher level of awareness. The links between groups were examined using the Chi-square test of independence. Analysis of categorical and continuous variables was done using logistic regression and the Mann–Whitney test. P-values 0.05 were considered statistically significant. Univariable and multivariable logistic regressions were used to examine the variables related with the intention to vaccinate. A purposeful selection process was utilized based on a univariable analysis for each variable. We based our multivariable analysis on the Wald test from logistic regression.
3. Results
3.1. Socio-demographic characteristics of respondents
Among the Arab parents who participated in the survey, the majority were mothers (57.98 %) with 3 and more children (58.23 %) and they were predominantly married (91.59 %). Table 1 reported that there is a statistically significant relationship between gender and education level with the intention of the parents to have their children vaccinated. Majority of the parents (80.76 %) reached up to tertiary level of education and live in urban residences (78.94 %). Among the parents with no intention to have their children vaccinated, just over a third of them (36.83 %) have had someone in their household previously infected with COVID-19 than those who have the intention to have their children vaccinated (49.57). Parents with more healthcare workers in their family (40.81 %) expressed statistically significant intention to vaccinate than those with fewer healthcare workers in their family (27.56 %) as shown in Table 1.
Table 1.
Demographic characteristics of parents in relation to intention to vaccinate their children (n = 1154).
| Variables | Total, n(%) | Intention, n(%), 646 (56) | No intention, n(%), 508 (44) | P-value# |
|---|---|---|---|---|
| Age | ||||
| Mean (SD) : 37.32 (10.75) | ||||
| 18-30 | 331 (28.68) | 195 (16.90) | 136 (11.79) | 0.223 |
| 31-40 | 382 (33.10) | 201 (17.33) | 181 (15.68) | |
| <40 | 441 (38.21) | 250 (21.66) | 191 (16.55) | |
| Gender | <0.01* | |||
| Male | 485 (42.02) | 309 (26.78) | 176 (15.25) | |
| Female | 669 (57.98) | 337 (29.20) | 332 (28.77) | |
| Marital Status | 0.315 | |||
| Married | 1057 (91.59) | 587 (50.87) | 470 (40.72) | |
| Single/separated/divorced/widowed | 97 (8.41) | 59 (5.11) | 38 (3.29) | |
| Educational Level | ||||
| Primary | 8 (6.93) | 0 (0) | 8 (6.93) | 0.003* |
| Secondary | 142 (12.31) | 74 (6.41) | 68 (5.89) | |
| Tertiary | 1004 (80.76) | 572 (49.57) | 432 (37.44) | |
| Primary Residence | ||||
| Urban | 911 (78.94) | 522 (45.23) | 389 (33.71) | 0.08 |
| Rural | 243 (21.06) | 124 (10.75) | 119 (10.31) | |
| Does your Child have any chronic health condition | ||||
| Yes | 87 (7.54) | 36 (3.12) | 51 (4.42) | 0.004* |
| No | 1067 (92.46) | 610 (52.86) | 457 (39.60) | |
| Have you lost your Job due to the COVID-19 pandemic | ||||
| Yes | 152 (13.17) | 97 (8.41) | 55 (4.77) | 0.037* |
| No | 1002 (86.82) | 549 (47.57) | 453 (39.25) | |
| Do you have any Healthcare workers among the household | <0.01* | |||
| Yes | 789 (68.37) | 471 (40.81) | 318 (27.56) | |
| No | 365 (31.63) | 175 (15.16) | 190 (72.44) | |
| Anyone in the household has been infected with COVID-19 infection | <0.01* | |||
| Yes | 952 (82.50) | 572 (49.57) | 425 (36.83) | |
| No | 202 (17.50) | 119 (10.31) | 83 (7.19) | |
| Number of children in the household | 0.005* | |||
| 1 | 195 (16.90) | 97 (8.38) | 98 (8.49) | |
| 2 | 287 (24.87) | 146 (12.65) | 141 (12.22) | |
| 3 or more | 672 (58.23) | 403 (34.92) | 269 (23.31) |
#Pearson Chi-Square.
*Statistically significant (p > 0.05).
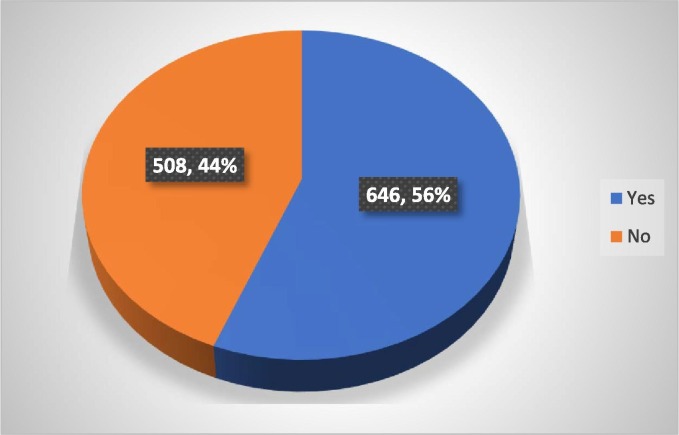
Additionally, among the 1154 Arab parents who participated in the study, 646 (56 %) indicated a positive response towards vaccination of their children while 508 (44 %) responded that they are unwilling to have their children vaccinated against the COVID-19 virus (Fig. 1 ).
