Abstract
Existing research proposed that moving from a disorder-level analysis to a symptom-level analysis may provide a more fine-grained understanding of psychopathology. This study aimed to explore the relations between two dimensions (i.e., cognitive reappraisal, CR; expressive suppression, ES) of emotion regulation and individual symptoms of depression and anxiety among medical staff during the late stage of COVID-19 pandemic. We examined depression symptoms, anxiety symptoms and emotion regulation among 420 medical staff during the late stage of COVID-19 pandemic via network analysis. Two networks (i.e. emotion regulation-depression network and emotion regulation-anxiety network) were constructed in the present study. Bridge centrality index was calculated for each variable within the two networks. Among the present sample, the prevalences of depression and anxiety are 39.5% and 26.0%. CR and ES showed distinct connections to symptoms of depression and anxiety. Results of bridge centrality showed that in both networks, CR had a negative bridge expected influence value while ES had a positive bridge expected influence value. The results revealed the specific role of CR and ES in relation to depression and anxiety at a symptom level. Implications for clinical preventions and interventions are discussed.
Keywords: COVID-19 pandemic, Emotion regulation, Depression, Anxiety, Network analysis
1. Introduction
The coronavirus disease 2019 (COVID-19) pandemic has been identified as a public health concern globally, threatening individuals’ physical and mental health (Fiorillo and Gorwood, 2020; Kumar and Nayar, 2021). Serving as crisis management personnel, medical staff are exposed to a high range of occupational risks whose severity and likelihood have increased since the pandemic outbreak (Diktas et al., 2021; El-Boghdadly et al., 2020; Franklin and Gkiouleka, 2021; Veziant et al., 2020). Several well-documented risk factors faced by the medical staff in the workplace during COVID-19 include high workload, direct contact with infected individuals, facing a higher rate of moral dilemmas (e.g., taking decisions about life and death), limited collegial and managerial support, perceived helplessness due to lack of experience or equipment and prolonged separation from families (Gohar et al., 2020; Fang et al., 2021; Shanafelt et al., 2020; Walton et al., 2020; Wang et al., 2020). All of the above had an unprecedented impact on the mental health of medical staff working at the front line of the COVID-19 pandemic response (Lai et al., 2020; Dong et al., 2020; De Kock et al., 2021; Zhao et al., 2022).
Depression and anxiety have been reported as the two mental health conditions most commonly experienced by medical staff during the pandemic, with a pooled prevalence of 28% and 33%, respectively (Luo et al., 2020). Despite the potentially detrimental effects at an individual level (e.g., developing chronic and lifelong mental health conditions), poor mental health among medical staff may further cause a considerable negative impact on patients and the whole health care system. Specifically, poor mental health may contribute to aversive consequences such as making medical errors and an overall deterioration of patient care quality and safety (Goulia et al., 2010; Letvak et al., 2012; Sun et al., 2022). Understanding mechanisms that underlie common mental health problems, such as depression and anxiety, may lead to improvements in early detection and the development of effective intervention strategies. Thereby mitigating the negative mental health impact of the pandemic on medical staff.
An important concept in understanding internalizing disorders, emotion regulation refers to the internal and external processes of monitoring, evaluating, and modifying individuals’ emotional states (Gross, 1998a). Successful emotion regulation is important to affective, social functioning, and overall well-being (John and Gross, 2004). Conversely, failure in emotion regulation is associated with various mental disorders, particularly depression and anxiety (Aldao et al., 2010). Among many different forms of emotion regulation strategies, two of the most common and well-examined strategies are cognitive reappraisal and expressive suppression (Gresham and Gullone, 2012).
Cognitive reappraisal (CR) involves reinterpreting the meaning of a challenging situation in a way that changes its emotional impact (Lazarus and Alferti, 1964; Meyer et al., 2012). As an antecedent-focused emotion regulation strategy, CR typically manifests before the emotional experiences are fully generated (John and Gross, 2004). For example, suppose medical staff are required to stay isolated from their family due to exposure to suspected COVID-19 patients. In that case, the involvement of CR might be in interpreting such a measure as a way to reduce the potential risk of infecting their loved ones rather than an imposed restriction on their freedom of movement. The adoption of CR as a response mechanism to stressful events is associated with reduced negative emotions and physiological arousal and thereby is considered a protective factor against depression and anxiety (Aldao et al., 2010).
Expressive suppression (ES) involves inhibiting outward emotional expression (Gross, 1998b; Meyer et al., 2012). Contrary to CR, ES occurs after emotional experiences have been fully manifested (Gross, 1998b; Meyer et al., 2012). Extending the aforementioned example, medical staff who adopt ES may force themselves to hide their emotions by keeping a neutral facial expression. Frequent use of ES has been associated with elevated negative affect, physiological arousal, and cognitive load (Campbell-Sills et al., 2006; Gross and John, 2003). ES is generally considered a maladaptive emotion regulation strategy associated with an increased risk for depression and anxiety (Aldao et al., 2010). Intriguingly, studies conducted during the pandemic reported mixed findings on the relationship of CR and ES to mental health outcomes (e.g., Li et al., 2022; Sun et al., 2021; Zhu et al., 2021). For example, the frequent use of ES has been associated with reduced negative emotions (Sun et al., 2021), which is at odds with the reportedly maladaptive nature of this emotional regulation strategy. The above calls for further investigation into the role of CR and ES as protective or risk factors in relation to the mental health of medical staff during a highly stressful period of the COVID-19 pandemic, as well as during the post-pandemic era.
