Abstract
Alcohol use is a major risk factor for noncommunicable diseases in Thailand, and one of its pathways is high blood pressure. Given that brief intervention can effectively reduce hazardous alcohol consumption, this study aimed to investigate how hypertensive patients with concomitant alcohol use are identified and treated in Thai primary care settings and what this may mean for screening and lifestyle intervention strategies. In a cross-sectional, mixed-method design, we surveyed 91 participants from three different groups of Thai stakeholders: policy- and decisionmakers; healthcare practitioners; and patients diagnosed with hypertension. Data was collected between December 2020 and May 2021. Responses were analyzed descriptively and using open coding tools to identify current practices, barriers, facilitators, and implications for interventions. All stakeholder groups regarded alcohol use as an important driver of hypertension. While lifestyle interventions among hypertensive patients were perceived as beneficial, current lifestyle support was limited. Barriers included limited resources in primary healthcare facilities, lack of continuous monitoring or follow-up, missing tools or procedures for risk assessment and lifestyle intervention, and stigmatization of alcohol use. Our results suggest that although screening for lifestyle risk factors (including alcohol use) and lifestyle interventions are not yet sufficiently established, a wide range of stakeholders still recognize the potential of interventions targeted at hazardous alcohol use among hypertensive patients. Future interventions may establish standardized assessment tools, be tailored to high-risk groups, and include electronic or remote elements.
Keywords: Hypertension, Primary Health Care, Alcohol use, Lifestyle intervention, Screening and brief intervention, Stakeholder survey, Thailand
1. Introduction
High blood pressure (hypertension) and alcohol use are both major risk factors for noncommunicable diseases (NCDs), placing a significant burden on patients, healthcare systems, and society as a whole (Murray et al., 2020). Globally, one in four men and one in five women were estimated to have hypertension (at least 140/90 mm Hg) in 2015 (NCD Risk Factor Collaboration, 2017), and the most recent Global Burden of Disease (GBD) estimates (2019) showed that high systolic blood pressure was the most impactful risk factor for mortality and disability-adjusted life-years (Murray et al., 2020). While the prevalence of hypertension is decreasing in high-income countries, it is rapidly increasing in low- and middle-income countries (Mills et al., 2016, NCD Risk Factor Collaboration NCD-RisC, 2017).
Importantly, alcohol use and hypertension are causally linked in a dose–response fashion (Taylor et al., 2009, O’Keefe et al., 2014, Briasoulis et al., 2012, Roerecke et al., 2018), making heavy alcohol use one of the most common causes of reversible hypertension. Interventions to reduce alcohol consumption could be a feasible and effective approach for reducing the prevalence of hypertension and related NCD burden (Roerecke et al., 2017). Results from several trials suggest a comparable reduction in patients’ blood pressure can be achieved through either lowering alcohol intake or other interventions that focus on lifestyle risk factors such as weight loss, diet and physical activity (Roerecke et al., 2017, Semlitsch et al., 2016, Lin et al., 2014). This is promising since alcohol brief interventions (defined as a conversation comprising five or fewer sessions of brief advice or brief lifestyle counselling and a total duration of fewer than 60 min) can reduce hazardous or harmful alcohol consumption and may be as effective as extended interventions (Beyer et al., 2019, O’Connor et al., 2018, Kaner et al., 2018). Currently, though overall implementation is low and there is a need for further education and stigma reduction (Rehm et al., 2016), evidence from Europe shows that alcohol screening in hypertensive patients was largely accepted by general practitioners (Hanschmidt et al., 2017). However, as of yet, there is limited evidence of attitudes and barriers elsewhere, such as South-East Asia, where alcohol use and hypertension are among the leading risk factors for NCDs (Murray et al., 2020).
For instance, it was estimated that hypertension accounted for about 8 % of the total disease burden in Thailand in 2019, with a 10 % increase over the past 10 years (Institute for Health Metrics and Evaluation, 2021). According to the Thai National Health Examination Survey (NHES V) conducted in 2014, one in four Thais had hypertension. Of those with hypertension, 45 % were unaware of it and only 30 % had their blood pressure under control (Roubsanthisuk et al., 2018). At the same time, with an estimated 8.8 liters of pure alcohol per capita in 2017, alcohol consumption in Thailand is nearly double the average consumption of the WHO South-East Asia Region overall (Manthey et al., 2019, Sornpaisarn et al., 2020, World Health Organization. Global Status Report on Alcohol and Health, https://apps.who.int/iris/rest/bitstreams/, 2018). While the prevalence of current drinking is comparatively low in Thailand with 55 % among men and 28 % among women, about 50 % (men) and 20 % (women) of the current drinkers engage in heavy episodic drinking (World Health Organization, 2018). While national clinical guidelines recommend lifestyle counselling for patients with hypertension (Thai Hypertension Society, 2019), it remains unclear to which extent alcohol brief interventions and lifestyle interventions that focus on other lifestyle risk factors are currently implemented in Thailand. We henceforth refer to all interventions focused on lifestyle risk factors – including but not limited to alcohol use – as lifestyle interventions.
In this study, we aimed to identify (i) current practices regarding alcohol use and lifestyle interventions among hypertensive patients, (ii) practical, social, economic, and cultural barriers to routine screening and lifestyle intervention targeted at hypertensive patients, particularly at those with hazardous alcohol use, and (iii) implications for targeted interventions in Thai primary care.
2. Methods
This study is a cross-sectional, mixed-method assessment based on surveys among three sets of respondents whose perspectives are relevant to hypertension care in Thailand: a) policy- and decisionmakers, members of educational institutions, and representatives from governing bodies of healthcare providers and advocacy groups (henceforth referred to as policymakers), b) healthcare practitioners (henceforth referred to as practitioners), and c) patients with hypertension (henceforth referred to as patients).