Fig. 1.
Parents' intention to vaccinate their children.
3.2. Health belief models of parents toward vaccination their children
The parents expressed varying perceptions regarding the vaccination of their children (Table 2 ). Predominantly, parents expressed uncertainty on whether their children being susceptible to infection from the virus (58.1 %) and only a minority (2.1 %) can strongly agree that they think their children are susceptible to being infected. On the contrary, the majority of the parents are worried about their children’s susceptibility to the virus (58 %). The parents’ perception of the severity of COVID-19 among children is scattered, with only a quarter (25.2 %) believing that the complications are severe. Despite the hesitation towards vaccination, nearly half of the parents believe the vaccination would benefit their children (42.40 %) and decreases their likelihood of suffering from complications associated with the virus (44.40 %).
Table 2.
Perception of susceptibility, severity, and benefits of parents in relation to vaccinate their children (n = 1154).
| Health Belief Model Constructs |
Strongly Disagree n(%) |
Disagree n(%) |
Uncertain n(%) |
Agree n(%) |
Strongly Agree n(%) |
|---|---|---|---|---|---|
| Perception of susceptibility | |||||
| My child/children’s chance of getting Coronavirus in the next few months is high. | 83 (7.2) |
188 (16.3) |
670 (58.1) |
189 (16.4) |
24 (2.1) |
| I am worried about my child/children’s likelihood of getting the Coronavirus. | 71 (6.2) | 201 (17.4) | 143 (12.4) | 588 (51.0) | 151 (13.1) |
| Getting the Coronavirus is currently a possibility for my child/children. | 61 (5.3) | 221 (19.2) | 360 (31.2) | 458 (39.7) | 54 (4.7) |
| Perception of severity | |||||
| Complications from the Coronavirus infections are serious. |
32 (2.7) | 76 (6.6) | 175 (15.2) | 580 (50.3) | 291 (25.2) |
| My child/children will be very sick if he/she gets the Coronavirus. | 51 (4.4) | 21.3 (18.5) | 445 (38.6) | 333 (28.9) | 112 (9.7) |
| I am afraid of my child/children getting the Coronavirus. | 42 (3.6) | 103 (8.9) | 126 (10.9) | 610 (52.9) | 273 (23.7) |
| Perception of benefits | |||||
| Vaccination for children is a good idea because it makes me feel less worried about my child/children catching the Coronavirus. | 135(11.7) | 137 (11.9) | 170 (14.7) | 487 (42.2) | 225 (19.5) |
| Vaccination decreases my child/children’s chance of getting the Coronavirus or its complications. |
122(10.6) | 79 (6.8) | 215 (18.6) | 512 (44.4) | 226 (19.6) |
Moreover, the parents acknowledge various barriers and action cues in relation to the vaccination of their children. The efficacy of the COVID-19 vaccine for children is a crucial factor driving intention, with feelings of uncertainty (19.8 %) and great concern (35.7 %) surrounding it. Scheduling a vaccination date for their children is not a significant barrier, as only about a third (33.2 %) indicate challenges in doing so. Over half of the parents (52.3 %) intend to have their children vaccinated when they gain enough information about the vaccine. Despite the general public taking the vaccine, about a third of the parents would still not consider having their children vaccinated (32.4 %). However, nearly half of the parents indicate that they will agree to have their children vaccinated when it is either required by the school their children attend (49.0 %) and over half of the parents will agree to vaccination when it has been recommended by their doctor (63.8 %). The results are shown in Table 3 below.
Table 3.
Perception of barriers and action cues of parents in relation to vaccinate their children (n = 1154).