Previous studies have commonly examined the relationship between emotion regulation (e.g., CR and ES) and depression/anxiety via the latent variable approach (with depression/anxiety severity indexed by sum-scores of symptoms), which may overlook their relationships at the symptom level (Fried and Nesse, 2015). Emerging research shows that both depression and anxiety are heterogeneous syndromes that manifest via discrete symptoms (Fried and Nesse, 2015). In line with this approach, it has been shown that positive reappraisal is differentially related to individual symptoms of depression and anxiety (Everaert and Joormann, 2019). Neglecting the symptomatic heterogeneity of depression and anxiety may mask the differential relationships between clinically distinct symptoms and emotion regulation strategies, potentially contributing to inconsistent findings across studies.
To address the above-mentioned measurement challenges, we adopted a symptom-based analytical approach, namely, network analysis. From a network analysis perspective, mental disorders emerge from the relations among interacting variables (both symptom and non-symptom) rather than being the consequences of a latent common cause (Borsboom, 2017). Using this approach, emotion regulation strategies and individual psychological symptoms (e.g., depression or anxiety) are depicted as nodes, and potential pathways through which emotion regulation strategies connect to different symptoms are depicted as edges. Hence, network analysis focuses on identifying specific pathways that connect emotion regulation strategies and individual symptoms of depression and anxiety. This stands out from the latent variable model, which focuses on how emotion regulation strategies may impact latent psychopathology constructs (e.g., depression and anxiety measured by symptom sum scores). In addition to delineating emotion regulation–symptom pathways, network analysis offers empirical indices (e.g., bridge expected influence). These novel indices allow researchers to quantify to what extent CR/ES may transmit positive/negative influence (risk and protective ability) to the symptom clusters (Jones et al., 2021).
In this study, we constructed two networks to independently examine the interrelationship between two emotion regulation strategies (i.e., CR and ES) and two disorders (i.e., depression and anxiety) at a symptom level. The aims of the current study are two-fold: 1) to explore potential pathways linking emotion regulation strategies (i.e., CR and ES) to individual symptoms of depression and anxiety; and 2) to measure the risk and protective ability of the CR and ES on depression and anxiety symptom clusters.
2. Method
2.1. Participants
Data were collected between 16 and 18 April 2021 through paper and pencil tests. 458 medical staff from Xijing Hospital participated in Shaanxi Province, China in the study. Only participants who provided informed consent were included in the study. Thirty-eight responses were excluded due to incomplete demographic information (n = 6) or failed the two honesty check items (n = 32). As a result, a total of 420 questionnaires were included in the analysis and the final sample consisted of 199 doctors (females = 130) and 221 nurses (females = 213) aged 22–50 years (mean age = 32.74, SD = 5.37). The Ethics Committee of the First Affiliated Hospital of the Fourth military medical university approved this study (Project No. KY20182047-F-1).
2.2. Measures
2.2.1. Emotion regulation
Emotion regulation was assessed using the Emotion Regulation Questionnaire (ERQ). This is a 10-item self-report measure examining an individual's tendency to use cognitive reappraisal/expressive suppression when regulating their emotions (Gross and John, 2003). The measure has two subscales, namely, Cognitive Reappraisal (6 items) and Expressive Suppression (4 items). Responses ranged from 1 (strongly disagree) to 7 (strongly agree). Following the recommendations by Preece et al. (2020), we used the 10-item form of ERQ to ensure the content validity of the CR subscale. The summed scores of two subscales were of interest to the current study. The internal consistency of CR and ES subscales in this study demonstrated good (α = 0.86) and acceptable (α = 0.76) levels, respectively.
2.2.2. Depression symptoms
We used the Patient Health questionnaire-9 (PHQ-9) scale to assess depression symptoms. This is a 9-item self-report measure examining depression severity. Participants were asked to report the frequency of symptoms they experienced during the past two weeks. Responses ranged from 0 (not at all) to 3 (nearly every day) (Kroenke et al., 2001). Individual symptom-score was the measure of interest for the current study. The scale demonstrated good internal consistency in the current study (α = 0.87).
2.2.3. Anxiety symptoms
We used Generalized anxiety disorder 7-item (GAD-7) Scale to assess anxiety symptoms (Spitzer et al., 2006). This is a 7-item self-report measure examining anxiety severity. Participants were asked to report the frequency of symptoms they experienced during the past two weeks. Responses ranged from 0 (not at all) to 3 (nearly every day). Individual symptom-score was the measure of interest for the current study. The scale demonstrated excellent internal consistency in the current study (α = 0.90).
2.3. Network analysis
Two networks were examined in the current study, namely, the ER-depression and ER-anxiety network. The Graphical LASSO network approach was used to estimate the network structure of the two undirected networks. Within each network, edges represent the partial correlation between two nodes when adjusting the effects coming from all remaining nodes. The networks in the current study were based on Spearman rho correlation. The graphical Least Absolute Shrinkage and Selection Operator (LASSO) technique was used to regularize partial correlations within the represented networks (Friedman et al., 2008). By punishing the trivially small partial correlation coefficients to zero, such a technique helps to remove spurious edges and results in more stable and sparse networks (Epskamp and Fried, 2018; Friedman et al., 2008). The Extended Bayesian Information Criterion (EBIC) hyperparameter γ was set to 0.5 to balance sensitivity and specificity (Epskamp and Fried, 2018; Foygel and Drton, 2010). The layout of the presented networks was based on the Fruchterman-Reingold algorithm (Fruchterman and Reingold, 1991). The R-package qgraph was used to compute the presented networks (Epskamp et al., 2012).
