Abstract
Early investigations of subjective well-being responses to the COVID-19 pandemic indicated average deterioration but also high variability related to vulnerability of population groups and pandemic phase. Thus, we aimed to gain new insights into the characteristics of certain groups and their differences in subjective well-being response patterns over time. First, we performed Latent Class Analyses with baseline survey data of 2,137 adults (mean age = 40.98, SD = 13.62) derived from the German CORONA HEALTH APP Study to identify subgroups showing similarity of a comprehensive set of 50 risk and protective factors. Next, we investigated the course of quality of life (QoL) as an indicator of subjective well-being grouped by the identified latent classes from July 2020 to July 2021 based on monthly and pandemic phase averaged follow-up survey data by means of Linear Mixed-Effects Regression Modeling. We identified 4 latent classes with distinct indicators and QoL trajectories (resilient, recovering, delayed, chronic) similar to previous evidence on responses to stressful life events. About 2 out of 5 people showed a resilient (i.e., relative stability) or recovering pattern (i.e., approaching pre-pandemic levels) over time. Absence of depressive symptoms, distress, needs or unhealthy behaviors and presence of adaptive coping, openness, good family climate and positive social experience were indicative of a resilient response pattern during the COVID-19 pandemic. The presented results add knowledge on how to adapt and enhance preparedness to future pandemic situations or similar societal crises by promoting adaptive coping, positive thinking and solidary strategies or timely low-threshold support offers.
Supplementary Information
The online version contains supplementary material available at 10.1007/s12144-022-03628-4.
Keywords: Quality of life, COVID-19, Latent class analysis, Longitudinal, Resilience, Coping
The ongoing COVID-19 pandemic represents a global crisis with consequences on the everyday lives and well-being of people from various ages, social and economic contexts (Vindegaard & Benros, 2020). On behalf of restriction measures to combat the spreading of the SARS-CoV-2 virus, people were challenged by changes in lifestyle, structure and routine (e.g., home office, home schooling, travel, nutrition and physical activity), insecurity and worries about health, financials and caregiving, over a considerable period of time (El Keshky et al., 2020; Prime et al., 2020). Thus, it has been discussed that people’s quality of life (QoL; i.e., subjective evaluations of and satisfaction with multiple life domains, most commonly comprising a physical, mental, social, and environmental dimension; Haas, 1999) is at risk of suffering and that there is the urgent need to address questions on how to mitigate maladaptive coping and long-lasting health consequences not only for survivors, families, and health care workers but the general population (Bryson, 2021; Ogueji et al., 2021).
A closer look at currently published results on peoples’ QoL suggests an average small to moderate decrease soon after the outbreak of the COVID-19 pandemic but also high variability between different samples and contexts (Herrera et al., 2021; Koivunen et al., 2022; Park et al., 2021; Rogers et al., 2021; van de Weijer et al., 2022). Results on the long-term development of QoL during the COVID-19 pandemic is fragmentary, so far. One study comparing the QoL during the initial phase of the COVID-19 pandemic with 8 months later observed a trend towards the approximation to average population levels for some domains (e.g., cognitive functioning, depressive symptoms) while others remained persistently worse (e.g., physical functioning, fatigue) (Rogers et al., 2021). This finding is supported by investigations on mental health outcomes indicating a temporary increase of certain psychopathological symptoms at the onset of the COVID-19 pandemic followed by a decrease to almost pre-pandemic levels for many people (Robinson et al., 2022; Vindegaard & Benros, 2020). Since the publication rate on COVID-19-related effects on the general population decreased after the first wave and most of the actual evidence refers to the initial phase of the pandemic, there is an ongoing need to further monitor the development and trend over time to identify phase-dependent or long-lasting effects (Mauz et al., 2022).
Notwithstanding the insufficient number of longitudinal population studies based on randomly drawn representative samples (Mauz et al., 2022; Vindegaard & Benros, 2020), there seems to be an agreement across studies on vulnerable groups that should be paid particular attention to. As proposed by the Vulnerability-Stress Theory (Rutter, 2006), the way people respond to stress is related to genetically determined, socially neglected or learned predispositions (i.e., vulnerabilities). In the face of a stressful life event, vulnerabilities can increase the risk of health deterioration and psychopathology (Rutter, 2006). However, it has to be considered that risk-enhancing factors do not occur isolated but interact with co-occurring risk-reducing factors (e.g., social support) and the strength of risk tends to vary across situations, life circumstances or stages (Lazarus, 1966). Hence, it is important to consider various potentially relevant factors at the same time. In the current pandemic situation, female sex, young adult age, pre-existing health conditions, pessimism, working in healthcare, job loss and financial insecurity, living alone or feelings of loneliness, COVID-19 infected relatives and health concerns were among the most frequently observed risk-enhancing factors for QoL limitations among people from various regions of the world (Algahtani et al., 2021; El Keshky et al., 2020; Epifanio et al., 2021; Gibson et al., 2021; Koivunen et al., 2022).
Resilience, on the contrary, describes the maintenance of subjective well-being and functioning over time (i.e., relatively stable trajectory) and as compared to others facing a comparable level of adversity (Bonanno, 2004). Despite inter-individual diversity in the presence of risk-enhancing and -reducing factors, resilience theory suggests shared mechanisms involved in the processing of a stressful life event (Mancini & Bonanno, 2009). The initial appraisal of the experience (e.g., as personally meaningful, threatening or overwhelming), availability of resources (e.g., social support or personal competencies) and coping strategy (e.g., emotion- or problem-focused) represent crucial mechanisms for adjustment and along the pathway to resilience (see Transactional Stress and Coping Theory, Lazarus & Folkman, 1984, and Individual Differences Model, Mancini & Bonanno, 2009). Coping has been conceptualized as both, a relatively stable (trait-like) tendency or style as well as a (situation-specific) dynamic process initiated by personally significant experience of harm or threat (Lazarus, 1993). One theoretically sound and empirically validated way to define and operationalize coping strategies is to differentiate between emotion-focused (i.e., regulation of negative emotional reactions), problem-focused (i.e., attempts to solve the problem), meaning-focused (i.e., positive reappraisal and acceptance) and support-focused (i.e., seeking instrumental and emotional support) coping (Folkman & Moskowitz, 2004, 2007). Specific situational characteristics of the COVID-19 pandemic and the corresponding restriction measures to combat the spreading of the SARS-CoV-2 virus are limitations of certainty, controllability and avoidability, which most probably affected the pursuit of coping responses and availability of resources. From stress response theory (Skinner & Zimmer-Gembeck, 2011) and investigations of comparable unavoidable stressful situations with limited control (e.g., chronic illness; Roesch & Weiner, 2001), we already know that certain coping efforts can be hampered and thus the risk of maladaptive coping increases. First investigations on coping responses to the COVID-19 pandemic moreover highlighted the level of perceived risk for self-protective or risk-taking behaviors (Gan & Fu, 2022; Motta Zanin et al., 2020). Additionally, availability of social resources such as face-to-face meetings and support systems (e.g., counselling) were also hampered due to stay-at-home-orders and people were challenged to compensate and were at higher risk of feelings of loneliness (Marroquín et al., 2020). Thus, it is important to enhance the understanding of reactivity and characteristics of resilient response patterns under the situational demanding circumstances of the COVID-19 pandemic.