| Health Belief Model Constructs |
Strongly Disagree n(%) |
Disagree n(%) |
Uncertain n(%) |
Agree n(%) |
Strongly Agree n(%) |
|---|---|---|---|---|---|
| Perception of barriers | |||||
| I am concerned about the efficacy of the COVID-19 vaccine for children. |
69 (6.0) | 230 (19.9) | 229 (19.8) | 412 (35.7) | 214 (18.5) |
| I am concerned about the safety of the COVID-19 vaccine for children. |
67(5.8) | 187 (16.2) | 270 (23.4) | 404 (35.0) | 226 (19.6) |
| I am concerned about the affordability of the COVID-19 vaccine. | 206(17.9) | 321(27.8) | 274 (23.7) | 264 (22.9) | 89 (7.7) |
| I am worried about the possible side-effects of the COVID-19 vaccine for my child/children. |
41 (3.6) | 128 (11.1) | 194 (16.8) | 537 (46.5) | 254 (22.0) |
| I am concerned I will not be able to schedule the vaccination for my child/children. |
152 (13.2) | 332 (28.8) | 286 (24.8) | 311 (26.9) | 73 (6.3) |
| Cues to action | |||||
| I will consider my child/children taking the COVID-19 vaccine only if I am given adequate information about it. |
94 (8.1) | 149 (12.9) | 155 (13.4) | 604 (52.3) | 152 (13.2) |
| I will consider my child/children taking the COVID-19vaccine if the general public takes it. | 110 (9.5) | 264 (22.9) | 187 (16.2) | 504 (43.7) | 89 (7.7) |
| I will consider my child/children taking the COVID-19 vaccine if it is required by the school. |
116 (10.1) | 255 (22.1) | 218 (18.9) | 482 (41.8) | 83 (7.2) |
| I will consider my child/children taking the COVID-19 vaccine if it is recommended by his/her doctor. |
94(8.1) | 154 (13.3) | 170 (14.7) | 553 (47.9) | 183 (15.9) |
3.3. Factors associated with parents’ intention to vaccinate their children
For a deeper insight into the factors associated with the parents’ intention to have their children vaccinated, univariable logistic regression outputs were evaluated (Table 4 ). Parents’ perception of susceptibility, severity, benefits, barriers and cues to action were significantly associated with parents’ intention to vaccinate their children The odds of perceived barriers were more likely to influence. parents’ decision to vaccinate their children (OR = 1.304; 95 %CI = 1.192–5.731, p < 0.001), followed by perceived susceptibility (OR = 0.786; 95 %CI = 0.489–0.943). Parents who lost their jobs due to COVID-19 and with healthcare workers on their family had more significantly impact on parents’ intention to vaccinate their children respectively (OR = 0.152, 95 %CI = 0.078–0.293, P=<0.001; OR = 0.621 95 %CI = 0.406–0.949, P = 0.022). Parents with one child were almost three times most likely to vaccinate their children compared to their reference group (OR = 2.660, 95 %CI = 1.572–4.504, p < 0.001).
Table 4.
Logistic regression of factors significantly associated with parents’ intention to vaccinate children against COVID-19.
| Variables | OR (95%) | P-Value |
|---|---|---|
| Perceived susceptibility items | 0.786 (0.489-0.943) | 0.003 |
| Perceived severity items | 0.590(0.429-0.811) | 0.001 |
| Perceived benefits items | 0.124(0.088-0.175) | >0.001 |
| Perceived barriers items | 1.304(1.192-5.731) | >0.001 |
| Cues to action items | 0.248(0.179-0.343) | >0.001 |
| Job loss due to the COVID-19 pandemic (Ref. No) | ||
| Yes | 0.152(0.078-0.293) | <0.001 |
| Healthcare worker among the household (Ref. No) | ||
| Yes | 0.621(0.406-0.949) | 0.022 |
| Number of children (Ref. three children or more) | ||
| 1 | 2.660(1.572-4.504) | >0.001 |
| 2 | 2.399(1.504-3.826) | >0.001 |
For more insights into the perceived barriers and cues to action, the means scores (MS) between the parents with intention and parents with no intention to vaccinate their children against Covid-19 were gathered and analysed (Table 5 ). Parents who were unwilling to vaccinate their children had statistically significant concerns on vaccine’s side effects (MS = 3.72) followed by efficacy and safety respectively (MS = 3.46 and 3.41). Scheduling difficulty was also one of the significant main barriers that might prevent the parents from vaccine their children (MS = 2.84). On the other hand, strategies that are most significantly motivated parents to vaccinate their children are doctor’s recommendation and adequate information being provided (p < 0.05). General public accepting the vaccine and school district requirement were other factors that have significant effect on parents’ intention to vaccinate their children. The results are shown in Table 5 below.
Table 5.
Perceived barriers and cues to action in relation with intention for parents to vaccinate their children (n = 1154).
| Items | Overall scale scores mean (SD) | P-value |
|---|---|---|
| Perceived Barriers | ||
| Safety | 3.41(1.17) | >0.001* |
| Efficacy | 3.46(1.14) | >0.001* |
| Affordability | 2.75(1.21) | 0.940 |
| Side effects | 3.72(1.03) | 0.001* |
| Scheduling difficulty | 2.84(1.15) | 0.029* |
| Cues to actions | ||
| Adequate information provided | 3.46(1.15) | >0.001* |
| General public accepting the vaccine | 3.14(1.18) | >0.001* |
| School district requirement | 3.07(1.18) | >0.001* |
| Doctors’ recommendation | 3.47(1.17) | >0.001* |
*Statistically significant (p < 0.05).
4. Discussion
This cross-sectional survey is the first of its kinds to be carried out in multi-Arab countries to have a clear insight on Arab parents with different cultural and background toward vaccinating their children against Covid-19. The outcomes of this study can help to prepare for the wide dissemination required for a successful vaccination program against Covid-19 among Arab societies. It is known that Arab Parents have been expressing varied perceptions on the issue of whether or not their children should be vaccinated against the COVID-19 virus [21]. This stems from the uncertainty and the safety of the vaccines and the potential effects which they have on the children. It is rare to come across parents who have hesitated to question the safety and risks associated with the other vaccinations which children have to take. For the minority of the population which does not believe in vaccination; it is often driven by religious beliefs and personal preferences [22]. However, it must be noted that these parents would typically have other alternatives to vaccination usually in herbal form, thus the concept of vaccination is maintained. Thus, when it comes to vaccination against COVID-19, based on a previous study, it has proven to be a problematic issue among parents; fueled by their health beliefs, perceptions and strategies towards their children [23].