Two communities were pre-defined for the current study, namely, ER (including CR and ES) and symptom communities (including individual depression/anxiety symptoms). Bridge expected influence (the sum of the edge weights connecting a given node to all nodes in the other community) was calculated to identify bridge nodes that link the communities. Bridge expected influence is more suitable than other bridge centrality (e.g., bridge strength and betweenness) for determining bridge nodes in a network with both negative and positive connections (Robinaugh et al., 2016; Jones et al., 2021). A higher bridge expected influence value means a higher likelihood of activating the opposite community (Jones et al., 2021). The bridge expected influence was calculated via the R package networktools (Jones et al., 2021).
The accuracy of edge weights was assessed by plotting the 95% confidence interval (with 2,000 bootstrap samples) for each edge within the presented networks. The stability of bridge expected influence was evaluated by calculating the Correlation Stability (CS)-coefficient via a case-dropping bootstrap approach (with 2,000 bootstrap samples). According to the recommendation (Epskamp et al., 2018), the ideal CS-coefficient is above .5 and should not be below .25. We further conducted bootstrapped difference tests (with 2,000 bootstrap samples) for edge weights and bridge expected influence. The aforementioned procedures were conducted via the R-package bootnet (Epskamp et al., 2018).
3. Results
The prevalence of depression (PHQ-9 ≥ 5) and anxiety (GAD-7 ≥ 5) in the present study is reported to be at 39.5% and 26.0%. Table 1 shows abbreviation, mean scores and standard deviations for each variable selected in the present networks.
Table 1.
Abbreviation, mean scores and standard deviations for each variable selected in the present networks.
| Variables | Abbreviation | M | SD |
| Emotion Regulation | |||
| Cognitive reappraisal | CR | 30.60 | 5.65 |
| Expressive suppression | ES | 15.78 | 4.43 |
| Depression symptoms (PHQ-9) | |||
| PHQ-1: Anhedonia | D1 | 0.70 | 0.63 |
| PHQ-2: Depressed or sad mood | D2 | 0.47 | 0.61 |
| PHQ-3: Sleep difficulties | D3 | 0.58 | 0.68 |
| PHQ-4: Fatigue | D4 | 0.73 | 0.67 |
| PHQ-5: Appetite changes | D5 | 0.43 | 0.62 |
| PHQ-6: Feeling of worthlessness | D6 | 0.38 | 0.60 |
| PHQ-7: Concentration difficulties | D7 | 0.50 | 0.64 |
| PHQ-8: Psychomotor agitation/retardation | D8 | 0.20 | 0.48 |
| PHQ-9: Thoughts of death | D9 | 0.07 | 0.28 |
| Anxiety symptoms (GAD-7) | |||
| GAD-1: Nervousness or anxiety | A1 | 0.49 | 0.65 |
| GAD-2: Uncontrollable worry | A2 | 0.36 | 0.61 |
| GAD-3: Worry too much | A3 | 0.52 | 0.63 |
| GAD-4: Trouble relaxing | A4 | 0.50 | 0.71 |
| GAD-5: Restlessness | A5 | 0.28 | 0.51 |
| GAD-6: Irritable | A6 | 0.59 | 0.63 |
| GAD-7: Afraid something will happen | A7 | 0.23 | 0.47 |
Abbreviations: M, mean; SD, standard deviation
The ER-depression network
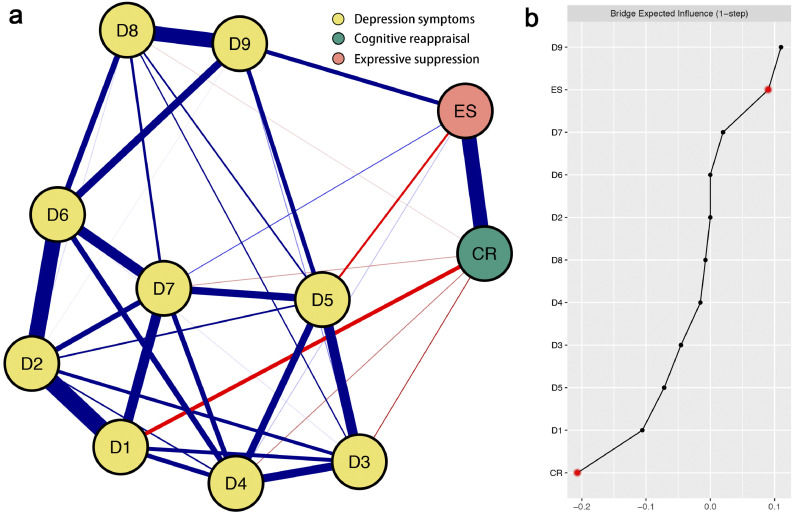
The ER-depression network structure is shown in Fig. 1 a. Four strongest edges are between D1-D2 (weight = 0.35), D2-D6 (weight = 0.32), D8-D9 (weight = 0.30) and CR-ES (weight = 0.30). CR is only negatively linked with five depression symptoms: D1 (weight = -0.11), D3 (weight = -0.05), D4 (weight = -0.03), D7 (weight = -0.02), and D8 (weight = -0.008). ES is positively linked with three depression symptoms: D9 (weight = 0.11), D7 (weight = 0.04) and D4 (weight = 0.01) and negatively linked with one depression symptom: D5 (weight = -0.07). All edge weights within the ER-depression network can be found in Table S1 (in Supplemental Material). The bootstrapped 95% confidence interval is relatively narrow, indicating that the ER-depression is considered to be accurate (Fig. S1 in Supplementary Material). Fig. S2 (in Supplementary Material) shows the bootstrapped difference test for edge weights.