Overall, there is mounting evidence suggesting that the majority of individuals respond in a resilient manner to stressful life events (35–65%; i.e., relatively stable high level, Bonanno et al., 2011). In addition to a resilient responding, the responses to stressful life events over time seem to follow a prototypical pattern of either recovering (15–25%; i.e., temporary decrease and gradual return), chronic (5–30%; i.e., persistently low level) or delayed (0–15%; i.e., steeper decrease and slower recovery) (Bonanno et al., 2011; Mancini & Bonanno, 2009). Some research also observed a response pattern that can be characterized as improving (i.e., temporary relief or lasting increase), for instance, after divorce or chronic illness (Bonanno et al., 2011; Mancini et al., 2011). While originating from studies addressing samples with a history of mental illness, the pattern seems to hold also true for well-being trajectories of the general population (Mancini et al., 2011). Large population-based studies yielded results that speak in favor of inter- as well as intra-individual heterogeneity in well-being responses to stressful life events with some people returning quickly to a set-point, as is a relatively stable personal baseline level (i.e., recovering pattern), while others do not (i.e., delayed pattern) and with some events raising the risk of permanent change (e.g., unemployment, financial deterioration) while others do not (e.g., divorce, job change) (Hentschel et al., 2017; Lucas, 2007; Luhmann et al., 2012). Therefore, in investigations on reactivity to stressful life events it is essential to consider both change and stability and to differentiate the trajectories over time by means of between- and within-person level comparison (Lucas, 2007; Mancini et al., 2011). Apart from the effects of type of event (Hentschel et al., 2017; Lucas, 2007; Luhmann et al., 2012) and controllability (Schwarzer & Schulz, 2003), it should be noted that the permanency (Hentschel et al., 2017) or repeated exposition (Luhmann & Eid, 2009) and possible experience of both positive and negative characteristics (Luhmann et al., 2012) are essential for investigations on stress responses in general and during the COVID-19 pandemic, in particular.
One promising method to identify population groups of similar health or well-being profiles, is a person-centered approach, such as the Latent Class Analysis (LCA; Eid, 2018). LCA particularly aims at detecting unobserved (latent) groups with shared characteristics and allows the simultaneous consideration of a large number of possible indicators (Collins & Lanza, 2009). This is particularly advantageous in view of the rather fragmentary evidence on risk factors during the COVID-19 pandemic. Accordingly, LCA has been increasingly applied in the context of crises and resilience research (Bonanno et al., 2011; Mancini & Bonanno, 2009; Mancini et al., 2011).
Study rationale
The present study aimed to add insights to the previously incomplete and scarce knowledge of quality-of-life trajectories by looking at a one-year period marked by the COVID-19 pandemic and by considering an extensive selection of relevant situation-specific and general risk-increasing and risk-reducing factors. The leading research aim was to identify a resilient response pattern (i.e., stability of QoL over time) and distinct indicators of such a pattern. This information is highly valuable for public health protection, promotion and preparedness in case of the current COVID-19 pandemic and future similar situations. With reference to previous investigations of response patterns in the face of diverse stressful life events (Bonanno et al., 2011; Mancini et al., 2011) as well as in the past SARS (Bonanno et al., 2008) or the initial SARS-CoV-2 pandemic situation (Pierce et al., 2021; Shilton et al., 2021; Truskauskaite-Kuneviciene et al., 2021; Yalçın et al., 2022), we expected to find 3 to 5 different response patterns comprising one resilient subgroup.
Methods
Sample and Procedure
The present analyses are based on data derived from the CORONA HEALTH App Study collected from July 2020 to July 2021 (Beierle et al., 2021). The study addressed voluntary participants of at least 18 years of age recruited via the project partners’ institutional homepages and social media channels, mailing lists and media reports. We combined a cross-sectional (comprehensive baseline questionnaire) with a longitudinal design (reduced follow-up questionnaires), accompanied by a smartphone-delivered collection of data regarding communication app usage and the sensing of the GPS location at the time of answering the survey. After completing the baseline survey, participants were invited to answer follow-up surveys on a weekly basis. Participation could be cancelled, paused, and resumed at any time. With reference to the present analyses’ objectives (identification and tracing of QoL response patterns; see Study Rational), we considered self-report (survey) data, only. Moreover, the present analyses cover a data collection period of one year including phases of relaxation of the spreading of the SARS-CoV-2 virus after the second wave (July 2020 to October 2020, “pre lockdown”), intensification of infection rates and restriction measures during the third wave (November 2020 to March 2021, “lockdown”), followed by further relaxation of infection rates and restriction measures thereafter (April to July 2021, “post lockdown”) in Germany.
The original data base included 2,156 voluntary adult participants. Inspection of the plausibility of answers (e.g., correspondence between similar items), careless responding (straightlining and intraindividual response variability) and extreme outliers (Mahalanobis distance, Cook’s distance) led to the exclusion of 19 participants and a final sample size of 2,137 adults with an age range from 18 to 84 years (52.1% female, 47.3% male, 0.7% other; mean age = 40.98, SD = 13.62). 55% (N = 1,178; 55.0% female, 44.2% male, 0.7% other; mean age = 46.49, SD = 13.46) participated in the longitudinal part, with 2.3 times a month on average (SD = 1.30). The total number of answered questionnaires was n = 9,502 with a monthly average of n = 731 (SD = 291.71). Although the female to male ratio was relatively balanced, the sample was constituted of less old (60 years and older) and low educated (no school leaving certificate or primary education) participants. Table S1 in the Supplementary Materials presents more detailed sample characteristics for all variables under study.
Measures
Outcome
We used the EUROHIS-QOL-8-item index (Schmidt et al., 2005; e.g., satisfaction with personal relations, living conditions, ability to manage daily life) answered on a 5-point rating scale from 1 (very bad) to 5 (very good) to asses quality of life (see Table S1 in the Supplementary Materials). The internal consistency was α = 0.84.
Indicators
As a standardized measure of psychopathological symptoms, we used the depression (9 items, e.g., little interest or pleasure in doing things; α = 0.90), general anxiety (7 items, e.g., not being able to stop or control worrying; α = 0.85) and short panic module (i.e., having a panic attack) of the Patient Health Questionnaire (PHQ-D; Löwe et al., 2002; Spitzer et al., 1999). We further used the standardized items of the PHQ-D (Löwe et al., 2002; Spitzer et al., 1999) psychosocial distress module (10 items, e.g., having no one to discuss problems with; α = 0.78) and experience of violence (e.g., being hit, kicked, or otherwise physically hurt). The 7-item version of the Insomnia Severity Index (ISI-7, Bastien et al., 2001; e.g., problems sleeping through; α = 0.91) was answered to indicate sleep problems. Loneliness was measured with the 3-item SOEP Loneliness Scale (LS-S, Richter & Weinhardt 2013; e.g., missing the company of others; α = 0.81). To measure the Big Five personality dimensions, we used the 10-item Big Five Inventory (BFI-10, Rammstedt et al., 2017; e.g.complete tasks thoroughly) comprising 2 items for each of the dimensions of openness, conscientiousness, extraversion, agreeableness, neuroticism (inter-item correlations were r = .82, 0.84, 0.83, 0.73, 0.75). As an indicator of situational coping strategy, we used the 28-item Brief-Cope Questionnaire (Carver, 1997) comprising 2 items for each of the 14 dimensions (e.g., denial, planning, humor). The dimensions were summarized to 4 latent factors (problem-focused, escape-avoidant-focused, meaning-focused and support-focused coping; α = 0.76, 0.72, 0.73, 0.83) in line with previous findings (Knoll et al., 2005) and as suggested by Carver (1997) based on Exploratory and Confirmatory Factor Analyses(Cohrdes et al., in revision). Subjective health, chronic conditions and health limitations were assessed via the first three items of the Mini European Health Module (MEHM, Cox et al., 2009; inter-item correlations were r = 0.43, 0.56). Stigmatization expectance and experience were assessed by 4 items adopted from the German version of the Inventory of Stigmatizing Experience (ISE, Schulze et al., 2009; e.g., observed or experienced teasing, bullying, or harassment because of COVID-19; inter-item correlations were r = 0.59, 0.51). Scoring procedures and cut-offs were followed according to the instructions of respective manuals (see Table S1 of the Supplementary Materials for further details).