4.1. Parental intention and benefit to vaccinate their children
In the current study, just under half of the parents have indicated that they have no intention to have their children vaccinated, which indicates quite a significant number of parents who are currently against the vaccination of their children among Arab population. This is consistent with findings of previous studies in Greek, Chicago, and Saudi Arabia where parents also showed a critical concerns regarding Covid-19 vaccine for children [24], [25], [26]. This is because some parents are suspicious of the vaccine's ability to protect their children, therefore they feel it may be pointless for them to be vaccinated. There is also concern over the long-term consequences of the vaccine on children, with multiple unsubstantiated reports claiming that the vaccine would have a severe impact on the children's future health and economic well-being [20]. In a contrast, around 56 % of participated parents showed an intention in vaccinating their children, and this is similar to other studies which reported the proportion of parents’ that intend to vaccinate their children ranges from 48 % to 60.4 % [27], [28], [29].
Despite the hesitation and reluctance to have their children vaccinated parents have agreed that the vaccines hold benefits for their children. One of the benefits which the parents have acknowledged is the protection against infection with the virus. Parents recognize that by being vaccinated, their children’s chances of being infected with the virus are significantly lowered [22]. This is supported by the mechanism by which vaccines work; as they prepare the body to fight a known illness in a lower dosage so that when future infection occurs; the immune system is more prepared and ready to conquer the illness. Primarily, vaccines would prevent severe illness and death in patients who have been vaccinated. In the study of Goldman et al., (2021) and Alfieri et al., (2021), similar sentiments where expressed as parents collectively agreed that vaccination of their children would provide them with assurance over the safety of their children from being infected [25], [30]. However, recent studies by Yigit et al., (2021) indicate that this notion is being challenged by the news of new variants which are emerging [31]. At first, it was the delta variant which was identified and now it is the Omicron variant which has been recently discovered. As the new variants are emerging, the efficacy of the vaccines is being questioned and this can reduce the confidence which parents have over their children have in being vaccinated; if new variants emerge [32].
4.2. Vaccine intention-related factors
Our findings demonstrated that the presence of healthcare workers within the household is a factor which influences the intention of parents towards having their children vaccinated. This can be driven by the presence of information which drives them to actively intend to have their children vaccinated. This is reflected in the studies of Dyder et al., (2020) and Bell et al., (2020) which suggested that when people have adequate information over health issues, they are more likely to be compliant with the recommended course of action. On the contrary the lack of information often results in misinformation and biases towards approved means of treatment [13], [33], [34].
The incidence of COVID-19 within the household has been an essential factor which drives the parent’s intention to have their children vaccinated. People who have lived in close proximity with infected individuals can attest to the severity of the disease and how it can lead to death. This is in contrast to people who up to date have not had anyone in close proximity get infected with the disease and become severely ill. Therefore, mainly people who have someone in their household previously infected are more wary if the disease and keen to be vaccinated promptly; together with their children. These notions are similarly expressed by Wilder-Smith & Qureshi (2020) and Domnich et al., (2020), who note that the incidence of COVID-19 in a household prompted a higher level of alertness and pro-vaccine activists being more assertive [35], [36].
Moreover, the number of children within the household is also another significant factor which drives the intention to have the children vaccinated. Each child is a potential contact person for the virus, and the more children in the household lead to the increased likelihood of children being carriers of the virus. Typically, people with one or two children only would try to safeguard their children by limiting their movements, yet those with more children would potentially fail to do so if they attempted it. Therefore, vaccination would be a tool by which they can safeguard their children’s safety and reduce the incidence of infection and spread within the household, which is consistent with the findings of Ganzak et al. (2020) [37].
Among the respondents of the survey were parents who had children with underlying medical conditions, and this has been identified as a significant factor in the intention to have children vaccinated. Parents are concerned with how their children with underlying health conditions would fare in the event that they have been vaccinated. Ever since the pandemic broke out, it has been noted and even reported that the disease would be more severe in people with underlying conditions such as diabetes, hypertension, obesity, heart and other respiratory conditions such as asthma [38]. This notion is reflected in the study of Barnejee et al., (2020), where it was noted that the parents of children with asthma have been highly reluctant in having their children vaccinated [39]. Managing asthma in children is problematic as it requires the parent to really study the severity of the illness in their children and minimize any other interfering factors as much as possible; especially those surrounding the children’s respiratory system. Therefore, with the complexity of COVID-19 and its effect on the respiratory system; parents with children with underlying conditions are less eager to have their children vaccinated to avoid further straining their children [40].
4.3. Parents’ barriers to vaccinate their children
The safety of vaccines has proven to be one of the critical factor which Arab parents are concerned about; given the rapid time in which the vaccines were formulated. Typically, it takes several years for a vaccine to be formulated and approved [41]. This amount of time taken is used for the development of the vaccine, where it is subjected to various clinical trials and its efficacy is tested. The time would also be taken to analyse the potential adverse effects which the virus has and how they can be effectively treated [42]. However, the first COVID-19 vaccine was developed in just nine months after the onset of the pandemic [43]. Before the first vaccine was developed, there was no existing vaccination against coronaviruses for human, thus it was a new innovation. Therefore, there have been high levels of skepticism towards the authenticity of vaccines which have been developed in a shorter amount of time, which is a concept that has been extensively discussed in the previous studies [44], [45]. However, the vaccines were tested rigorously and millions of people have been vaccinated safely thus this can debunk the misconceptions surrounding the safety of the vaccines.