Fig. 1.
Network structure of emotion regulation-depression symptoms. (a) Blue edges represent positive correlations, red edges represent negative correlations. The thickness of the edge reflects the magnitude of the correlation. Cut value = 0.05. (b) Centrality plot depicting the bridge expected influence of each variables in the network (raw value). The text of depression symptoms can be seen in Table 1. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
Fig. 1b depicts the raw value of bridge expected influence for each node within the ER-depression network. The CR's bridge expected influence value is negative (about -0.21), whereas the ES's bridge expected influence value is positive (about 0.09). The CS-coefficient of node bridge expected influence is 0.52, indicating the centrality index (i.e., bridge expected influence) is adequately stable (Fig. S3 in Supplementary Material). Fig. S4 (in Supplementary Material) shows the bootstrapped difference tests for node bridge expected influence.
The ER-anxiety network
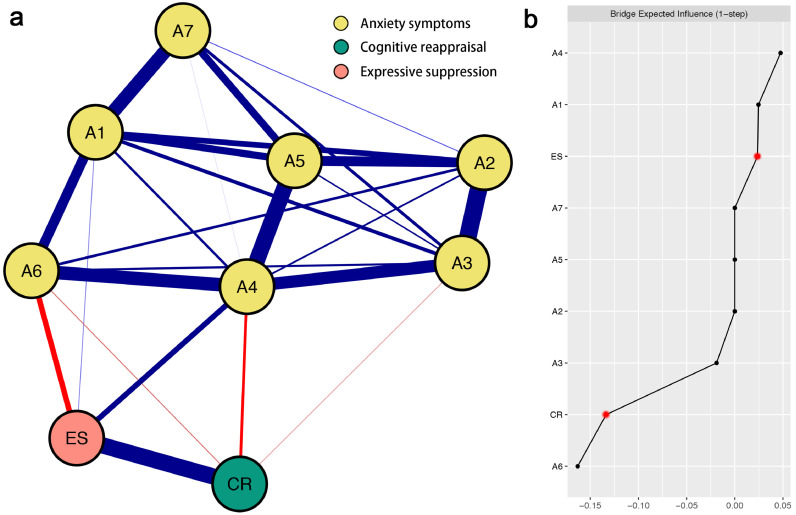
The ER-anxiety network structure is presented in Fig. 2 a. Three strongest edges are between A2-A3 (weight = 0.35), CR-ES (weight = 0.33), and A4-A5 (weight = 0.32). CR is only negatively linked with three anxiety symptoms: A4 (weight = -0.08), A6 (weight = -0.03), and A3 (weight = -0.02). ES is positively linked with two anxiety symptoms: A4 (weight = 0.13) and A1 (weight = 0.02) and negatively linked with one anxiety symptom: A6 (weight = -0.13). All edge weights within the ER-anxiety network can be found in Table S2 (Supplemental Material). Similar to the ER-depression network, the bootstrapped 95% confidence interval plot supported that the edge weights of the ER-anxiety network are accurate (Fig. S5 in Supplementary Material). Fig. S6 (in Supplementary Material) shows the bootstrapped difference test for edge weights.
Fig. 2.
Network structure of emotion regulation-anxiety symptoms. (a) Blue edges represent positive correlations, red edges represent negative correlations. The thickness of the edge reflects the magnitude of the correlation. Cut value = 0.05. (b) Centrality plot depicting the bridge expected influence of each variables in the network (raw value). The text of depression symptoms can be seen in Table 1. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
Fig. 2b depicts the raw value of bridge expected influence for each node within the ER-anxiety network. The CR's bridge expected influence value is negative (about -0.13), whereas the ES's bridge expected influence value is positive (about 0.02). The CS-coefficient of node bridge expected influence is 0.28, which is above the recommended cut-off (Fig. S7 in Supplementary Material). Fig. S8 (in Supplementary Material) shows the bootstrapped difference tests for node bridge expected influence.
4. Discussions
The COVID-19 pandemic has presented unprecedented and sustained psychological threats to medical staff. The current study found that the prevalence rates of depression and anxiety symptoms among Chinese medical staff were 39.5% and 26.0%, respectively. The prevalence rates of both depression and anxiety reported in the current study are higher than in the previous research conducted among Chinese medical staff (35.8% and 24.4%, respectively; Lixia et al., 2022), suggesting a long-lasting psychological impact of the pandemic. To inform proactive prevention and interventions for medical staff, the current study used network analysis to examine how individual differences in emotion regulation may protect against/drive risks for individual symptoms of depression and anxiety. In line with previous research (Fried and Nesse, 2015; Everaert and Joormann, 2019), we found that CR and ES may function differently in relation to specific depression/anxiety symptoms, with several robust pathways being identified. Further, results from bridge centrality analysis supported the protective role of CR and the detrimental role of ES in relation to both depression and anxiety symptoms.