2.1. Study setting
The district health system, consisting of a district hospital together with several Community Health Promoting Hospitals (CHPHs) at subdistrict level, is the backbone of Thailand’s primary healthcare system. Practitioners and patients in our study were recruited in the province of Nakhon-Pathom, situated in a semi-urban setting about 50 kms outside-Bangkok. All six district hospitals of the province (providing primary and secondary care), the provincial hospital (providing tertiary care in addition to primary and secondary care), and one community hospital (limited to providing primary care and basic secondary care) were included in the study. Each district hospital serves a population of 30,000–50,000 and has inpatient facilities as well as outpatient clinics. With some variation, each district hospital is linked with 8–12 CHPH, which are the first point of contact for the population for preventive and basic curative services. While newly diagnosed hypertension cases may be identified through community-based or opportunistic screening during regular services, ongoing hypertension management primarily takes place in district hospitals’ NCD outpatient clinics (World Health Organization, 2019). According to National Hypertension Guidelines, while patients with hypertension wait their turn to see the doctor in NCD outpatient clinics, nurses, counsellors, or pharmacists provide group education on treatment adherence and healthy lifestyles (Thai Hypertension Society, 2019). At CHPH, hypertension management services are generally limited to prescription refills by nurses.
2.2. Inclusion criteria, sampling strategy, and recruitment
We purposely identified policymakers as established, national experts in either hypertension care or alcohol use through consultations, desktop and internet search, and review of policy and strategy documents. Policymakers were invited to participate in our study via e-mail or phone.
Practitioners were medical doctors and nurses working at outpatient clinics of the eight hospitals included in our study. With permission from the Provincial Health Administrative office, each hospital’s study coordinator invited all doctors and nurses working in the hypertension outpatient clinic (usually 1–3 per profession) to participate in our survey and distributed the questionnaires. Nurses may have simultaneously worked in alcohol clinics. Responses of those who returned the questionnaire to the hospital study coordinator were included in our study.
To ensure that patients had undergone all aspects of hypertension care (and not just diagnostics), patients must have had a recorded hypertension diagnosis made at least 6 months ago. We chose 35 years as the minimum age requirement as this is the threshold to be eligible for organized hypertension screening activities, and hypertension prevalence is notably higher compared to adult patients aged below 35 years (Charoendee et al., 2018, Thai Hypertension Society. Thai Hypertension Guideline, http://www.thaihypertension.org/files/HT guideline, 2019). Half of the patients were purposely selected by the hospital study coordinator based on their prior medical records indicating alcohol use, while the other half constituted a convenience sample of patients diagnosed with hypertension. Nurses and village health volunteers supported the recruitment of all patients and arranged appointments at their nearest health facility. Respondents provided informed consent and were compensated for their time.
2.3. Study materials, data collection, and analysis
Questionnaires elicited information regarding current practices and feasibility of interventions targeted at concomitant hypertension and alcohol use (Fig. 1). The content was adapted to the perspective of each stakeholder group. Questionnaire sections generally included a set of statements for which participants indicated their response on a Likert scale, followed by an open-ended question or the option for additional comment by the respondent. The development of questions was loosely guided by the Consolidated Framework for Implementation Research (CFIR), a typology of constructs that have been associated with effective implementation (Damschroder et al., 2009, VanDevanter et al., 2017).
Fig. 1.
Content of survey-based assessment for each stakeholder group.
Data collection took place between December 2020 and May 2021. Policymakers were surveyed online. Practitioners responded to self-administered paper–pencil questionnaires. Patient surveys were conducted in person and responses were recorded verbatim on paper–pencil questionnaires by the interviewer. Answers to open-ended questions were translated by a professional translator using standard translation procedure.
In our analysis, we first analyzed responses and described response patterns separately within each stakeholder group before comparing results between stakeholder groups. Closed-ended questions were analyzed descriptively using R version 4.1.0 (R Core Team, 2021). For each Likert-scaled statement, we compared the share of respondents disagreeing (Completely disagree/disagree) with the share of respondents agreeing (Completely agree/agree). We show key results for each stakeholder group by illustrating selected Likert-scaled statements in a vertical bar graph anchored at the neutral response category. We further created a heat map using Excel to compare the share of respondents in each stakeholder group indicating that they “completely agree” or “agree” with the statement. Here, we only included statements that were included in the questionnaires of at least two different stakeholder groups to show varying strengths of agreement across stakeholder groups. Open-ended questions were analyzed using open coding tools from thematic content analysis. Specifically, after breaking each qualitative answer into individual response components and labeling each component, coding results were grouped by theme within the broader categories of barriers, facilitators, and implications.
2.4. Ethics
Ethics approval was obtained from the institutional ethics boards of the Centre for Addiction and Mental Health (REB# 076/2020) and Mahidol University (MUSSIRB:2020/169(B1)).
3. Results
In total, 91 stakeholders participated in our survey (Table 1). Policymakers worked at governmental policy institutions (n = 6), in governing bodies of healthcare providers (n = 3), at university or policy research institutions (n = 11), and for advocacy groups (n = 2). Detailed characteristics of policymakers are shown in Supplementary Table 1. Practitioners included 15 clinical nurses and 9 medical doctors. Detailed characteristics of practitioners are shown in Supplementary Table 2. Of 45 patients diagnosed with hypertension, 28 (62 %) consumed an alcoholic beverage at least twice a week (Supplementary Table 3).
Table 1.
Sample characteristics.
| Variable | Policymakers | Practitioners | Patients with hypertension |
|---|---|---|---|
| N | 22 | 24 | 45 |
| Age in years, median (range) | 58 (29–81) | 46.5 (26–70) | 52 (37–75) |
| Female, n (%) | 14 (63.6) | 19 (79.2) | 6 (13.3) |
We present key results by stakeholder group. For each group, results are divided into three sub-sections including current practices, barriers and facilitators, and areas for potential improvement. This is followed by a comparison of similarities and differences between stakeholder groups. All results were informed by responses to both closed- and open-ended questions. Exemplar verbatim quotations from stakeholders are presented in Table2.
Table 2.