In addition, several in-house developed items were included as indicators of COVID-19-related worries (infecting oneself or other people, becoming severely ill, lack of medical supplies) or job constraints (short-term work, closing of workplace or childcare facilities, quarantine), a current COVID-19 infection (oneself, relatives) and COVID-19-related death of relatives, financial loss, home-office, relevant sociodemographic characteristics (partnership status, household size, children, family climate, living conditions, working as healthcare professional), self-reported lifetime diagnosis of mental disorder, current psychotherapy, health behavior (physical activity, alcohol consumption), needs (e.g., instrumental or psychosocial support) and positive effects (e.g., societal cohesion or solidarity).
Covariates
The participant’s age group (18–29, 30–44, 45–59, 60 + years), sex (female, male, other), and educational level (low = no school-leaving certificate or primary education [German “Hauptschulabschluss”], moderate = secondary education [German “Realschulabschluss” or “Fachabitur”], high = high school graduation [German “Abitur”]) were included as covariates in the analyses.
Table S1 in the Supplementary Materials gives a detailed overview of the variables under study.
Statistical analyses
Latent Class Analyses (LCA) was used to identify unobserved (latent) groups based on similarity of response patterns in observed (manifest) variables under the assumption of statistical independency (Collins & Lanza, 2009). In preparation for LCA, we transformed metrical or multinomial variable values into binary categories coded at levels 1 and 2 (Linzer & Lewis, 2011). If applicable, we used prescribed cut-off values (e.g., psychopathological symptoms assessed with the PHQ-D) for dichotomizing the metric variable scores. Elsewise, metric variable scores or single item values were dichotomized based on 75% or 25% quantile bands of the distribution. For multinomial variable values we summarized answers based on theoretical and distribution-related appropriateness. For further details see the Measures section and Table S1 in the Supplementary Materials.
In the first set of analyses, we conducted subsequent LCA models by specifying 1 to 7 classes with several random starting values and 200 model estimate repetitions including the 50 indicators and 3 covariates. The analyses were conducted with the software R (R Core Team, 2021) and by using the poLCA (Linzer & Lewis, 2011) and tidyLPA (Rosenberg et al., 2018) packages. In poLCA, the expectation-maximization and Newton-Raphson algorithms are used to estimate the latent class model log-likelihood function. The following information criteria were used in order to assess the statistical model fit and optimal number of classes: Aikake´s Information Criteria (AIC), Bayesian Information Criteria (BIC), adjusted BIC, entropy and power based on Lo-Mendell-Rubin adjusted Likelihood Ratio Test (LMR-LRT) comparing k-1 classes. There were no missing variables due to forced choice response format.
In the second set of analyses, we conducted linear mixed-effects models (LME) with the lmerTest package (Kuznetsova et al., 2017). Thereby, we predicted the course of QoL scores (averaged by month and lockdown period) from the latent classes while taking repeated-measurements nested within persons as random effects into account. Linear mixed-effects modeling is appropriate for handling variation among the number or timing of observations (i.e., unbalanced data; Laird & Ware, 1982). In line with suggestions of higher statistical precision and avoidance of selection bias, we included all participants, even those with only baseline measurement, to estimate the changes (slopes) in the participant population (Thiébaut & Walker, 2008).
Results
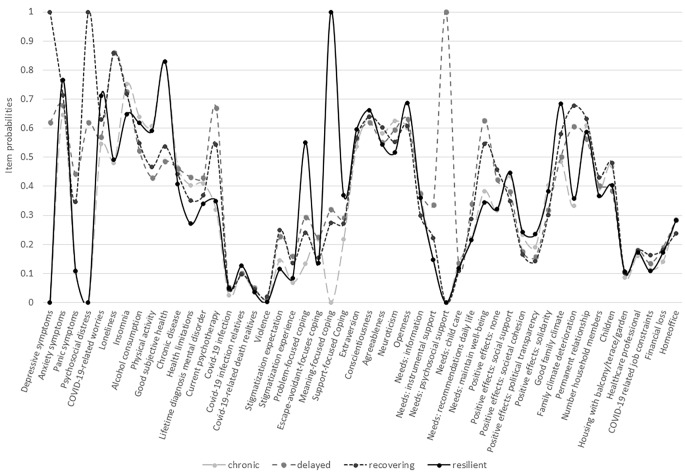
The results from LCA including a variety of 50 risk-enhancing and -reducing factors (see Fig. 1) and with the participant’s age, sex and educational level as covariates, suggested that a four and a five latent class solution fitted best the current data with regards to the information criteria presented in Table 1. On behalf of theory (Bonanno, 2004; Bonanno et al., 2011; Mancini & Bonanno, 2009), interpretability, and comparability to previous findings on latent classes in responses to the current and past pandemics (Bonanno et al., 2011; Mancini et al., 2011; Pierce et al., 2021; Shilton et al., 2021), we considered the four-class solution as optimal and focused in the following analyses on the four classes in more detail.
Fig. 1.
Item probabilities for each of the indicators under study (see the Supplementary Materials Table S2 in detail) grouped by four latent classes resulting from LCA
Table 1.