Noteworthy, we found that CR was negatively related to five depression symptoms that capture fatigue (D1 “Anhedonia”, D3 “Sleep difficulties”, D4 “Fatigue”, D8 “Psychomotor agitation/retardation” and D7 “Concentration difficulties”, Maslach and Leiter, 2016). Compared to the general population, the job duties of medical staff may frequently expose them to emotion-eliciting situations that involve moral dilemmas and associated moral stress (Reynolds et al., 2012). Existing research has demonstrated that moral stress is a unique predictor of fatigue symptoms (DeTienne et al., 2012). CR represents the ability to evaluate the emotion-eliciting situation in a way that modifies its aversive impacts (John and Gross, 2004). Hence, when facing moral dilemmas, CR may enable medical staff to reconstruct these situations in a way that increases their perceived self-efficacy in taking appropriate actions, alleviating their moral stress, and further reducing fatigue symptoms.
A strong positive edge was identified between ES and “Thought of death” (D9), indicating that more frequent use of ES is associated with an increased risk of suicidal ideation. Existing research on the relationship between ES and suicidal ideation reported conflicting findings (e.g., Forkmann et al., 2014; Franz et al., 2021; Ghorbani et al., 2017); for example, Franz et al. (2021) found that ES may reduce (rather than increase) the risk for suicidal ideation. Our findings add evidence to this debate and further extend previous findings from clinical populations (i.e., Forkmann et al., 2014; Ghorbani et al., 2017) to medical staff. The acute stressful experience during the pandemic may trigger both suicidal ideation and ES, which may reinforce each other and form a vicious cycle. Specifically, as ES only reduces the outward expression of emotion, the internal negative feelings may persist and accumulate, triggering suicidal thoughts. This may, in turn, promote increased use of ES as a way to inhibit such troubling thoughts. The reciprocal effect between ES and suicidal ideation may be particularly concerning as a high proportion of medical staff relies on self-help when distressed (Søvold et al., 2021). As ES represents one of the most common ways to self-regulate emotions, this may put medical staff at a higher risk for suicidal ideation.
Within the emotion regulation-anxiety network, we found that “Trouble relaxing” (A4) was negatively linked to CR and positively linked to ES. The finding may be explained in several ways. For instance, during the pandemic, medical staff were required to work in high-pressure environments (with potentially ongoing stressful events) for long hours with heavy workloads (Søvold et al., 2021). The intensive working situations may objectively increase feelings of difficulty in relaxing while leaving medical staff with limited time to resolve such feelings. In this context, it may be intuitive for medical staff to engage in more ES and less CR, as it may not be feasible to reinterpret every stressful event while keeping up with job duties. It is also plausible that CR may be more effective than ES in reducing somatic symptoms such as having trouble relaxing. Future research is needed to test both assumptions and ascertain the directionality of these pathways.
It is worth noting that ES was negatively linked to one anxiety symptom “Irritable” (A6), and one depression symptom “Appetite changes” (D5). This may mean that ES could be effective for reducing symptoms such as irritability and appetite changes while heightening risks for other symptoms of depression and anxiety (e.g., “Thought of death” and “Trouble relaxing”). These findings support the notion that risk/protective factors may have substantially different relations with individual symptoms within a disorder (Fried and Nesse, 2015). Such differences are currently neglected by sum-score analysis, which may account for the inconsistent findings across studies.
To quantify the protective or risk ability of CR/ES on depression and anxiety symptoms using network analysis, the bridge expected influence of each network was calculated, respectively. In both ER-depression and ER-anxiety networks, CR has a negative bridge expected influence value while ES has a positive bridge expected influence value, indicating CR may manifest as a protective factor and ES may manifest as a risk factor for depression and anxiety among medical staff. These findings are consistent with previous studies that consider CR and ES as protective and risk factors for depression and anxiety (Aldao et al., 2010) while adding to the evidence of the role of CR and ES during the pandemic.
The current findings have several important implications for the development of early detection and interventional strategies aimed at protecting the mental health of medical staff. First and foremost, by pinpointing the pathway between ES and suicidal ideation, our results suggest that ES may be prioritized as a target for early detection and prevention. Specifically, the stigma around mental illness (e.g., fear of repercussions from employers, health regulators or medical boards) may introduce self-report bias when using symptom-based questionnaires as screening tools. On the other hand, ES-related items are more neutral, thus, less likely to produce concerns such as fear of reprisal during screening. More importantly, as ES may exist independent of symptoms, measuring ES may help identify the at-risk population and provide timely support even before the onset of symptoms. Hence, stakeholders may consider incorporating the ES subscale into the existing occupational health assessment. Further, by demonstrating the protective role of CR and the detrimental role of ES in depression and anxiety, our results suggest that psychoeducation that focuses on promoting the implementation of CR and reducing reliance on ES may be beneficial. Given the high prevalence of depression and anxiety symptoms among medical staff, such programs are urgently needed to reduce short-term and long-term adverse psychological impacts. Last, by showing the differential relationships between emotion regulation strategies and psychological symptoms, our results may inform the development of personalized prevention and intervention strategies that recognize symptom heterogeneity.