Exemplar quotations from stakeholders and implications for potential interventions.
| Area | Quotation | Rationale | Implication |
|---|---|---|---|
| Blood pressure screening | |||
| “Factory workers […] who are sick with hypertension often go to receive services outside their scheduled times because they fear wasting working time and having their wages deducted. There should be an accommodation for the worker care service system to better and systematically access services at their workplaces.” (Professor of Public Health Nursing, female, 53 years) | At-risk populations such as informal laborers or factory workers, that are insufficiently reached through traditional routes, may profit from targeted interventions. | Identify strategies for at-risk populations. | |
| Lifestyle risk factor screening | |||
| “The alcohol screening tool is complicated [and] hard to understand. There are too many questions. For example, AUDIT is not suitable for screening in the Thai social context.” (Professor of Medicine, female, 56 years)“ Using modern and easy-to-understand tools in measuring the amount of alcohol and drinking patterns, such as adopting a program that includes illustrations.” (Researcher at International Health Policy Program Office, female, 40 years) |
Effective screening may improve the targeting of alcohol use as a risk factor for hypertension. | Implement standardized, easy to use assessment tools that are adapted to the Thai context. | |
| “There are many patients waiting and not enough time to discuss it.” (Patient, male, 50 years)“ If there are too many patients at government facilities, it directly affects the quality of the counseling provided.” – Medical doctor at District Hospital (male, 69) |
Limited resources in healthcare facilities need to be carefully divided and efficiently employed. | Identify strategies to reduce congestion at facilities and workload of practitioners. | |
| “Asking about drinking alcohol for all males is easy and normal. Women, on the other hand, are sometimes nervous when asked.” (Clinical nurse, female, 42 years, district hospital) “Patients are afraid to tell the truth that they drink alcohol.” (Patient, male, 37 years) |
Create an environment where patients, in particular female patients, feel comfortable discussing their alcohol use. | Identify strategies to reduce stigmatization of (heavy) alcohol use. | |
| Lifestyle interventions | |||
| “There should be a specific approach used as an easy-to-follow manual for personnel and a user-friendly manual for patients that they can utilize themselves […].” (Director at Department of Disease Control, female, 56 years) | Access to standardized, high-quality lifestyle support and counselling should be ensured for all patients. | Develop clear and concise guidelines for evidence-based interventions. | |
| “[Remote intervention] can be used to follow up behavior modification and to empower the patient. This will help reduce the missing of appointments.” (Operation Chief of the Primary Care Services at Regional Public Health Office, male, 50 years) | Improve patient compliance and long-term lifestyle modification. | Introduce monitoring mechanisms for (changes in) lifestyle behavior and alcohol use. | |
| “Advantages [are] being able to get advice at anytime, anywhere with a signal, and every-one can access it, if they have electronic communication devices.” (Medical doctor, male, 58 years, district hospital) “Most of the patients with chronic diseases are the elderly. They are not skillful in using electronic devices. Some people are poor and obtaining electronic equipment is difficult.” – Clinical nurse, female, 36 years, NCD clinic |
Digital tools may be used to expand equal access to lifestyle interventions. | Implement remote and electronically supported intervention elements that are compatible with the population’s skillset. | |
| “Advice can only be provided at the NCD clinic. Outside the clinic, there are some, but it depends on the service provider.” (Clinical nurse, female, 52 years, district hospital) | Health promotion and lifestyle counselling at sub-district level may be more easily accessed by patients. | Strengthen resources and activities at sub-district level. | |
3.1. Policymakers
3.1.1. Current practices
There was large variation in the perceived status quo of blood pressure screening: 39 % of policymakers agreed with the statement that blood pressure screening is routinely performed in primary healthcare facilities, while 44 % disagreed, and almost half (47 %) agreed that there is no or insufficient community-based screening. Policymakers agreed that expansion of blood pressure screening should focus on places outside of clinical settings, i.e., community-, home-, or workplace-based screening. Some policymakers highlighted that screening has not been comprehensively expanded, especially in urban areas with few health volunteers, disadvantaged communities, or inaccessible areas, such as island regions. This is supported by statements that hypertension care is presently not catered to individuals with low socioeconomic status or health literacy, informal laborers, and populations whose working hours impede receiving care (Table2). Policymakers agreed (81 %) that both lifestyle risk factor screening and lifestyle interventions among patients with hypertension are insufficiently implemented.
3.1.2. Barriers and facilitators
Smoking and alcohol were recognized as important drivers of hypertension by all policymakers. However, one respondent was critical of the importance of screening for alcohol use, arguing that there is a low prevalence of heavy drinking among hypertensive patients.
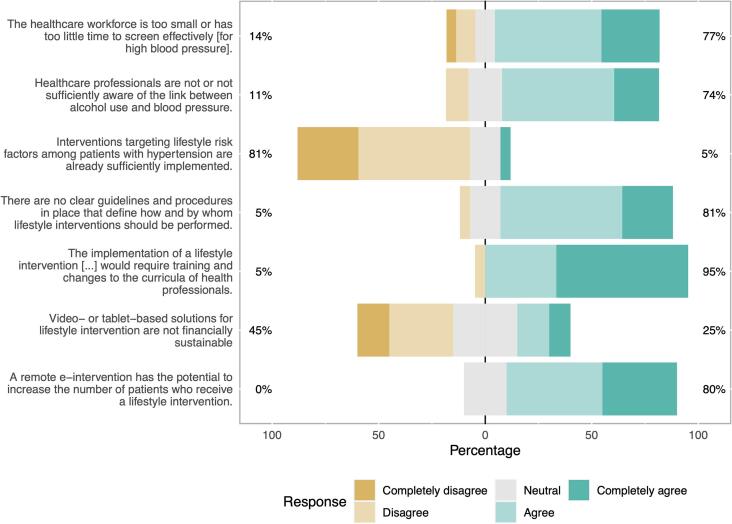
In terms of barriers, policymakers agreed (64 %) that current guidelines regarding procedures of lifestyle risk factor screening are not clear enough. Policymakers supported the statement that practitioners are insufficiently or completely unaware of the link between alcohol use and raised blood pressure (Fig. 2). A lack of appropriate screening tools for systematically assessing alcohol use in the Thai primary healthcare context was identified as another barrier (Table2). Policymakers were split on whether there is a stigma associated with heavy drinking and whether practitioners are comfortable discussing alcohol use with patients. While there was high agreement that hypertension medication should be complemented with lifestyle intervention (95 %), insufficient resources (e.g., time, personnel, funds, or space) were seen as an important barrier to lifestyle risk factor screening and interventions (Fig. 2).