Summary of Latent Class Analysis Information Criteria (N = 2,137)
| # classes | MLL | AIC | BIC | aBIC | Entropy | LMR-LRT1 |
|---|---|---|---|---|---|---|
| 1 | -173262.52 | 347521.10 | 350343.31 | 116525.09 | -- | -- |
| 2 | -54319.42 | 108846.80 | 109435.84 | 109105.41 | 0.894 | 7661.74 |
| 3 | -53391.99 | 107099.98 | 107994.80 | 107492.81 | 0.931 | 1854.86 |
| 4 | -52849.69 | 106123.39 | 107324.03 | 106650.48 | 0.937 | 1084.60 |
| 5 | -52437.69 | 105407.38 | 106913.84 | 106068.73 | 0.937 | 824.00 |
| 6 | -52122.50 | 104885.01 | 106697.30 | 105680.63 | 0.916 | 630.38 |
| 7 | -51822.60 | 104393.21 | 106511.33 | 105323.09 | 0.920 | 599.80 |
Notes. MLL = Maximum log-likelihood, AIC = Akaike information criterion, BIC = Bayesian information criterion, aBIC = adjusted Bayesian information criterion, LMR-LRT = Lo-Mendell-Rubin adjusted Likelihood Ratio Test. 1 LMR-LRT k(-1) Model comparisons were all significant at p < .001. The four-class solution was identified as optimal and highlighted in boldface
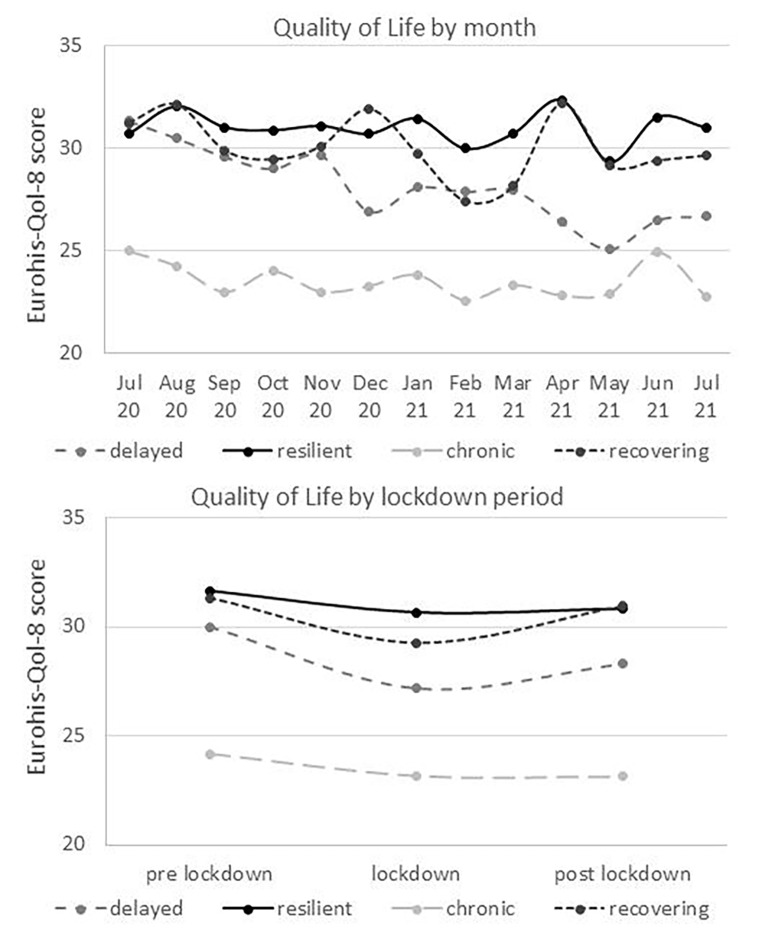
In consideration of the four latent trajectories as depicted in Fig. 2, the classes have been labelled as “resilient” (18.7%), “recovering” (20.6%), “delayed” (25.4%) and “chronic” (35.3%) based on prototypical patterns analogous to previous studies (Bonanno, 2005; Bonanno et al., 2008,2011; Mancini & Bonanno, 2009; Pierce et al., 2021; Shilton et al., 2021). Across time, QoL levels were the highest in the resilient class (M = 32.52, SD = 3.90), followed by the recovering (M = 30.82, SD = 4.41), delayed (M = 25.54, SD = 4.78) and chronic class (M = 23.17, SD = 5.21).
Fig. 2.
Subjective well-being trajectories during the COVID-19 pandemic, grouped by four latent classes as presented in Table 2 and Fig. 1, aggregated by month (above) and lockdown phase (below)
The resilient class is characterized by a low probability of depressive and panic symptoms or distress but moderate levels of anxiety symptoms and COVID-19-related worries. In addition, class members showed a high probability of good physical health and activity, family climate, conscientiousness and openness, meaning- and problem-focused coping, as well as positive experiences such as perceptions of social support and solidarity (see Fig. 1). In contrast, the chronic class is characterized by a high probability of insomnia, alcohol consumption, chronic disease, neuroticism, and a low probability of psychopathological symptoms or COVID-19-related worries, good family climate, meaning- and problem-focused coping. The recovering class is characterized by a high probability of depressive and anxiety symptoms, distress, perceived loneliness, stigmatization expectation, deterioration of family climate, having children, COVID-19-related job constraints and low probability of perceptions of positive effects (see Fig. 1, Table S2 of the Supplementary Materials). Characteristic for the delayed class was a comparatively high probability of panic symptoms, perceived loneliness, current psychotherapy, lifetime diagnosis of any mental disorder, health limitations, urgent need of psychosocial support and recommendations on how to maintain well-being in daily life, as well as a low probability of physical activity, good subjective health, perceiving positive effects and political transparency, in particular. Class membership differed only slightly according to the covariates with a tendency of young age, female sex and high education indicative for the resilient class. Table S2 in the Supplementary Materials presents all class probabilities in detail.
Tables 2 and 3 present the results from four LME models with each of the latent classes as reference category and QoL responses aggregated within-persons on a monthly basis as well as separated by lockdown period. The results suggest a significant main effect of the chronic class with significantly lower QoL as compared to the other classes. In addition, grouping by lockdown period lead to significant QoL differences of the recovering class compared to the resilient, chronic and delayed class (Table 3). While QoL levels remained relatively constant over time for the resilient and chronic class, we found a significant main effect of time (see Tables 2 and 3) as well as interactions with time for the recovering and delayed class, as displayed in Fig. 2. The average QoL level of the recovering class declined from pre-lockdown to lockdown and approximated the baseline level thereafter (post-lockdown); the delayed class showed a steeper decrease of QoL during the lockdown phase followed by a slower increase during the post-lockdown phase.
Table 2.
Predicting Quality of Life by Four Latent Classes (Resilient, Recovering, Delayed, Chronic), Time aggregated in Months and Interactions based on Mixed-Effects Regression Modeling with the Participants as Random Effects Nested within Time (N = 2,137)
| QoL – M1 | QoL – M2 | QoL – M3 | QoL – M4 | |||||
|---|---|---|---|---|---|---|---|---|
| B (SE) | p | B (SE) | p | B (SE) | p | B (SE) | p | |
| Intercept | 31.92 (0.37) | < 0.001 | 31.31 (0.36) | < 0.001 | 32.15 (0.46) | < 0.001 | 24.28 (0.46) | < 0.001 |
| Resilient | Ref | 0.61 (0.52) | 0.236 | -0.23 (0.59) | 0.146 | 7.64 (0.60) | < 0.001 | |
| Recovering | -0.62 (0.52) | 0.236 | Ref | -0.84 (0.58) | 0.695 | 7.03 (0.59) | < 0.001 | |
| Delayed | 0.23 (0.59) | 0.695 | 0.85 (0.58) | 0.146 | Ref | 7.87 (0.65) | < 0.001 | |
| Chronic | -7.64 (0.60) | < 0.001 | -7.03 (0.69) | < 0.001 | -7.88 (0.65) | < 0.001 | Ref | |
| Month | -0.14 (0.08) | 0.067 | -0.47 (0.06) | < 0.001 | -0.29 (0.08) | < 0.001 | -0.10 (0.07) | 0.157 |
| Resilient × Month | Ref | 0.34 (0.10) | < 0.001 | 0.15 (0.11) | 0.189 | -0.03 (0.11) | 0.742 | |
| Recovering × Month | -0.33 (0.10) | < 0.001 | Ref | -0.19 (0.09) | 0.047 | -0.37 (0.10) | < 0.001 | |
| Delayed × Month | -0.15 (0.11) | 0.107 | -0.19 (0.09) | 0.047 | Ref | -0.18 (0.11) | 0.100 | |
| Chronic × Month | 0.03 (0.11) | 0.741 | -0.37 (0.10) | < 0.001 | 0.18 (0.11) | 0.100 | Ref | |
|
Random effect ID:Time Var = 18.00, SD = 4.24 | ||||||||
Notes. QoL = Quality of Life, M = Model, B = Unstandardized beta coefficient, SE = Standard error, Ref = Reference category, Var = Variance, SD = Standard deviation. M1 = Resilient as reference category, M2 = Recovering as reference category, M3 = Delayed as reference category, M4 = Chronic as reference category. Boldface indicates significant results at p < .05
Table 3.