Despite the novelty of the current findings, several limitations warrant consideration. First, the utilization of cross-sectional data restricted us from confirming the direction of causality. Future research is needed to ascertain whether emotion regulation strategies influence/are influenced by symptoms of depression and anxiety or if external situations may elicit both symptoms and emotion regulation strategies. Second, the network structure observed in the current study may be specific to the questionnaires we employed and may not be replicable when the constructs are measured using different scales. Nevertheless, all study measures are widely adopted and validated in diverse settings. Third, the emotion regulation-symptom networks reflect between-subject effects on a group level, which may not capture within-person processes. Idiographic network analysis using intensive longitudinal data may facilitate the understanding of emotion regulation-symptom relations within an individual. Fourth, given the difference in health care systems between China and other countries, future research involving medical staff from different countries is needed to examine the generalizability of the reported findings.
5. Conclusion
The current study used network analysis to understand the symptomatic interplay between emotion regulation strategies and depression and anxiety among medical staff during the pandemic. Our findings highlight the protective role of CR and the detrimental role of ES and outline the pathways through which these emotion regulation strategies may interact with symptoms of depression and anxiety. These findings may facilitate the development of early detection and intervention strategies to mitigate the adverse impact of the pandemic on the mental health of medical staff.
Author statement
Role of funding
This study was supported by the Fourth Military Medical University (2021JSTS30, BWS16J012).
CRediT authorship contribution statement
Shuyi Liang: Visualization, Writing – original draft. Chang Liu: Writing – original draft. Kristian Rotaru: Writing – original draft. Kuiliang Li: Visualization, Data curation, Formal analysis, Investigation. Xinyi Wei: Data curation, Formal analysis, Investigation. Shangqing Yuan: Data curation, Formal analysis, Investigation. Qun Yang: Data curation, Formal analysis, Investigation. Lei Ren: Visualization, Data curation, Formal analysis, Investigation, Writing – original draft. Xufeng Liu: Visualization, Data curation, Formal analysis, Investigation.
Declaration of Competing Interest
The authors have no conflicts of interest to declare.
Acknowledgements
We would like to thank all the individuals who participated in the study. We also thank all the administrative staff and doctors in the hospital who help us with the recruitment.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.psychres.2022.114863.
Appendix. Supplementary materials
References
- Aldao A., Nolen-Hoeksema S., Schweizer S. Emotion-regulation strategies across psychopathology: a meta-analytic review. Clin. Psychol. Rev. 2010;30(2):217–237. doi: 10.1016/j.cpr.2009.11.004. [DOI] [PubMed] [Google Scholar]
- Borsboom D. A network theory of mental disorders. World Psychiatry. 2017;16(1):5–13. doi: 10.1002/wps.20375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell-Sills L., Barlow D.H., Brown T.A., Hofmann S.G. Acceptability and suppression of negative emotion in anxiety and mood disorders. Emotion. 2006;6(4):587–595. doi: 10.1037/1528-3542.6.4.587. [DOI] [PubMed] [Google Scholar]
- De Kock J.H., Latham H.A., Leslie S.J., Grindle M., Munoz S.A., Ellis L., Polson R., O'Malley C.M. A rapid review of the impact of COVID-19 on the mental health of healthcare workers: implications for supporting psychological well-being. BMC Public Health. 2021;21(1):104. doi: 10.1186/s12889-020-10070-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeTienne D.R., McKelvie A., Chandler G.N. Academy of Management Proceedings.; Boston, MA: 2012. The impact of Motivation, Innovation and Causation and Effectuation Approaches on Exit Strategies. [Google Scholar]
- Diktas H., Oncul A., Tahtasakal C.A., Sevgi D.Y., Kaya O., Cimenci N., Dokmetas I. What were the changes during the COVID-19 pandemic era concerning occupational risks among health care workers? J. Infect. Public Health. 2021;14(10):1334–1339. doi: 10.1016/j.jiph.2021.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong Z.Q., Ma J., Hao Y.N., Shen X.L., Liu F., Gao Y., Zhang L. The social psychological impact of the COVID-19 pandemic on medical staff in China: a cross-sectional study. Eur. Psychiatry. 2020;63(1):e65. doi: 10.1192/j.eurpsy.2020.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El-Boghdadly K., Wong D., Owen R., Neuman M.D., Pocock S., Carlisle J.B., Johnstone C., Andruszkiewicz P., Baker P.A., Biccard B.M., Bryson G.L., Chan M., Cheng M.H., Chin K.J., Coburn M., Jonsson Fagerlund M., Myatra S.N., Myles P.S., O'Sullivan E., Pasin L., Ahmad I. Risks to healthcare workers following tracheal intubation of patients with COVID-19: a prospective international multicentre cohort study. Anaesthesia. 2020;75(11):1437–1447. doi: 10.1111/anae.15170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epskamp S., Borsboom D., Fried E.I. Estimating psychological networks and their accuracy: a tutorial paper. Behav. Res Methods. 2018;50(1):195–212. doi: 10.3758/s13428-017-0862-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epskamp S., Cramer A., Waldorp L., Schmittmann V., Borsboom D. qgraph: network visualizations of relationships in psychometric data. J. Stat. Softw. 2012;48(4):1–18. doi: 10.18637/jss.v048.i04. [DOI] [Google Scholar]