Fig. 2.
Responses from policymakers (n = 22) to selected items that are relevant to implementing targeted lifestyle interventions for patients with hypertension. The percentage on the left side indicates the share of policymakers disagreeing (Completely disagree/Disagree) with the statement; the percentage on the right side indicates the share of policymakers agreeing (Completely agree/Agree) with the statement.
3.1.3. Potential improvements
Policymakers agreed that improvements in different areas of hypertension care are urgent, with ‘blood pressure screening’ and ‘screening for and addressing lifestyle risk factors’ ranking highest in urgency. Policymakers supported prioritizing lifestyle counselling in practitioners’ curricula (86 %) and raised concerns about the health system’s current foci:
“The medical care system that doctors learned from in medical schools still focuses on treatment with medication and spends less time promoting, preventing, and referring patients. […]” – Operation Chief of the Primary Care Services at Regional Public Health Office (male, 50).
Similarly, respondents noted that the provision of services is not sufficiently focused on “creating systematic health literacy” (Public Health Technical Officer, female, 60) and that “the dimensions of health promotion are overlooked” (Researcher at International Health Policy Program Office, female, 40). Policymakers emphasized the need for skill building among practitioners concerning health communication, effectively increasing the health literacy of patients, and screening to identify lifestyle risk factors. They agreed (90 %) that in-person lifestyle screening and interventions should be complemented by electronic tools but were divided as to whether video- or tablet-based solutions are financially sustainable (Fig. 2). Similarly, remote lifestyle interventions were viewed positively by policymakers. However, while they acknowledged the opportunity to reduce in-person time and increase the number of patients who receive a lifestyle intervention, they feared that remote e-interventions may be inaccessible to many patients due to a lack of mobile devices, internet access, or digital skills (Table2).
3.2. Practitioners
3.2.1. Current practices
Practitioners were divided on whether blood pressure screening is routinely performed in primary healthcare facilities, with 42 % agreeing and 46 % disagreeing. However, all practitioners indicated that patients with hypertension are being screened for behavioral risk factors and receive some form of lifestyle intervention in their facilities (where applicable for patients). When instead asked what percentage of the general eligible population of hypertensive patients receive lifestyle interventions, estimates varied from 40 to 100 % with a median of 80 %. Lifestyle interventions included in-person conversation (92 %), standardized leaflet (88 %) and presentation (42 %), video (33 %), or written personalized information (33 %), and were mostly performed by doctors or nurses. For district hospitals, the estimated average maximum duration of lifestyle intervention was slightly shorter (13.2 min) compared to CHPH (16.7 min) where responses varied greatly from 0 to 60 min. All practitioners indicated that alcohol use is being discussed with hypertension patients either regularly (58 %) or sometimes (42 %). When asked about what topics are being addressed by lifestyle intervention, smoking and alcohol use ranked highest (96 % and 88 %, respectively).
3.2.2. Barriers and facilitators
Practitioners cited insufficient resources (e.g., knowledge and tools) at CHPH and patients’ working hours or frequent relocation as general barriers to hypertension care. They identified migration workers and elderly patients without any caretakers as risk groups.
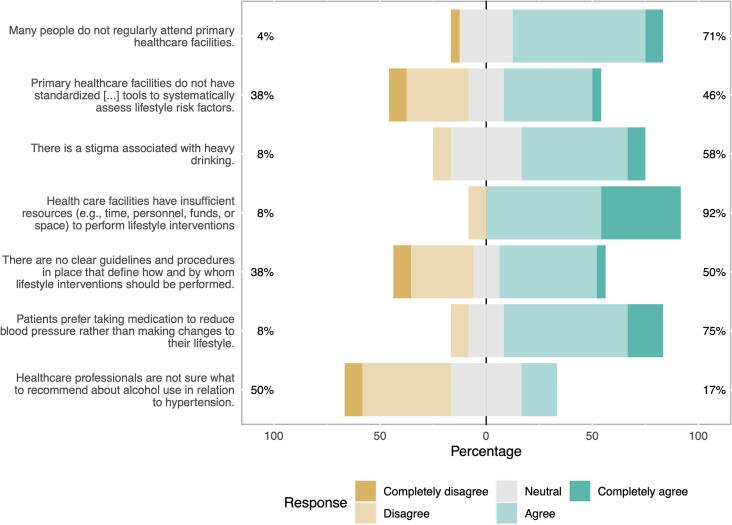
The majority (58 %) disagreed that practitioners know too little about blood pressure screening procedures or lifestyle risk factors for hypertension. Lifestyle risk factors were perceived as important drivers for hypertension, with smoking and salt or sodium considered slightly more important than others. Practitioners were divided on whether primary healthcare facilities have standardized tools to systematically assess lifestyle risk factors (Fig. 3). Though most practitioners perceived heavy drinking among patients as stigmatized, they disagreed with statements that their peers are insufficiently aware of the link between alcohol use and blood pressure (54 %) and that they do not feel comfortable raising the topic of alcohol use with patients (73 %) (Fig. 3).
Fig. 3.
Responses from practitioners (n = 24) to selected items that are relevant to implementing targeted lifestyle interventions for patients with hypertension. The percentage on the left side indicates the share of practitioners disagreeing (Completely disagree/Disagree) with the statement; the percentage on the right side indicates the share of practitioners agreeing (Completely agree/Agree) with the statement.
Practitioners agreed that patients feel uncomfortable discussing their alcohol use (70 %) and several respondents worried about harming their relationship with the patient. They noted that women rarely disclose information about alcohol use, which “makes solving the problem of alcohol drinking impossible” (Clinical nurse, female, 45), and that female patients may feel “more humiliated than male patients” when asked about alcohol use (Clinical nurse, 55, female). Some practitioners asserted that women rarely drink or, congruously, that, if a patient is female, staff may not think that she drinks alcohol.
Practitioners perceived lifestyle interventions as useful. However, they overwhelmingly agreed that resources are presently lacking to perform these interventions (Fig. 3) and that congestion in district hospitals affects the quality of interventions (Table 2). Half of the practitioners agreed that there are no guidelines and procedures in place that define how and by whom lifestyle interventions should be performed (Fig. 3). While several free-text responses highlighted patient-related characteristics as barriers (e.g., noncompliance), one nurse (female, 54) acknowledged that “[…] healthcare services are more focused on medication treatment than risk behavior management.”.
