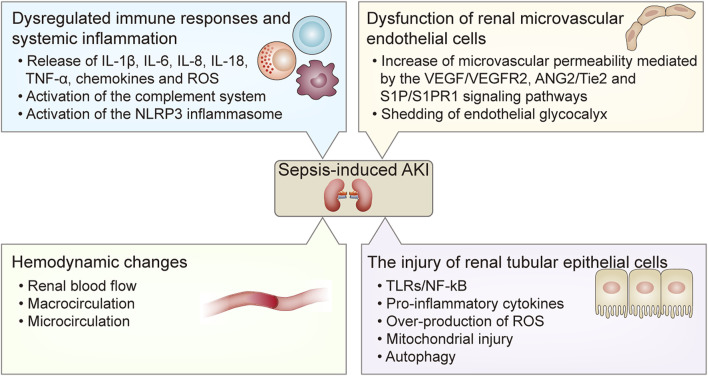
FIGURE 1.
The pathogenesis of sepsis-induced AKI. The pathogenesis of sepsis-induced AKI includes 1) dysregulated immune responses and systemic inflammation including the release of pro-inflammatory cytokines such as IL-1β, IL-6, IL-8, IL-18, TNF-α, chemokines and ROS, and the activation of the complement system and the NLRP3 inflammasome; 2) hemodynamic changes including alterations of renal blood flow, macrocirculation and microcirculation; 3) dysfunction of renal microvascular endothelial cells including increased microvascular permeability mediated by the VEGF/VEGFR2, ANG2/Tie2, and S1P/S1PR1 signaling pathways, and shedding of endothelial glycocalyx; 4) the injury of renal tubular epithelial cells mediated by the TLRs/NF- κB signaling pathway and reduced autophagy at the late stage of sepsis, which result in the release of pro-inflammatory cytokines and over-production of ROS and mitochondrial injury. AKI, acute kidney injury; IL, interleukin; TNF-α, tumor necrosis factor-α; ROS, reactive oxygen species; NLRP3, nucleotide-binding oligomerization domain-like receptor protein 3; VEGF, vascular endothelial growth factor; VEGFR2, VEGF receptor 2; ANG2, Angiopoietin 2; TLRs, Toll-like receptors; NF- κB, nuclear factor kappa B.