Predicting Quality of Life by Four Latent Classes (Resilient, Recovering, Delayed, Chronic), Time aggregated in Lockdown Phases and Interactions based on Mixed-Effects Regression Modeling with the Participants as Random Effects Nested within Time (N = 2,137)
| QoL – M1 | QoL – M2 | QoL – M3 | QoL – M4 | |||||
|---|---|---|---|---|---|---|---|---|
| B (SE) | p | B (SE) | p | B (SE) | p | B (SE) | p | |
| Intercept | 30.57(0.55) | < 0.001 | 27.18 (0.36) | < 0.001 | 29.24(0.57) | < 0.001 | 23.17 (0.47) | < 0.001 |
| Resilient | Ref | 3.39(0.66) | < 0.001 | 1.33(0.79) | 0.095 | 7.41(0.73) | < 0.001 | |
| Recovering | -3.39(0.65) | < 0.001 | Ref | -2.06(0.68) | 0.002 | 4.01(0.59) | < 0.001 | |
| Delayed | -1.33(0.79) | 0.095 | 2.06(0.67) | 0.002 | Ref | 6.07(0.74) | < 0.001 | |
| Chronic | -7.41(0.72) | < 0.001 | -4.01(0.59) | < 0.001 | -6.07(0.74) | < 0.001 | Ref | |
| Lockdown vs. pre | 1.05(0.62) | 0.089 | 2.79(0.44) | < 0.001 | 2.07(0.84) | 0.002 | 0.97(0.57) | 0.093 |
| Lockdown vs. post | 0.25(0.82) | 0.762 | 1.10(0.55) | 0.048 | 1.70(0.84) | 0.043 | -0.04(0.76) | 0.961 |
| Resilient Lockdown × pre | Ref | -1.73(0.76) | 0.021 | -1.02(0.91) | 0.262 | 0.08(0.84) | 0.926 | |
| Recovering Lockdown × pre | 1.74(0.75) | 0.021 | Ref | 0.71 (0.80) | 0.368 | 1.81(0.73) | 0.012 | |
| Delayed Lockdown × pre | 1.02(0.91) | 0.065 | -0.72(0.80) | 0.368 | Ref | 1.10(0.87) | 0.213 | |
| Chronic Lockdown × pre | -0.08(0.84) | 0.926 | -1.82(0.73) | 0.012 | -1.10(0.88) | 0.213 | Ref | |
| Resilient Lockdown × post | Ref | -0.85(0.99) | 0.392 | -1.45(1.17) | 0.217 | 0.29(1.12) | 0.798 | |
| Recovering Lockdown × post | 0.85(0.99) | 0.392 | Ref | -0.60(1.01) | 0.553 | 1.14(0.94) | 0.229 | |
| Delayed Lockdown × pre | 1.45(1.17) | 0.217 | 0.60(1.01) | 0.553 | Ref | 1.73(1.13) | 0.125 | |
| Chronic Lockdown × post | -0.29(1.12) | 0.798 | -1.14(0.95) | 0.229 | -1.73(1.13) | 0.125 | Ref | |
|
Random effect ID:Time Var = 20.97, SD = 4.58 |
||||||||
Notes. QoL = Quality of Life, M = Model, B = Unstandardized beta coefficient, SE = Standard error, Ref = Reference category, Var = Variance, SD = Standard deviation. M1 = Resilient as reference category, M2 = Recovering as reference category, M3 = Delayed as reference category, M4 = Chronic as reference category. Boldface indicates significant results at p < .05
Discussion
This study aimed to contribute to the understanding of differences and changes of adult QoL over a period of one year during the COVID-19 pandemic in Germany and with regards to substantial risk-enhancing or -reducing factors. Of particular interest was the question as to which factors are predictive of a resilient response pattern (i.e., maintaining relatively high levels of QoL) to derive recommendations for better preparedness and universal prevention measures.
In general, the actual QoL was slightly lower as compared to German adult norm values from 2004: the average across items was 3.61 (SD = 0.74) vs. 4.08 (SD = 0.49) (Schmidt et al., 2005) and the raw score was 28.91 (SD = 5.90) vs. 30.88 (SD = 4.59) (Brähler et al., 2007). However, the extensive period of 17 years between the two measurement points and non-representativeness of the present sample hinder interpretability of comparison and conclusion about mean-level difference related to the COVID-19 pandemic. By taking also other research into account (van de Weijer et al., 2022), the overall results suggest that the COVID-19 pandemic may not manifest in substantial average QoL change or affect adult QoL levels equally. However, there certainly seem to be subgroups vulnerable to QoL deterioration. In fact, we identified four latent classes (resilient, recovering, delayed and chronic) with distinct QoL patterns in accordance with evidence on prototypical responses to stressful life events from previous research (Bonanno et al., 2011; Mancini et al., 2011) as well as from the initial phase of the COVID-19 pandemic (Pierce et al., 2021; Shilton et al., 2021). Two of these classes, namely the resilient and chronic subgroup, showed relatively stable trajectories over a period of one year on a rather high or low QoL level, respectively. In contrast, the other two classes, showed instability of QoL levels over time indicating adjustment processing in response to the situational demands of the COVID-19 pandemic. Whereas the QoL levels decreased at first in both classes, the recovering class returned almost to baseline level over time and the delayed class showed a steeper decrease and slower increase not reaching the initial baseline level. Thus, the delayed class can be seen as particularly vulnerable to QoL deterioration during the COVID-19 pandemic.
In line with previous evidence on COVID-19-related risk factors (Algahtani et al., 2021; El Keshky et al., 2020; Epifanio et al., 2021; Gibson et al., 2021; Koivunen et al., 2022), we found that people with pre-existing health conditions (lifetime diagnosis of mental disorder, chronic illness, functional limitations) or currently undergoing psychotherapeutic treatment, a rather pessimistic view of the situation (no positive experiences, expecting stigmatization), COVID-19-related job constraints or financial loss, living alone or feeling lonely, had the highest probability of QoL limitations and fell either into the recovering, delayed or chronic class. In contrast to previous findings, we could not find any signs of relatedness between class membership with working in healthcare (Papoutsi et al., 2020) or the occurrence of COVID-19 infections among relatives (Beck et al., 2021), which may be due to differences in health-care systems, amount of COVID-19-related hospitalizations, mortality rate or sampling bias (e.g., under-representation or lack of certain job information such as working in intensive or outpatient care) (Skoda et al., 2020).