3.2.3. Potential improvements
Practitioners recognized the potential of remote or electronically supported lifestyle interventions, in particular by allowing patients to access support in any place and at any time (Table2). This is in line with practitioners’ view that many Thai people do not regularly attend primary healthcare facilities (70 %) and that patients often do not return for follow-up appointments (68 %). However, practitioners also expressed concerns about adaptability, with 75 % agreeing that a remote e-intervention will be inaccessible to many patients (Table2).
At the same time, 79 % of practitioners agreed that it is important for patients to be able to directly consult a health care professional and they were largely undecided (50 %) as to whether patients would be willing to follow advice that is not given by an on-site health professional (e.g., by way of a remote e-intervention). Respondents noted that conversations held remotely may end up being a “one-way communication” and may impede giving feedback.
3.3. Patients diagnosed with hypertension
3.3.1. Current practices
Over two-thirds of patients (78 %) indicated that someone explained the causes of hypertension when they were first diagnosed. However, there was variation in the number of patients that reported assessment of different lifestyle risk factors, with 98 % for smoking, 96 % for alcohol use, 84 % for body weight or BMI, 73 % for diet or nutrition, and 69 % for salt or sodium intake.
All patients except for one (98 %) indicated that they received some form of lifestyle intervention upon their initial diagnosis of hypertension. This was most often delivered or performed by a doctor (77 %), a nurse (73 %), or a pharmacist (25 %). The format and duration of advice varied within our patient group: while 16 % indicated that they have only received written information, most patients (58 %) reported that the lifestyle intervention lasted more than 5 and less than 15 min, with some reporting duration of fewer than five minutes (13 %) or of more than 15 min and up to one hour (11 %). Lifestyle interventions most often addressed diet or nutrition (86 %), alcohol use (73 %), smoking habits (73 %), body weight or BMI (61 %), or salt or sodium intake (59 %).
3.3.2. Barriers and facilitators
Patients agreed that lifestyle behaviors, including alcohol use, are relevant to the development and progression of hypertension in the Thai population. However, they were divided on whether practitioners had practicable advice for patients on how to change their lifestyle (Fig. 4).
Fig. 4.
Responses from patients diagnosed with hypertension (n = 45) to selected items that are relevant to implementing targeted lifestyle interventions for patients with hypertension. The percentage on the left side indicates the share of patients disagreeing (Completely disagree/Disagree) with the statement; the percentage on the right side indicates the share of patients agreeing (Completely agree/Agree) with the statement.
At the same time, patients were undecided on whether the relevant patient population was motivated to change their lifestyle (50 % neutral and 47 % agreement). Patients mentioned their peers, socializing habits, and daily routines as barriers to changing their lifestyle and alcohol use. Some patients expressed the belief that medication should prevail as the first line of treatment for lowering blood pressure and that lifestyle modification alone is insufficient. Two-thirds of patients agreed with the statement that there is stigma associated with heavy drinking (60 %), noting that “patients are afraid to tell the truth that they drink alcohol” (Patient, male, 37; Table2).
3.3.3. Potential improvements
Most patients agreed that it is important for them to be able to ask questions directly to a health professional (85 %). This may explain a rather skeptical view of remote and electronic interventions (Fig. 4). Many free-text answers supported the notion that not all patients have the skills to operate smart devices and/or lack access to them. While there were concerns about the reach of remote interventions, views on their efficacy were split: while 49 % agreed that remote e-interventions are a good alternative to in-person lifestyle interventions, 33 % disagreed. In free-text responses, some patients acknowledged the potential benefits of remote interventions, with reduced travel time being cited most often.
3.4. Comparison across stakeholder groups
Fig. 5 shows the strength of agreement across key areas for each stakeholder group. Both policymakers and practitioners agreed that improvements in hypertension care, especially relating to lifestyle modification, are necessary. Across groups, there was not only a general understanding that lifestyle modification is critical to hypertension care but also that alcohol is an important risk factor for hypertension (Fig. 5). However, stakeholders repeatedly mentioned that current hypertension care prioritizes medication, potentially contributing to patients’ belief that lifestyle modification is secondary to lowering blood pressure.
Fig. 5.
A heat map indicating the percentage of respondents in each stakeholder group indicating that they “completely agree” or “agree” with the statement. Values range from 0% (beige color) to 100% (dark turquoise color). a Percentage that deemed alcohol an “important” or “very important” risk factor for hypertension. b Percentage of respondents that reported to counsel on alcohol use or that report to have been counselled on alcohol use.
While both practitioners and patients diagnosed with hypertension indicated that alcohol use is currently being assessed and discussed, there seems to be no standardized tools or procedures for risk assessment and lifestyle intervention that are being universally applied (Fig. 5). Lifestyle interventions that are being offered seem to vary in duration, intensity, medium, and content.
Barriers were viewed somewhat heterogeneously across stakeholder groups (Fig. 5). Policymakers and practitioners cited lacking resources and compatibility with existing workflows as barriers. While policymakers questioned practitioners’ knowledge relating to alcohol use and hypertension, and their ability to perform lifestyle interventions, surveyed practitioners recognized the link between alcohol use and hypertension and were confident addressing alcohol use and lifestyle changes with patients. Instead, practitioners cited patient-related characteristics as barriers to realizing effective lifestyle modification. Unlike policymakers, practitioners and patients perceived alcohol use as stigmatized and cited patients’ reluctance in disclosing their alcohol use as a barrier.
There were competing views about remote lifestyle interventions: while stakeholders recognized the potential to reach patients that would otherwise not receive care, and to reduce congestion in hospitals, they highlighted that remote interventions may not be available to all population groups due to lacking access and skills among the elderly, poor, or less educated population segments. Patients also expressed differing opinions regarding the efficacy of remote interventions. However, policymakers and practitioners in particular, exhibited rather favorable views towards remote or electronically supported lifestyle interventions.