Parents have also indicted concern over the potential adverse side effects which the vaccines would have on children. Due to their young age, younger children are often more vulnerable to severity of infections and illnesses [46]. Therefore, the illnesses and symptoms which adults survive may have fatal effects on young children. This is partly contributed to by the fact that the children’s immune system would still be developing [47]. Therefore, parents are concerned on whether their children would survive the typical side effects of the vaccines which include fever, body aches and a sore arm. As explained in the study of Lai et al., (2021) and Su et al. (2021), parents would be worried that the fever would not easily go away and develop into serious cases and body aches would become more severe [48], [49]. In other instances, there are no substantial fears which the parents would have but would be largely skeptical on the reported side effect of vaccines. Most of the reported effects are largely a natural response of the immune system that it has identified the virus and is fighting against it, rather than indicating an actual illness [50]. Therefore, with this uncertainty over the potential adverse effects of the vaccine on their children’s wellbeing, most parents have been unwilling to have their children vaccinated.
4.4. Parental vaccine intention-related strategies
Our results found that one of the cues action that play a significant role in motivating Arab parents to vaccinate their children is the provision of adequate information. It is undeniable that the origins and progression of the COVID-19 virus has been clouded with different information which can leave one with an uncertain picture of the disease [51]. While some of the information has been verified and it backed by scientific data, there is another pool of information regarding the virus which is largely driven by suspicion and conspiracy theories; which is similarly expressed by recent published literature studies [52], [53]. This has caused some people to lose confidence in any form of treatment and vaccination, so they are afraid that it would negatively affect them. Similarly, parents with inadequate information about the vaccines are reluctant to have their children vaccinated. It is essential for the healthcare workers and authorities to ensure that there is transparency and wider availability of information on the vaccines [54]. When the parents have adequate information about vaccination, they can make informed decisions which will protect their children and their communities in the long run. This information can be provided by healthcare workers as they engage the parents on how vaccination can be beneficial to the children too.
Nonetheless, the issue of vaccination in children among parents is also affected by the need to return to normalcy, which is consistent with the findings of previous studies [55], [56]. For parents with children, part of the normalcy which they desire is for children to go back to attending school physically. As a means to contain the spread of the virus, schools had been shut down and the children had to rely on virtual forms of learning [57], [58]. While this was a measure which ensured continuity among the children and minimized the level of disruption to their learning, many parents have expressed their eagerness to have their children attend school as before [55]. Therefore, the parents who are reluctant to have their children vaccinated have indicated that in the event that their children’s school requires mandatory vaccination, they would have their children vaccinated. Therefore, if the schools leave vaccination as an optional requirement lesser children would be vaccinated but if it were mandatory more children would be vaccinated, which is consistent with the findings of Zimmerman et al., 2021 [56]. This indicates some of the conditions which have the potential to change the intentions of the parents towards their children’s vaccination.
5. Limitations
This study has some limitations. The respondents were network users, which means that the data were collected from individuals who have access to the internet and social media and do not represent a population without these characteristics.
Similarly, the variables included in this study were those that were available in the survey database, since there may have been more linked factors that were not quantified in the survey and should be included in future research. Nonetheless, this study demonstrates the value of evaluating a database comprised of a broad representative sample of individuals from several Arab nations by taking into consideration the homogeneity of their population.
6. Conclusion
The rate of Arab parents who intend to vaccinate their children against Covid-19 is still not high. Safety of their children and vaccine’s effect are the main concerns that parents have. This is partly birthed from the conditions of the pandemic where vaccines were quickly formulated and this was largely misunderstood by the public. There are also concerns of the adverse effects of taking the vaccine in the future wellbeing of the children, with claims of deformation, infertility and decreased life span being erroneously spread among the people. Therefore, it is recommended for parents to be availed with sufficient information on the vaccines, and how they would impact children with underlying conditions such as asthma and allergies. This information would increase the willingness of parents to have their children vaccinated. It would also curb the misinformation and erroneous suspicions surrounding COVID-19 pandemic and the various vaccination schemes. It is also recommended for the increased transparency on the potential adverse effects which vaccines have on children, as it would prepare parents and caregivers on how to cope with their children in the likelihood that it happens.
Ethical statement
All procedures performed in this study were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The Institutional Research Ethics Committee of Al Rafidain University College granted the ethical approval for this study (EC-71-2021).
Consent to participate
Informed consent was obtained from all individual participants in the study.
Consent to publish
Participants signed informed consent regarding publishing their de-identified data.
Availability of Data and Materials
Data and other materials are available upon request from the corresponding authors.
Funding
None.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
None.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.vaccine.2022.09.052.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
Data availability
Data will be made available on request.