- Epskamp S., Fried E.I. A tutorial on regularized partial correlation networks. Psychol. Methods. 2018;23(4):617–634. doi: 10.1037/met0000167. [DOI] [PubMed] [Google Scholar]
- Everaert J., Joormann J. Emotion regulation difficulties related to depression and anxiety: a network approach to model relations among symptoms, positive reappraisal, and repetitive negative thinking. Clin. Psychol. Sci. 2019;7(6):1304–1318. doi: 10.1177/2167702619859342. [DOI] [Google Scholar]
- Fang X.H., Wu L., Lu L.S., Kan X.H., Wang H., Xiong Y.J., Ma D.C., Wu G.C. Mental health problems and social supports in the COVID-19 healthcare workers: a Chinese explanatory study. BMC Psychiatry. 2021;21(1):34. doi: 10.1186/s12888-020-02998-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiorillo A., Gorwood P. The consequences of the COVID-19 pandemic on mental health and implications for clinical practice. Eur. Psychiatry. 2020;63(1):e32. doi: 10.1192/j.eurpsy.2020.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forkmann T., Scherer A., Böcker M., Pawelzik M., Gauggel S., Glaesmer H. The relation of cognitive reappraisal and expressive suppression to suicidal ideation and suicidal desire. Suicide Life Threat. Behav. 2014;44(5):524–536. doi: 10.1111/sltb.12076. [DOI] [PubMed] [Google Scholar]
- Foygel R., Drton M. Extended bayesian information criteria for gaussian graphical models. Advances in Neural Information Processing Systems. 2010;23 [Google Scholar]
- Franklin P., Gkiouleka A. A scoping review of psychosocial risks to health workers during the Covid-19 pandemic. Int. J. Environ. Res. Public Health. 2021;18(5):2453. doi: 10.3390/ijerph18052453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franz P., Kleiman E., Nock M., Franz P., Hall J. Reappraisal and suppression each moderate the association between stress and suicidal ideation: preliminary evidence from a daily diary study. Cogn. Therapy Res. 2021;45:1120–1127. doi: 10.1007/s10608-021-10214-8. [DOI] [Google Scholar]
- Friedman J., Hastie T., Tibshirani R. Sparse inverse covariance estimation with the graphical lasso. Biostatistics. 2008;9(3):432–441. doi: 10.1093/biostatistics/kxm045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fried E.I., Nesse R.M. Depression is not a consistent syndrome: An investigation of unique symptom patterns in the STAR*D study. J. Affect. Disord. 2015;172:96–102. doi: 10.1016/j.jad.2014.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fruchterman T.M.J., Reingold E.M. Graph drawing by force-directed placement. Softw. Pract. Exp. 1991;21:1129–1164. doi: 10.1002/spe.4380211102. [DOI] [Google Scholar]
- Ghorbani F., Khurasan V., Sharifi Bastan F., Jamaati Ardakani R. The alexithymia, emotion regulation, emotion regulation difficulties, positive and negative effects, and suicidal risk in alcohol-dependent outpatients. Psychiatry Res. 2017;252:223–230. doi: 10.1016/j.psychres.2017.03.005. [DOI] [PubMed] [Google Scholar]
- Gohar B., Larivière M., Nowrouzi-Kia B. Sickness absence in healthcare workers during the COVID-19 pandemic. Occup. Med. (Lond.) 2020;70(5):338–342. doi: 10.1093/occmed/kqaa093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goulia P., Mantas C., Dimitroula D., Mantis D., Hyphantis T. General hospital staff worries, perceived sufficiency of information and associated psychological distress during the A/H1N1 influenza pandemic. BMC Infect. Dis. 2010;10:322. doi: 10.1186/1471-2334-10-322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gresham D., Gullone E. Emotion regulation strategy use in children and adolescents: the explanatory roles of personality and attachment. Pers. Individ Dif. 2012;52(5) doi: 10.1016/j.paid.2011.12.016. [DOI] [Google Scholar]
- Gross J.J. The emerging field of emotion regulation: an integrative review. Rev. Gen. Psychol. 1998;3(2):271–299. doi: 10.1016/j.paid.2011.12.016. [DOI] [Google Scholar]
- Gross J.J. Antecedent- and response-focused emotion regulation: divergent consequences for experience, expression, and physiology. J. Pers. Soc. Psychol. 1998;74(1):224–237. doi: 10.1037/0022-3514.74.1.224. [DOI] [PubMed] [Google Scholar]
- Gross J.J., John O.P. Individual differences in two emotion regulation processes: implications for affect, relationships, and well-being. J. Pers. Soc. Psychol. 2003;85(2):348–362. doi: 10.1037/0022-3514.85.2.348. [DOI] [PubMed] [Google Scholar]
- John O.P., Gross J.J. Healthy and unhealthy emotion regulation: personality processes, individual differences, and life span development. J. Pers. 2004;72(6):1301–1333. doi: 10.1111/j.1467-6494.2004.00298.x. [DOI] [PubMed] [Google Scholar]
- Jones P.J., Ma R., McNally R.J. Bridge centrality: a network approach to understanding comorbidity. Multivariate Behav. Res. 2021;56(2):353–367. doi: 10.1080/00273171.2019.1614898. [DOI] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B. The PHQ-9: validity of a brief depression severity measure. J. Gen. Intern. Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar A., Nayar K.R. COVID 19 and its mental health consequences. J. Ment. Health. 2021;30(1):1–2. doi: 10.1080/09638237.2020.1757052. [DOI] [PubMed] [Google Scholar]