4. Discussion
This study assessed practices and barriers relating to screening and interventions for lifestyle risk factors among patients diagnosed with hypertension, in particular regarding alcohol use, from three different perspectives. Building on the CFIR typology (Damschroder et al., 2009), we have identified several constructs (henceforth stylized in italics) within four CFIR domains (intervention characteristics, outer and inner setting, and characteristics of individuals) that are likely relevant for the successful implementation of interventions targeting lifestyle behaviors (alcohol use) among patients diagnosed with hypertension in Thailand. In the following section, we provide a synthesis of our study results by mapping implications for implementing such interventions onto CFIR constructs.
Regarding intervention characteristics, there was a general appreciation of the evidence strength and quality among stakeholders that lifestyle support should play a key role when treating hypertensive patients with and without concomitant alcohol use. This is in line with previous findings that identified the efficacy of alcohol screening and brief intervention (SBI) as an enabling factor for successful implementation (Chan et al., 2021). A digital approach that provides a standardized, self-administered assessment and intervention with minimal training requirements and flexible follow-up conditional on the patient needs may further provide a relative advantage over existing procedures, while ensuring an inclusive approach that is adaptable to meet local needs (Adam et al., 2019, Wiemker et al., 2022). For example, patient groups that are both at a higher risk to engage in heavy episodic drinking and less likely to be reached through traditional primary care pathways might require targeted intervention strategies (Table 2). At the very least, improvements in standardized, context-appropriate tools and clear procedures for risk assessment and lifestyle intervention are warranted (Abidi et al., 2016).
The proposal of a (digital) SBI to reduce blood pressure has received high support by policy stakeholders which may be indicative of a positive outer setting regarding external policy and incentives. While effectiveness is not yet sufficiently demonstrated, smartphone applications designed to assist users to reduce hazardous alcohol consumption show potential as an inexpensive alternative to brief intervention in primary care (Colbert et al., 2020). At the same time, wider patient needs and resources must be accurately known and considered: intervention strategies that rely on remote or electronic elements have to strike a balance between providing convenient care to at-risk groups and avoiding reinforcing health disparities along the digital divide that often exists between marginalized and ‘connected’ population segments (Levy and Janke, 2016, Khoong et al., 2021, Liu et al., 2020).
The construct tension for change in the inner setting domain describes the degree to which stakeholders perceive the current situation as intolerable or needing change. While stakeholders agreed that prioritization of health promotion activities is essential for improving hypertension management in Thailand, available resources and access to knowledge and information were identified as the main limiting factors. In particular concerning available resources, any potential intervention needs to carefully consider time constraints and congestion in district hospitals as well as lacking resources and coverage at the sub-district level.
With regard to knowledge and beliefs about the intervention (in the domain of characteristics of individuals), stakeholders mentioned concerns due to the potential stigmatization of heavy alcohol use. While the latter point underlines the importance of ensuring confidentiality and acceptance as an integral part of any intervention (preventing potential alienation of patients, in particular in relation to gender), practitioners overall showed a high self-efficacy by reporting confidence in their abilities to screen for and give advice regarding alcohol use. Self-efficacy of practitioners has been repeatedly reported to be an enabler for implementing SBI in primary care (Chan et al., 2021).
Our study results are in line with previous empirical findings on barriers to implementing SBI that generally highlight the role of adequate resources, training, and the identification of those at risk without stereotyping as main facilitators in primary care (Chan et al., 2021, Johnson et al., 2011). While there were structural barriers (e.g., the fact that practitioners have many competing tasks in the Thai primary care system), most of the identified barriers are modifiable per se and, maybe more importantly, set in a wider positive implementation climate. Thus, we argue that it may be worth focusing on hazardous alcohol use among hypertensive patients in Thai primary care, in particular given the existing evidence for positive effects of reducing alcohol intake on hypertension (Roerecke et al., 2018, Roerecke et al., 2017). Given the substantial alcohol-attributable risk in Thailand (Institute for Health Metrics and Evaluation, 2021) and that even short interventions can effectively reduce alcohol consumption (Beyer et al., 2019, O’Connor et al., 2018, Kaner et al., 2018), prioritizing hazardous alcohol use among hypertensive patients has the potential for substantial synergistic health gains and healthcare cost reductions by lowering the burden of NCDs (Rehm et al., 2017, Rehm and Roerecke, 2013, Baliunas et al., 2009, Patra et al., 2010).
4.1. Limitations
This study has several limitations. First, recruitment of respondents was conducted at only eight hospitals, all situated in Nakhon-Pathom province, and participants constitute a convenience sample. As well, relatively small sample sizes were used for each stakeholder group. Therefore, the results are not representative of all primary healthcare facilities in Thailand. However, by including three different groups with broad inclusion criteria, we ensured that diverse perspectives were assessed. Second, while we ensured that the focus on alcohol use was not obvious from the outset, respondents may have exhibited socially desirable behavior by acknowledging alcohol as an important risk factor for hypertension (Lavrakas, 2008). Third, respondents may have operated under varying assumptions of what lifestyle interventions entail as we provided a broad definition of lifestyle intervention to capture all current activities.
4.2. Conclusion
Stakeholders recognized the potential of screening and brief interventions targeting hazardous alcohol use among hypertensive patients. We identified barriers as well as potential implications that may guide the development and implementation of such interventions. Future research may establish the feasibility of such interventions, while attention should be paid to any solution that could reinforce existing inequities along social and demographic gradients.
CRediT authorship contribution statement
Julia M. Lemp: Conceptualization, Methodology, Formal analysis, Writing – original draft, Visualization. Supa Pengpid: Conceptualization, Investigation, Writing – review & editing, Project administration. Doungjai Buntup: Investigation, Writing – review & editing. Till W. Bärnighausen: Writing – review & editing. Pascal Geldsetzer: Writing – review & editing. Karl Peltzer: Writing – review & editing. Jürgen Rehm: Conceptualization, Writing – review & editing. Bundit Sornpaisarn: Writing – review & editing. Charlotte Probst: Conceptualization, Methodology, Writing – review & editing, Supervision, Project administration, Funding acquisition.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
We thank the survey team and stakeholder participants who made this analysis possible. We would also like to thank Tessa Carr for her diligent proofreading of this article. The authors declare that there are no conflicts of interest pertaining to this research. This research was funded by the Institute Community Support Program of the Canadian Institutes of Health Research (PCS-168229). Funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.pmedr.2022.101954.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
Data availability
Data will be made available on request.