Additionally, we observed a high probability of symptoms of depression, anxiety and psychosocial distress in the recovering class. Thus, the results reflect a frequently observed trend of temporarily enhanced psychopathological symptoms that seemed to level off at a certain stage of the COVID-19 pandemic (Mauz et al., 2022; Robinson et al., 2022; Vindegaard & Benros, 2020). The recovering class moreover included people most likely to have children, experiencing deterioration of family climate and COVID-19-related job constraints. Thereby, the recovering class can be seen as representative for a large proportion of families struggling with COVID-19-related losses of income, access to resources, daily routines and planned activities, as well as work-from-home arrangements in combination with childcare (Lee et al., 2020; Prime et al., 2020). In contrast, members of the chronic class showed less signs of COVID-19-related symptoms or worries but reported more unhealthy lifestyle behaviors (insomnia, alcohol consumption), high neuroticism and maladaptive coping in addition to chronic illness. While chronic illness can be seen as one of the most comprehensible indicators of reduced QoL irrespective of situational context (Megari, 2013), there is also evidence on interrelatedness between the other indicators. Neuroticism has been related to a relatively stable trend of maladaptive responding to stressors (i.e., high negative affective reactivity), risky health behaviors, higher risk of mental and physical illness, and mortality (Lahey, 2009). Overall, coping strategy and other personal or social resources (personality, family climate) in this research became apparent as central indicators differentiating between groups of people showing diverse QoL trajectories, as proposed by resilience and stress response theories (Lazarus & Folkman, 1984; Mancini & Bonanno, 2009). Most obviously, meaning-focused coping (e.g., positive reframing and acceptance) was predictive of resilient responding, underscoring previous assumptions on its increased importance particularly in uncontrollable stressful situations (Folkman & Moskowitz, 2007) and during the COVID-19 pandemic in particular (Shamblaw et al., 2021). Relatively high perceptions of solidarity and seldom reports of stigmatization expectation or experience due to a COVID-19 infection were among the most positive experiences during the COVID-19 pandemic were. Both applies to the members of the resilient class.
However, the proportion of resilient individuals in the present study was relatively low as compared to other studies during the COVID-19 pandemic (e.g., in the UK (Pierce et al., 2021), USA and Israel (Shilton et al., 2021), Lithuania and Germany (Truskauskaite-Kuneviciene et al., 2021) or Turkey (Yalçın et al., 2022)). One possible explanation is that the other studies focused on mental health outcomes as indicators of resilient responding (Pierce et al., 2021; Shilton et al., 2021; Truskauskaite-Kuneviciene et al., 2021; Yalçın et al., 2022) while the present research investigated QoL, closely related to other well-being or health measures but representing a distinct dimensional construct (Keyes, 2014). The risk of developing a manifest mental illness during the challenges related to the COVID-19 pandemic may be not as high as the risk of deteriorations of subjective well-being. Future research will have to elaborate on that in more detail.
Summarizing the amount of resilient and recovering response patterns leads to the conclusion that the highest proportion but not even half of the people showed a high probability of adjustment to the challenges of the COVID-19 pandemic while about one fourth was at risk of long-lasting QoL deterioration (delayed class). By taking also into consideration that a considerable proportion of participants fell into the chronic class with comparatively low QoL and high psychopathological symptoms at the same time, highlight the need of both mental illness prevention and QoL promotion in line with the conceptualization of mental health as a dual continuum and complete state (i.e., differentiating between absence of illness and presence of negative well-being or functioning, Keyes 2014). The present findings imply that healthy behaviors (e.g., regular physical activity) and adaptive stress reactivity competencies (e.g., emotional stability as opposed to neuroticism, positive reframing as opposed to denial) may be a good starting point for universal prevention and promotion at the population level. Importantly, the burden of the delayed class can be seen as particularly worrisome with respects to the demands related to the COVID-19 pandemic. People in this class reported unmet needs such as psychosocial support and showed the steepest decline over the period of one year even though receiving psychotherapy to a large extent. Accordingly, people in the delayed class seem to require more or other than the already established prevention and protection efforts to enhance (faster) recovery or resilience.
In consideration of moderate anxiety and COVID-19-related worries even in the resilient class suggests that individuals of each of the four classes have to deal with certain risk factors but the resilient class differentiates from the others by showing maintenance of QoL despite comparable level of adversity, as suggested by resilience theory (Rutter, 2006). It is to be assumed that a certain level of anxiety and worry is a normal reaction and concurrently present risk-reducing factors help compensate and maintain QoL despite certain risk-enhancing factors (e.g., COVID-19-related worries and anxiety symptoms). Other findings underscore this assumption by showing how individuals during the COVID-19 pandemic mobilized resources to compensate needs and maintain their QoL (Herrera et al., 2021). However, these post-hoc explanations were not tested and need further investigation on interaction effects.
Limitations
This study has some limitations that should be considered for interpreting the results. First, the data base was a convenience sample not allowing any generalization of findings to the German population. More precisely, the sample was unbalanced with regard to the educational level and age, comprising a greater amount of people with higher education and from young to middle adulthood. Therefore, the educational level and age were consistently included as covariates in the present analyses. Second, the data collection was undertaken by a smartphone app, thereby limiting the sample to participants who had access and were proficient with smartphones. Third, despite the longitudinal design and advantage of tracing QoL levels over time, this research lacks pre-pandemic QoL levels. Thus, conclusions are limited to the pandemic phase and do not allow continuous pre- to post comparisons. Although the data were collected during the COVID-19 pandemic, recall bias cannot be ruled out either. Furthermore, the interfaces for Android users and iOS users never look the same, which can generally create an information bias.
Conclusion
The results highlight the central need of adaptive coping competency, positive social experience such as solidarity as well as low-threshold psychosocial support and prompt easily accessible recommendations on how to maintain well-being during a societal crisis such as the COVID-19 pandemic. Public health measures should be addressed particularly to people showing considerable QoL deterioration without returning to baseline levels (delayed and chronic response pattern) in both a preventive and promotive matter to enhance preparedness and resilience.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Author contributions
CC, RP and HB devised the CORONA HEALTH APP study conception and design. RP was mainly responsible for the data acquisition and preparation procedures. CC developed the present research questions and methodology. BW, CC and KG performed the data analyses. CC wrote a first draft of the manuscript. All authors critically revised the manuscript and approved the final version to be published.
Funding
Open Access funding enabled and organized by Projekt DEAL. HB and RP are supported by grants in the project COMPASS. COMPASS is part of the German COVID-19 Research Network of University Medicine (“Netzwerk Universitätsmedizin”), funded by the German Federal Ministry of Education and Research (funding reference 01KX2021).
Data Availability
The data presented in this study are available on request from the corresponding author. The data are not publicly available because participants’ informed consent did not cover public deposition of data.
Declarations
Ethics approval
The CORONA HEALTH App study was conducted in accordance with the German medical products law and the data protection officer of the University of Würzburg, Germany. The procedures used in this study adhere to the tenets of the Declaration of Helsinki and was approved by the ethics committee of the University of Würzburg, Germany (No. 130/20-me).
Consent to participate
Informed consent was obtained from all participants involved in the study.