- Lai J., Ma S., Wang Y., Cai Z., Hu J., Wei N., Wu J., Du H., Chen T., Li R., Tan H., Kang L., Yao L., Huang M., Wang H., Wang G., Liu Z., Hu S. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw. Open. 2020;3(3) doi: 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lazarus R.S., Alferti E. Short-circuiting of threat by experimentally cognitive appraisal. J. Abnorm. Psychol. 1964;69:195–205. doi: 10.1037/h0044635. [DOI] [PubMed] [Google Scholar]
- Letvak S., Ruhm C.J., McCoy T. Depression in hospital-employed nurses. Clin. Nurse Spec. 2012;26(3):177–182. doi: 10.1097/NUR.0b013e3182503ef0. [DOI] [PubMed] [Google Scholar]
- Li N., Fan L., Wang Y., Wang J., Huang Y. Risk factors of psychological distress during the COVID-19 pandemic: the roles of coping style and emotional regulation. J. Affect. Disord. 2022;299:326–334. doi: 10.1016/j.jad.2021.12.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lixia W., Xiaoming X., Lei S., Su H., Wo W., Xin F., Jianmei C., Qi Z., Ming A., Li K. A cross-sectional study of the psychological status of 33,706 hospital workers at the late stage of the COVID-19 outbreak. J. Affect. Disord. 2022;297:156–168. doi: 10.1016/j.jad.2021.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo M., Guo L., Yu M., Jiang W., Wang H. The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and general public - a systematic review and meta-analysis. Psychiatry Res. 2020;291 doi: 10.1016/j.psychres.2020.113190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer T., Smeets T., Giesbrecht T., Merckelbach H. The efficiency of reappraisal and expressive suppression in regulating everyday affective experiences. Psychiatry Res. 2012;200(2-3):964–969. doi: 10.1016/j.psychres.2012.05.034. [DOI] [PubMed] [Google Scholar]
- Maslach C., Leiter M.P. Stress: Concepts, Cognition, Emotion, and Behavior. Academic Press; Cambridge: 2016. Burnout; pp. 351–357. [Google Scholar]
- Preece D.A., Becerra R., Robinson K., Gross J.J. The emotion regulation questionnaire: psychometric properties in general community samples. J. Pers. Assess. 2020;102(3):348–356. doi: 10.1080/00223891.2018.1564319. [DOI] [PubMed] [Google Scholar]
- Reynolds S.J., Owens B.P., Rubenstein A.L. Moral stress: Considering the nature and effects of managerial moral uncertainty. J. Bus. Ethics. 2012;106(4):491–502. doi: 10.1007/s10551-011-1013-8. [DOI] [Google Scholar]
- Robinaugh D.J., Millner A.J., McNally R.J. Identifying highly influential nodes in the complicated grief network. J. Abnorm. Psychol. 2016;125(6):747–757. doi: 10.1037/abn0000181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shanafelt T., Ripp J., Trockel M. Understanding and addressing sources of anxiety among health care professionals during the COVID-19 pandemic. JAMA. 2020;323(21):2133–2134. doi: 10.1001/jama.2020.5893. [DOI] [PubMed] [Google Scholar]
- Søvold L.E., Naslund J.A., Kousoulis A.A., Saxena S., Qoronfleh M.W., Grobler C., Munter L. Prioritizing the mental health and well-being of healthcare workers: an urgent global public health priority. Front. Public Health. 2021;9 doi: 10.3389/fpubh.2021.679397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer R.L., Kroenke K., Williams J.B., Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch. Intern. Med. 2006;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Sun J., Sarfraz M., Ivascu L., Iqbal K., Mansoor A. How did work-related depression, anxiety, and stress hamper healthcare employee performance during COVID-19? The mediating role of job burnout and mental health. Int. J. Environ. Res. Public Health. 2022;19(16):10359. doi: 10.3390/ijerph191610359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun X., Xie F., Chen B., Shi P., Shen S., Chen Z., Yuan Y., Zhang M., Qin X., Liu Y., Wang Y., Dai Q. Negative emotions in Chinese frontline medical staff during the early stage of the COVID-19 epidemic: status, trend, and influential pathways based on a national investigation. Front. Psychiatry. 2021;12 doi: 10.3389/fpsyt.2021.567446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Veziant J., Bourdel N., Slim K. Risks of viral contamination in healthcare professionals during laparoscopy in the Covid-19 pandemic. J. Visc. Surg. 2020;157(3/1):S59–S62. doi: 10.1016/j.jviscsurg.2020.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walton M., Murray E., Christian M.D. Mental health care for medical staff and affiliated healthcare workers during the COVID-19 pandemic. Eur. Heart J. Acute Cardiovasc. Care. 2020;9(3):241–247. doi: 10.1177/2048872620922795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang J., Zhou M., Liu F. Reasons for healthcare workers becoming infected with novel coronavirus disease 2019 (COVID-19) in China. J. Hosp. Infect. 2020;105(1):100–101. doi: 10.1016/j.jhin.2020.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao S., Long F., Wei X., Tuo J., Wang H., Ni X., Wang X. The effect of regional factors on the mental health status of frontline nurses and patients with COVID-19 during COVID-19: the role of depression and anxiety. Front Public Health. 2022;10 doi: 10.3389/fpubh.2022.857472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu Y., Wang H., Wang A. An evaluation of mental health and emotion regulation experienced by undergraduate nursing students in China during the COVID-19 pandemic: a cross-sectional study. Int. J. Ment. Health Nurs. 2021;30(5):1160–1169. doi: 10.1111/inm.12867. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.