References
- Abidi L., Oenema A., Nilsen P., Anderson P., van de Mheen D. Strategies to overcome barriers to implementation of alcohol screening and brief intervention in general practice: a delphi study among healthcare professionals and addiction prevention experts. Prev. Sci. 2016;17(6):689–699. doi: 10.1007/s11121-016-0653-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adam A., Schwartz R.P., Wu L.-T., Subramaniam G., Laska E., Sharma G., Mili S., McNeely J. Electronic self-administered screening for substance use in adult primary care patients: feasibility and acceptability of the tobacco, alcohol, prescription medication, and other substance use (myTAPS) screening tool. Addiction Science & Clinical Practice. 2019;14(1) doi: 10.1186/s13722-019-0167-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baliunas D.O., Taylor B.J., Irving H., Roerecke M., Patra J., Mohapatra S., Rehm J. Alcohol as a risk factor for type 2 diabetes: a systematic review and meta-analysis. Diabetes Care. 2009;32(11):2123–2132. doi: 10.2337/dc09-0227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beyer F.R., Campbell F., Bertholet N., Daeppen J.B., Saunders J.B., Pienaar E.D., Muirhead C.R., Kaner E.F.S. The Cochrane 2018 Review on Brief Interventions in Primary Care for Hazardous and Harmful Alcohol Consumption: A Distillation for Clinicians and Policy Makers. Alcohol and Alcoholism. 2019;54:417–427. doi: 10.1093/alcalc/agz035. [DOI] [PubMed] [Google Scholar]
- Briasoulis A., Agarwal V., Messerli F.H. alcohol consumption and the risk of hypertension in men and women: a systematic review and meta-analysis. J. Clinical Hypertension. 2012;14:792–798. doi: 10.1111/jch.12008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan P.-F., Fang Y., Wong M.-S., Huang J., Wang Z., Yeoh E.K. Using consolidated framework for implementation research to investigate facilitators and barriers of implementing alcohol screening and brief intervention among primary care health professionals: a systematic review. Implementation Science. 2021;16(1) doi: 10.1186/s13012-021-01170-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charoendee K., Sriratanaban J., Aekplakorn W., et al. Assessment of population coverage of hypertension screening in thailand based on the effective coverage framework. BMC Health Services Research. 2018;18:1–9. doi: 10.1186/s12913-018-2996-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colbert S., Thornton L., Richmond R. Smartphone apps for managing alcohol consumption: a literature review. Addiction Science & Clinical Practice. 2020;15:17. doi: 10.1186/s13722-020-00190-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Damschroder L.J., Aron D.C., Keith R.E., Kirsh S.R., Alexander J.A., Lowery J.C. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implementation Science. 2009;4(1) doi: 10.1186/1748-5908-4-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanschmidt F., Manthey J., Kraus L., et al. Barriers to Alcohol Screening Among Hypertensive Patients and the Role of Stigma: Lessons for the Implementation of Screening and Brief Interventions in European Primary Care Settings. Alcohol and Alcoholism. 2017;52(5):572–579. doi: 10.1093/alcalc/agx032. [DOI] [PubMed] [Google Scholar]
- Institute for Health Metrics and Evaluation (IHME). GBD Compare, https://vizhub.healthdata.org/gbd-compare/ (2021, accessed 22 June 2021).
- Johnson M., Jackson R., Guillaume L., Meier P., Goyder E. Barriers and facilitators to implementing screening and brief intervention for alcohol misuse: a systematic review of qualitative evidence. J. Public Health. 2011;33(3):412–421. doi: 10.1093/pubmed/fdq095. [DOI] [PubMed] [Google Scholar]
- Kaner E.F., Beyer F.R., Muirhead C., et al. Effectiveness of brief alcohol interventions in primary care populations. The Cochrane database of systematic reviews. 2018;2(6):CD004148. doi: 10.1002/14651858.CD004148.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khoong E.C., Olazo K., Rivadeneira N.A., Thatipelli S., Barr-Walker J., Fontil V., Lyles C.R., Sarkar U. Mobile health strategies for blood pressure self-management in urban populations with digital barriers: systematic review and meta-analyses. npj Digital Med. 2021;4(1) doi: 10.1038/s41746-021-00486-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lavrakas P (Ed.). 2008. Social Desirability. Encyclopedia of Survey Research Methods. 2455 Teller Road, Thousand Oaks California 91320 United States of America: Sage Publications, Inc. doi: 10.4135/9781412963947.n537.