Competing interests
The authors declare that there is no conflict of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Algahtani FD, Hassan SN, Alsaif B, Zrieq R. Assessment of the quality of life during COVID-19 pandemic: A cross-sectional survey from the kingdom of saudi arabia. International Journal of Environmental Research and Public Health. 2021;18(3):847. doi: 10.3390/ijerph18030847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bastien CH, Vallières A, Morin CM. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Medicine. 2001;2(4):297–307. doi: 10.1016/S1389-9457(00)00065-4. [DOI] [PubMed] [Google Scholar]
- Beck K, Vincent A, Becker C, Keller A, Cam H, Schaefert R, Hunziker S. Prevalence and factors associated with psychological burden in COVID-19 patients and their relatives: A prospective observational cohort study. PLoS One. 2021;16(5):e0250590. doi: 10.1371/journal.pone.0250590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beierle F, Schobel J, Vogel C, Allgaier J, Mulansky L, Haug F, Pryss R. Corona Health—A study- and sensor-based mobile app platform exploring aspects of the COVID-19 pandemic. International journal of Environmental Research and Public Health. 2021;18(14):7395. doi: 10.3390/ijerph18147395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonanno G. Loss, trauma, and human resilience: Have we underestimated the human capacity to thrive after extremely aversive events? The American Psychologist. 2004;59:20–28. doi: 10.1037/0003-066X.59.1.20. [DOI] [PubMed] [Google Scholar]
- Bonanno GA. Resilience in the face of potential trauma. Current Directions in Psychological Science. 2005;14(3):135–138. doi: 10.1111/j.0963-7214.2005.00347.x. [DOI] [Google Scholar]
- Bonanno GA, Ho SM, Chan JC, Kwong RS, Cheung CK, Wong CP, Wong VC. Psychological resilience and dysfunction among hospitalized survivors of the SARS epidemic in Hong Kong: A latent class approach. Health Psychology. 2008;27(5):659–667. doi: 10.1037/0278-6133.27.5.659. [DOI] [PubMed] [Google Scholar]
- Bonanno GA, Westphal M, Mancini AD. Resilience to loss and potential trauma. Annual Review of Clinical Psychology. 2011;7(1):511–535. doi: 10.1146/annurev-clinpsy-032210-104526. [DOI] [PubMed] [Google Scholar]
- Brähler E, Mühlan H, Albani C, Schmidt S. Teststatistische Prüfung und Normierung der deutschen Versionen des EUROHIS-QOL Lebensqualität-Index und des WHO-5 Wohlbefindens-Index. [Test Statistical Review and Standardization of the German Versions of the EUROHIS-QOL Quality of Life Index and the WHO-5 Well-Being Index] Diagnostica. 2007;53(2):83–96. doi: 10.1026/0012-1924.53.2.83. [DOI] [Google Scholar]
- Bryson WJ. Long-term health-related quality of life concerns related to the COVID-19 pandemic: a call to action. Quality of Life Research. 2021;30(3):643–645. doi: 10.1007/s11136-020-02677-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carver CS. You want to measure coping but your protocol’ too long: Consider the brief cope. International Journal of Behavioral Medicine. 1997;4(1):92. doi: 10.1207/s15327558ijbm0401_6. [DOI] [PubMed] [Google Scholar]
- Cohrdes, C., Pryss, R., Baumeister, H., Eicher, S., Knoll, N., & H?lling, H. (in revision). Seeking support as one key coping strategy for maintaining quality of life during the COVID-19 pandemic
- Collins, L. M., & Lanza, S. T. (2009). Latent class and latent transition analysis: With applications in the social, behavioral, and health sciences (718 vol.). John Wiley & Sons.
- Cox B, Oyen HV, Cambois E, Jagger C, Roy S, Robine JM, Romieu I. The reliability of the Minimum European Health Module. International Journal of Public Health. 2009;54(2):55–60. doi: 10.1007/s00038-009-7104-y. [DOI] [PubMed] [Google Scholar]
- Eid, M. (2018). Statistical approaches to analyzing well-being data. In E. Diener, S. Oishi, & L. Tay (Eds.), Handbook of Well-Being. DEF Publishers. https://doi.org/nobascholar.com
- El Keshky, M. E. S., Basyouni, S. S., & Al Sabban, A. M. (2020). Getting through COVID-19: The pandemic’s impact on the psychology of sustainability, quality of life, and the global economy – A systematic review. Frontiers in Psychology, 11:585897. 10.3389/fpsyg.2020.585897 [DOI] [PMC free article] [PubMed]
- Epifanio, M. S., Andrei, F., Mancini, G., Agostini, F., Piombo, M. A., Spicuzza, V., & La Grutta, S. (2021). The impact of COVID-19 pandemic and lockdown measures on quality of life among Italian general population. Journal of Clinical Medicine, 10(2), 10.3390/jcm10020289 [DOI] [PMC free article] [PubMed]
- Folkman S, Moskowitz J. Coping: Pitfalls and promise. Annual Review of Psychology. 2004;55:745–774. doi: 10.1146/annurev.psych.55.090902.141456. [DOI] [PubMed] [Google Scholar]
- Folkman, S., & Moskowitz, J. T. (2007). Positive affect and meaning-focused coping during significant psychological stress. In M. Hewstone, H. Schut, de J. Wit, Van Den K. Bos, & M. Stroebe (Eds.), The scope of social psychology: Theory and applications (pp. 193–208). Psychology Press. 10.4324/9780203965245
- Gan Y, Fu Q. Risk perception and coping response to COVID-19 mediated by positive and negative emotions: A study on Chinese college students. PLoS One. 2022;17(1):e0262161. doi: 10.1371/journal.pone.0262161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibson B, Schneider J, Talamonti D, Forshaw M. The impact of inequality on mental health outcomes during the COVID-19 pandemic: A systematic review. Canadian Psychology/Psychologie canadienne. 2021;62(1):101–126. doi: 10.1037/cap0000272. [DOI] [Google Scholar]
- Haas BK. A multidisciplinary concept analysis of quality of life. Western Journal of Nursing Research. 1999;21(6):728–742. doi: 10.1177/01939459922044153. [DOI] [PubMed] [Google Scholar]
- Hentschel S, Eid M, Kutscher T. The influence of major life events and personality traits on the stability of affective well-being. Journal of Happiness Studies. 2017;18(3):719–741. doi: 10.1007/s10902-016-9744-y. [DOI] [Google Scholar]
- Herrera MS, Elgueta R, Fernández MB, Giacoman C, Leal D, Marshall P, Bustamante F. A longitudinal study monitoring the quality of life in a national cohort of older adults in Chile before and during the COVID-19 outbreak. BMC Geriatrics. 2021;21(1):143. doi: 10.1186/s12877-021-02110-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keyes, C. L. M. (2014). Mental health as a complete state: How the salutogenic perspective completes the picture. In G. F. Bauer & O. Hämmig (Eds.), Bridging Occupational, Organizational and Public Health: A Transdisciplinary Approach (pp. 179–192). Springer Netherlands. 10.1007/978-94-007-5640-3_11
- Knoll N, Rieckmann N, Schwarzer R. Coping as a mediator between personality and stress outcomes: a longitudinal study with cataract surgery patients. European Journal of Personality. 2005;19(3):229–247. doi: 10.1002/per.546. [DOI] [Google Scholar]
- Koivunen K, Portegijs E, Sillanpää E, Eronen J, Kokko K, Rantanen T. Maintenance of high quality of life as an indicator of resilience during COVID-19 social distancing among community-dwelling older adults in Finland. Quality of Life Research. 2022;31(3):713–722. doi: 10.1007/s11136-021-03002-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuznetsova A, Brockhoff PB. lmerTest Package: Tests in Linear Mixed Effects Models. Journal of Statistical Software. 2017;82(13):1–26. doi: 10.18637/jss.v082.i13. [DOI] [Google Scholar]
- Lahey BB. Public health significance of neuroticism. The American Psychologist. 2009;64(4):241–256. doi: 10.1037/a0015309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laird NM, Ware JH. Random-effects models for longitudinal data. Biometrics. 1982;38(4):963–974. doi: 10.2307/2529876. [DOI] [PubMed] [Google Scholar]
- Lazarus, R. S. (1966). Psychological stress and the coping process. McGraw-Hill.
- Lazarus RS. Coping theory and research: past, present, and future. Psychosomatic Medicine. 1993;55(3):234–247. doi: 10.1097/00006842-199305000-00002. [DOI] [PubMed] [Google Scholar]
- Lazarus, R. S., & Folkman, S. (1984). Stress, appraisal, and coping. Springer.