References
- 1.Feng S., Shen C., Xia N., Song W., Fan M., Cowling B.J. Rational use of face masks in the COVID-19 pandemic. The Lancet Respiratory Med. 2020;8(5):434–436. doi: 10.1016/S2213-2600(20)30134-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cheng K.K., Lam T.H., Leung C.C. Wearing face masks in the community during the COVID-19 pandemic: altruism and solidarity. The Lancet. 2020 doi: 10.1016/S0140-6736(20)30918-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schünemann H.J., Akl E.A., Chou R., Chu D.K., Loeb M., Lotfi T., et al. Use of facemasks during the COVID-19 pandemic. The Lancet Respiratory Med. 2020;8(10):954–955. doi: 10.1016/S2213-2600(20)30352-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rosen B., Waitzberg R., Israeli A., Hartal M., Davidovitch N. Addressing vaccine hesitancy and access barriers to achieve persistent progress in Israel’s COVID-19 vaccination program. Israel J Health Policy Res. 2021;10(1):1–20. doi: 10.1186/s13584-021-00481-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Muhsen K., Cohen D. COVID-19 vaccination in Israel. Clin Microbiol Infect. 2021;27(11):1570–1574. doi: 10.1016/j.cmi.2021.07.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chernozhukov V., Kasahara H., Schrimpf P. Causal impact of masks, policies, behavior on early covid-19 pandemic in the US. J Econometrics. 2021;220(1):23–62. doi: 10.1016/j.jeconom.2020.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Santoli JM. Effects of the COVID-19 pandemic on routine pediatric vaccine ordering and administration—United States, 2020. MMWR Morbidity and mortality weekly report. 2020;69. [DOI] [PubMed]
- 8.Woodworth K.R., Moulia D., Collins J.P., Hadler S.C., Jones J.M., Reddy S.C., et al. The advisory committee on immunization practices’ interim recommendation for use of Pfizer-BioNTech COVID-19 vaccine in children aged 5–11 years—United States, November 2021. Morb Mortal Wkly Rep. 2021;70(45):1579. doi: 10.15585/mmwr.mm7045e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zou X., Cao B. COVID-19 vaccines for children younger than 12 years: are we ready? Lancet Infect Dis. 2021;21(12):1614–1615. doi: 10.1016/S1473-3099(21)00384-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Prevention CfDCa. COVID-19 Vaccines for Children and Teens; 2021.
- 11.Maldonado Y.A., O’Leary S.T., Banerjee R., Campbell J.D., Caserta M.T., Gerber J.S., et al. COVID-19 vaccines in children and adolescents. Pediatrics. 2021;148(2) doi: 10.1542/peds.2021-052336. [DOI] [PubMed] [Google Scholar]
- 12.Krok-Schoen J.L., Bernardo B.M., Weier R.C., Peng J., Katz M.L., Reiter P.L., et al. Belief about mandatory school vaccinations and vaccination refusal among Ohio Appalachian parents: Do demographic and religious factors, general health, and political affiliation play a role? J Rural Health. 2018;34(3):283–292. doi: 10.1111/jrh.12285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bell S., Clarke R., Paterson P., Mounier-Jack S. Parents’ and guardians’ views and experiences of accessing routine childhood vaccinations during the coronavirus (COVID-19) pandemic: A mixed methods study in England. PLoS ONE. 2020;15(12) doi: 10.1371/journal.pone.0244049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sato R., Belel A. The effect of performance-based financing on child vaccinations in northern Nigeria. Vaccine. 2020;38(9):2209–2215. doi: 10.1016/j.vaccine.2020.01.033. [DOI] [PubMed] [Google Scholar]
- 15.Wachob D., Boldy A. Social media’s influence on parents’ decision-making process of child vaccinations. Epidemiology, Biostatistics and Public Health. 2019;16(1) [Google Scholar]
- 16.Alruwaili A.A.S., Abo El-fetoh N.M., Alruwaili T.A.S., Alanazi W.A.S., Alhazmi H.H.R., Alanazi N.A.B., et al. Knowledge, attitude and practice of the parents regarding child vaccinations in Arar, Northern Saudi Arabia. Egypt J Hospital Med. 2018;72(9):5178–5182. [Google Scholar]
- 17.Weaver M.S., Wiener L. Applying palliative care principles to communicate with children about COVID-19. J Pain Symptom Manage. 2020;60(1):e8–e11. doi: 10.1016/j.jpainsymman.2020.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Samhan HH. Intra-ethnic diversity and religion. Biopsychosocial Perspectives on Arab Americans: Springer; 2014. p. 45–65.
- 19.Calculator RSS. Raosoft Inc-. 2004.