- Levy H., Janke A. Health literacy and access to care. J. Health Communication. 2016;21(sup1):43–50. doi: 10.1080/10810730.2015.1131776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin J, O’Connor E, Evans C, et al. Behavioral Counseling to Promote a Healthy Lifestyle for Cardiovascular Disease Prevention in Persons With Cardiovascular Risk Factors: An Updated Systematic Evidence Review for the U.S. Preventive Services Task Force. Rockville, MD, USA, 2014. [PubMed]
- Liu P., Astudillo K., Velez D., Kelley L., Cobbs-Lomax D., Spatz E.S. Use of mobile health applications in low-income populations: a prospective study of facilitators and barriers. Circ: Cardiovascular Quality and Outcomes. 2020;13(9) doi: 10.1161/CIRCOUTCOMES.120.007031. [DOI] [PubMed] [Google Scholar]
- Manthey J., Shield K.D., Rylett M., Hasan O.S.M., Probst C., Rehm J. Global alcohol exposure between 1990 and 2017 and forecasts until 2030: a modelling study. The Lancet. 2019;393(10190):2493–2502. doi: 10.1016/S0140-6736(18)32744-2. [DOI] [PubMed] [Google Scholar]
- Mills K.T., Bundy J.D., Kelly T.N., Reed J.E., Kearney P.M., Reynolds K., Chen J., He J. Global disparities of hypertension prevalence and control: a systematic analysis of population-based studies from 90 countries. Circulation. 2016;134(6):441–450. doi: 10.1161/CIRCULATIONAHA.115.018912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray C.J.L., Aravkin A.Y., Zheng P., et al. Global burden of 87 risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. The Lancet. 2020;396(10258):1223–1249. doi: 10.1016/S0140-6736(20)30752-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NCD Risk Factor Collaboration (NCD-RisC) Worldwide trends in blood pressure from 1975 to 2015: a pooled analysis of 1479 population-based measurement studies with 19·1 million participants. The Lancet. 2017;389(10064):37–55. doi: 10.1016/S0140-6736(16)31919-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Connor E.A., Perdue L.A., Senger C.A., Rushkin M., Patnode C.D., Bean S.I., Jonas D.E. Screening and behavioral counseling interventions to reduce unhealthy alcohol use in adolescents and adults. JAMA. 2018;320(18):1910. doi: 10.1001/jama.2018.12086. [DOI] [PubMed] [Google Scholar]
- O’Keefe J.H., Bhatti S.K., Bajwa A., DiNicolantonio J.J., Lavie C.J. Alcohol and cardiovascular health: the dose makes the poison…or the remedy. Mayo Clin. Proc. 2014;89(3):382–393. doi: 10.1016/j.mayocp.2013.11.005. [DOI] [PubMed] [Google Scholar]
- Patra J., Taylor B., Irving H., Roerecke M., Baliunas D., Mohapatra S., Rehm J. Alcohol consumption and the risk of morbidity and mortality for different stroke types - a systematic review and meta-analysis. BMC Public Health. 2010;10(1) doi: 10.1186/1471-2458-10-258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- R Core Team. R . R-project.org/; 2021. A Language and Environment for Statistical Computing. [Google Scholar]
- Rehm J., Roerecke M. Reduction of drinking in problem drinkers and all-cause mortality. Alcohol Alcohol. 2013;48(4):509–513. doi: 10.1093/alcalc/agt021. [DOI] [PubMed] [Google Scholar]
- Rehm J., Prieto J.A.A., Beier M., Duhot D., Rossi A., Schulte B., Zarco J., Aubin H.-J., Bachmann M., Grimm C., Kraus L., Manthey J., Scafato E., Gual A. The role of alcohol in the management of hypertension in patients in European primary health care practices - A survey in the largest european union countries. BMC Family Practice. 2016;17(1) doi: 10.1186/s12875-016-0529-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rehm J., Anderson P., Prieto J.A.A., Armstrong I., Aubin H.-J., Bachmann M., Bastus N.B., Brotons C., Burton R., Cardoso M., Colom J., Duprez D., Gmel G., Gual A., Kraus L., Kreutz R., Liira H., Manthey J., Møller L., Okruhlica Ľ., Roerecke M., Scafato E., Schulte B., Segura-Garcia L., Shield K.D., Sierra C., Vyshinskiy K., Wojnar M., Zarco J. Towards new recommendations to reduce the burden of alcohol-induced hypertension in the European Union. BMC Medicine. 2017;15(1) doi: 10.1186/s12916-017-0934-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roerecke M., Kaczorowski J., Tobe S.W., Gmel G., Hasan O.S.M., Rehm J. The effect of a reduction in alcohol consumption on blood pressure: a systematic review and meta-analysis. The Lancet Public Health. 2017;2(2):e108–e120. doi: 10.1016/S2468-2667(17)30003-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roerecke M., Tobe S.W., Kaczorowski J., Bacon S.L., Vafaei A., Hasan O.S.M., Krishnan R.J., Raifu A.O., Rehm J. Sex-specific associations between alcohol consumption and incidence of hypertension: a systematic review and meta-analysis of cohort studies. J. Am. Heart Association. 2018;7(13):e008202. doi: 10.1161/JAHA.117.008202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roubsanthisuk W., Silaruks S., Ophascharoensuk V., et al. Hypertension in thailand: a message from the thai hypertension society on world hypertension day 2017. J. Med. Assoc. Thai. 2018;101:705–706. [Google Scholar]
- Semlitsch T., Jeitler K., Berghold A., et al. Long-term effects of weight-reducing diets in people with hypertension. The Cochrane database of systematic reviews. 2016;3:CD008274. doi: 10.1002/14651858.CD008274.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sornpaisarn B., Shield K., Manthey J., Limmade Y., Low W.Y., Van Thang V.o., Rehm J. Alcohol consumption and attributable harm in middle-income South-East Asian countries: Epidemiology and policy options. Inter. J. Drug Policy. 2020;83:102856. doi: 10.1016/j.drugpo.2020.102856. [DOI] [PubMed] [Google Scholar]
- Taylor B., Irving H.M., Baliunas D., Roerecke M., Patra J., Mohapatra S., Rehm J. Alcohol and hypertension: gender differences in dose-response relationships determined through systematic review and meta-analysis. Addiction. 2009;104(12):1981–1990. doi: 10.1111/j.1360-0443.2009.02694.x. [DOI] [PubMed] [Google Scholar]
- Thai Hypertension Society. Thai Hypertension Guideline, http://www.thaihypertension.org/files/HT guideline 2019.with watermark.pdf (2019, accessed 20 April 2021).
- VanDevanter N., Kumar P., Nguyen N., Nguyen L., Nguyen T., Stillman F., Weiner B., Shelley D. Application of the consolidated framework for implementation research to assess factors that may influence implementation of tobacco use treatment guidelines in the viet nam public health care delivery system. Implementation Science. 2017;12(1) doi: 10.1186/s13012-017-0558-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiemker V., Neufeld M., Bunova A., Danquah I., Ferreira-Borges C., Konigorski S., Rastogi A., Probst C. Digital assessment tools using animation features to quantify alcohol consumption: systematic app store and literature review. J. Medical Internet Research. 2022;24(3):e28927. doi: 10.2196/28927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . Nonthaburi; Thailand: 2019. Hypertension care in thailand: best practices and challenges 2019. [Google Scholar]
- World Health Organization. Global Status Report on Alcohol and Health, https://apps.who.int/iris/rest/bitstreams/1151838/retrieve (2018, accessed 18 March 2022).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data will be made available on request.