- 20.Zakeri M., Li J., Sadeghi S.D., Essien E.J., Sansgiry S.S. Strategies to decrease COVID-19 vaccine hesitancy for children. J Pharm Health Services Res. 2021;12(4):539–544. [Google Scholar]
- 21.Szilagyi P.G., Shah M.D., Delgado J.R., Thomas K., Vizueta N., Cui Y., et al. Parents’ intentions and perceptions about COVID-19 vaccination for their children: results from a national survey. Pediatrics. 2021;148(4) doi: 10.1542/peds.2021-052335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Makarić Z.L., Kolarić B., Tomljenović M., Posavec M. Attitudes and beliefs related to childhood vaccinations among parents of 6 years old children in Zagreb. Croatia Vaccine. 2018;36(49):7530–7535. doi: 10.1016/j.vaccine.2018.10.055. [DOI] [PubMed] [Google Scholar]
- 23.Ruggiero K.M., Wong J., Sweeney C.F., Avola A., Auger A., Macaluso M., et al. Parents’ intentions to vaccinate their children against COVID-19. J Pediatric Health Care. 2021;35(5):509–517. doi: 10.1016/j.pedhc.2021.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Galanis P.A., Vraka I., Siskou O., Konstantakopoulou O., Katsiroumpa A., Moisoglou I., et al. Predictors of parents intention to vaccinate their children against the COVID-19 in Greece: a cross-sectional study. medRxiv. 2021 [Google Scholar]
- 25.Alfieri N.L., Kusma J.D., Heard-Garris N., Davis M.M., Golbeck E., Barrera L., et al. Parental COVID-19 vaccine hesitancy for children: vulnerability in an urban hotspot. BMC Public Health. 2021;21(1):1–9. doi: 10.1186/s12889-021-11725-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Altulaihi B.A., Alaboodi T., Alharbi K.G., Alajmi M.S., Alkanhal H., Alshehri A. Perception of parents towards COVID-19 vaccine for children in Saudi population. Cureus. 2021;13(9) doi: 10.7759/cureus.18342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bell S., Clarke R., Mounier-Jack S., Walker J.L., Paterson P. Parents’ and guardians’ views on the acceptability of a future COVID-19 vaccine: A multi-methods study in England. Vaccine. 2020;38(49):7789–7798. doi: 10.1016/j.vaccine.2020.10.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Brandstetter S., Böhmer M.M., Pawellek M., Seelbach-Göbel B., Melter M., Kabesch M., et al. Parents’ intention to get vaccinated and to have their child vaccinated against COVID-19: cross-sectional analyses using data from the KUNO-Kids health study. Eur J Pediatr. 2021;1–6 doi: 10.1007/s00431-021-04094-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Montalti M., Rallo F., Guaraldi F., Bartoli L., Po G., Stillo M., et al. Would parents get their children vaccinated against SARS-CoV-2? rate and predictors of vaccine hesitancy according to a survey over 5000 families from Bologna, Italy. Vaccines. 2021;9(4):366. doi: 10.3390/vaccines9040366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Goldman R.D., Staubli G., Cotanda C.P., Brown J.C., Hoeffe J., Seiler M., et al. Factors associated with parents’ willingness to enroll their children in trials for COVID-19 vaccination. Human Vaccines & Immunotherapeutics. 2021;17(6):1607–1611. doi: 10.1080/21645515.2020.1834325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yigit M., Ozkaya-Parlakay A., Senel E. Evaluation of COVID-19 vaccine refusal in parents. Pediatr Infect Dis J. 2021;40(4):e134–e136. doi: 10.1097/INF.0000000000003042. [DOI] [PubMed] [Google Scholar]
- 32.Zhang K.C., Fang Y., Cao H., Chen H., Hu T., Chen Y.Q., et al. Parental acceptability of COVID-19 vaccination for children under the age of 18 years: cross-sectional online survey. JMIR Pediatrics and Parenting. 2020;3(2) doi: 10.2196/24827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Dyda A., King C., Dey A., Leask J., Dunn A.G. A systematic review of studies that measure parental vaccine attitudes and beliefs in childhood vaccination. BMC Public Health. 2020;20(1):1–8. doi: 10.1186/s12889-020-09327-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cooper S., Schmidt B.M., Sambala E.Z., Swartz A., Colvin C.J., Leon N., et al. Factors that influence parents' and informal caregivers' acceptance of routine childhood vaccination: a qualitative evidence synthesis. The Cochrane Database Syst Rev. 2019;2019(2) doi: 10.1002/14651858.CD013265.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wilder-Smith A.B., Qureshi K. Resurgence of measles in Europe: a systematic review on parental attitudes and beliefs of measles vaccine. J Epidemiology Global Health. 2020;10(1):46. doi: 10.2991/jegh.k.191117.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Domnich A., Cambiaggi M., Vasco A., Maraniello L., Ansaldi F., Baldo V., et al. Attitudes and beliefs on influenza vaccination during the COVID-19 pandemic: results from a representative Italian survey. Vaccines. 2020;8(4):711. doi: 10.3390/vaccines8040711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ganczak M., Bielecki K., Drozd-Dąbrowska M., Topczewska K., Biesiada D., Molas-Biesiada A., et al. Vaccination concerns, beliefs and practices among Ukrainian migrants in Poland: a qualitative study. BMC Public Health. 2021;21(1):1–13. doi: 10.1186/s12889-020-10105-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sinha I.P., Harwood R., Semple M.G., Hawcutt D.B., Thursfield R., Narayan O., et al. COVID-19 infection in children. The Lancet Respiratory Med. 2020;8(5):446–447. doi: 10.1016/S2213-2600(20)30152-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Banerjee A., Pasea L., Harris S., Gonzalez-Izquierdo A., Torralbo A., Shallcross L., et al. Estimating excess 1-year mortality associated with the COVID-19 pandemic according to underlying conditions and age: a population-based cohort study. The Lancet. 2020;395(10238):1715–1725. doi: 10.1016/S0140-6736(20)30854-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gold J.A., Wong K.K., Szablewski C.M., Patel P.R., Rossow J., Da Silva J., et al. Characteristics and clinical outcomes of adult patients hospitalized with COVID-19—Georgia, March 2020. Morb Mortal Wkly Rep. 2020;69(18):545. doi: 10.15585/mmwr.mm6918e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Krause P.R., Gruber M.F. Emergency use authorization of Covid vaccines—safety and efficacy follow-up considerations. N Engl J Med. 2020;383(19) doi: 10.1056/NEJMp2031373. [DOI] [PubMed] [Google Scholar]
- 42.Cai C., Peng Y., Shen E., Huang Q., Chen Y., Liu P., et al. A comprehensive analysis of the efficacy and safety of COVID-19 vaccines. Mol Ther. 2021;29(9):2794–2805. doi: 10.1016/j.ymthe.2021.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Soiza R.L., Scicluna C., Thomson E.C. Efficacy and safety of COVID-19 vaccines in older people. Age Ageing. 2021;50(2):279–283. doi: 10.1093/ageing/afaa274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Petousis-Harris H. Assessing the safety of COVID-19 vaccines: a primer. Drug Saf. 2020;43(12):1205–1210. doi: 10.1007/s40264-020-01002-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wu Q., Dudley M.Z., Chen X., Bai X., Dong K., Zhuang T., et al. Evaluation of the safety profile of COVID-19 vaccines: a rapid review. BMC Med. 2021;19(1):1–16. doi: 10.1186/s12916-021-02059-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Jiang S. Don't rush to deploy COVID-19 vaccines and drugs without sufficient safety guarantees. Nature. 2020;579(7798):321–322. doi: 10.1038/d41586-020-00751-9. [DOI] [PubMed] [Google Scholar]
- 47.Kochhar S., Salmon D.A. Planning for COVID-19 vaccines safety surveillance. Vaccine. 2020;38(40):6194–6198. doi: 10.1016/j.vaccine.2020.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lai C.-C., Chen I.-T., Chao C.-M., Lee P.-I., Ko W.-C., Hsueh P.-R. COVID-19 vaccines: concerns beyond protective efficacy and safety. Expert Rev Vaccines. 2021;20(8):1013–1025. doi: 10.1080/14760584.2021.1949293. [DOI] [PubMed] [Google Scholar]
- 49.Su S., Du L., Jiang S. Learning from the past: development of safe and effective COVID-19 vaccines. Nat Rev Microbiol. 2021;19(3):211–219. doi: 10.1038/s41579-020-00462-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Xing K., Tu X.-Y., Liu M., Liang Z.-W., Chen J.-N., Li J.-J., et al. Efficacy and safety of COVID-19 vaccines: a systematic review. Chin J Contemp Pediatrics. 2021;23(3):221. doi: 10.7499/j.issn.1008-8830.2101133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Schleiss M.R., John C.C., Permar S.R. Children are the key to the Endgame: A case for routine pediatric COVID vaccination. Vaccine. 2021 doi: 10.1016/j.vaccine.2021.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Allington D., McAndrew S., Moxham-Hall V., Duffy B. Coronavirus conspiracy suspicions, general vaccine attitudes, trust and coronavirus information source as predictors of vaccine hesitancy among UK residents during the COVID-19 pandemic. Psychol Med. 2021;1–12 doi: 10.1017/S0033291721001434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Riad A., Pokorná A., Antalová N., Krobot M., Zviadadze N., Serdiuk I., et al. Prevalence and drivers of COVID-19 vaccine hesitancy among Czech University students: national cross-sectional study. Vaccines. 2021;9(9):948. doi: 10.3390/vaccines9090948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Tanveer S., Rowhani-Farid A., Hong K., Jefferson T., Doshi P. Transparency of COVID-19 vaccine trials: decisions without data. BMJ Evidence-Based Med. 2021 doi: 10.1136/bmjebm-2021-111735. [DOI] [PubMed] [Google Scholar]
- 55.Anderson E.J., Campbell J.D., Creech C.B., Frenck R., Kamidani S., Munoz F.M., et al. Warp speed for coronavirus disease 2019 (COVID-19) vaccines: why are children stuck in neutral? Clin Infect Dis. 2021;73(2):336–340. doi: 10.1093/cid/ciaa1425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Zimmermann P., Pittet L.F., Finn A., Pollard A.J., Curtis N. Should children be vaccinated against COVID-19? Arch Dis Child. 2021 doi: 10.1136/archdischild-2021-323040. [DOI] [PubMed] [Google Scholar]
- 57.Mahase E. Covid vaccine could be rolled out to children by autumn. BMJ: Br Med J (Online) 2021;372 doi: 10.1136/bmj.n723. [DOI] [PubMed] [Google Scholar]
- 58.Opel D.J., Diekema D.S., Ross L.F. Should we mandate a COVID-19 vaccine for children? JAMA Pediatrics. 2021;175(2):125–126. doi: 10.1001/jamapediatrics.2020.3019. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data will be made available on request.