- Lee J, Chin M, Sung M. How has COVID-19 changed family life and well-being in Korea? Journal of Comparative Family Studies. 2020;51(3/4):301–313. doi: 10.3138/jcfs.51.3-4.006. [DOI] [Google Scholar]
- Linzer DA, Lewis JB. poLCA: An R Package for Polytomous Variable Latent Class Analysis. Journal of Statistical Software. 2011;42(10):1–29. doi: 10.18637/jss.v042.i10. [DOI] [Google Scholar]
- Löwe, B., Spitzer, R. L., Zipfel, S., & Herzog, W. (2002). PHQ-D. Gesundheitsfragebogen für Patienten (PHQ-D). Manual Komplettversion und Kurzform. [PHQ-D. Patient Health Questionnaire (PHQ-D). Manual complete version and short form] (0940–5569).
- Lucas RE. Adaptation and the set-point model of subjective well-being: Does happiness change after major life events? Current Directions in Psychological Science. 2007;16(2):75–79. doi: 10.1111/j.1467-8721.2007.00479.x. [DOI] [Google Scholar]
- Luhmann M, Eid M. Does it really feel the same? Changes in life satisfaction following repeated life events. Journal of Personality and Social Psychology. 2009;97(2):363–381. doi: 10.1037/a0015809. [DOI] [PubMed] [Google Scholar]
- Luhmann M, Hofmann W, Eid M, Lucas RE. Subjective well-being and adaptation to life events: A meta-analysis. Journal of Personality and Social Psychology. 2012;102(3):592–615. doi: 10.1037/a0025948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mancini AD, Bonanno GA. Predictors and parameters of resilience to loss: Toward an individual differences model. Journal Of Personality. 2009;77(6):1805–1832. doi: 10.1111/j.1467-6494.2009.00601.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mancini AD, Bonanno GA, Clark AE. Stepping off the hedonic treadmill: Individual differences in response to major life events. Journal of Individual Differences. 2011;32(3):144–152. doi: 10.1027/1614-0001/a000047. [DOI] [Google Scholar]
- Marroquín B, Vine V, Morgan R. Mental health during the COVID-19 pandemic: Effects of stay-at-home policies, social distancing behavior, and social resources. Psychiatry Research. 2020;293:113419. doi: 10.1016/j.psychres.2020.113419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mauz E, Eicher S, Peitz D, Junker S, Hölling H, Thom J. Mental health of the adult population in Germany during the COVID-19 pandemic. Rapid Review. Journal of Health Monitoring. 2022;6(S7):1–63. doi: 10.25646/953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Megari K. Quality of life in chronic disease patients. Health Psychology Research. 2013;1(3):e27–e27. doi: 10.4081/hpr.2013.e27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Motta Zanin G, Gentile E, Parisi A, Spasiano DA. Preliminary evaluation of the public risk perception related to the COVID-19 health emergency in Italy. International Journal of Environmental Research and Public Health. 2020;17(9):3024. doi: 10.3390/ijerph17093024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogueji IA, Okoloba MM, Demoko Ceccaldi BM. Coping strategies of individuals in the United Kingdom during the COVID-19 pandemic. Current Psychology. 2021;Jan 3:1–7. doi: 10.1007/s12144-020-01318-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Papoutsi E, Giannakoulis VG, Ntella V, Pappa S, Katsaounou P. Global burden of COVID-19 pandemic on healthcare workers. ERJ Open Research. 2020;6(2):00195–02020. doi: 10.1183/23120541.00195-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park KH, Kim AR, Yang MA, Lim SJ, Park JH. Impact of the COVID-19 pandemic on the lifestyle, mental health, and quality of life of adults in South Korea. PLoS One. 2021;16(2):e0247970. doi: 10.1371/journal.pone.0247970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pierce M, McManus S, Hope H, Hotopf M, Ford T, Hatch SL, Abel KM. Mental health responses to the COVID-19 pandemic: a latent class trajectory analysis using longitudinal UK data. The Lancet Psychiatry. 2021;8(7):610–619. doi: 10.1016/S2215-0366(21)00151-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prime H, Wade M, Browne DT. Risk and resilience in family well-being during the COVID-19 pandemic. American Psychologist. 2020;75(5):631–643. doi: 10.1037/amp0000660. [DOI] [PubMed] [Google Scholar]
- Rammstedt B, Kemper CJ, Klein MC, Beierlein C, Kovaleva A. A short scale for assessing the Big Five dimensions of personality: 10 Item Big Five Inventory (BFI-10) Methods Data Analyses. 2017;7(2):233–249. doi: 10.12758/mda.2013.013. [DOI] [Google Scholar]
- Richter, D., & Weinhardt, M. (2013). LS-S: Loneliness Scale-SOEP. In C. J. Kemper, M. Zenger, & E. Brähler (Eds.), Psychologische und sozialwissenschaftliche Kurzskalen: Standardisierte Erhebungsinstrumente für Wissenschaft und Praxis (1.st ed.). Berlin: Mwv Medizinisch Wissenschaftliche Verlagsges.
- Robinson E, Sutin AR, Daly M, Jones A. A systematic review and meta-analysis of longitudinal cohort studies comparing mental health before versus during the COVID-19 pandemic in 2020. Journal of Affective Disorders. 2022;296:567–576. doi: 10.1016/j.jad.2021.09.098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roesch SC, Weiner B. A meta-analytic review of coping with illness: Do causal attributions matter? Journal of Psychosomatic Research. 2001;50(4):205–219. doi: 10.1016/S0022-3999(01)00188-X. [DOI] [PubMed] [Google Scholar]
- Rogers AM, Lauren BN, Baidal W, Ozanne JA, Hur C. Persistent effects of the COVID-19 pandemic on diet, exercise, risk for food insecurity, and quality of life: A longitudinal study among U.S. adults. Appetite. 2021;167:105639. doi: 10.1016/j.appet.2021.105639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenberg JM, Beymer PN, Anderson DJ, Van Lissa CJ. tidyLPA: An R package to easily carry out Latent Profile Analysis (LPA) using open-source or commercial software. Journal of Open Source Software. 2018;3(30):978. doi: 10.21105/joss.00978. [DOI] [Google Scholar]
- Rutter, M. (2006). The promotion of resilience in the face of Aaversity. In Families count: Effects on child and adolescent development. (pp. 26–52). Cambridge University Press. 10.1017/CBO9780511616259.003
- R Core Team R: A language and environment for statistical computing. Journal of Statistical Software. 2021;42:1–29. [Google Scholar]
- Schmidt S, Mühlan H, Power M. The EUROHIS-QOL 8-item index: psychometric results of a cross-cultural field study. European Journal of Public Health. 2005;16(4):420–428. doi: 10.1093/eurpub/cki155. [DOI] [PubMed] [Google Scholar]
- Schulze B, Stuart H, Riedel-Heller SG. The German version of the Inventory of Stigmatizing Experiences (ISE) - a new tool for assessing the prevalence and impact of “felt stigma". Psychiatrische Praxis. 2009;36(8):e19–27. doi: 10.1055/s-0029-1223337. [DOI] [PubMed] [Google Scholar]
- Schwarzer, R., & Schulz, U. (2003). Stressful life events. In I. B. Weiner, A. M. Nezu, C. M. Nezu, & P. A. Geller (Eds.), Handbook of Psychology: Health Psychology (Vol. 9, pp. 27–49). 10.1002/0471264385.wei0902
- Shamblaw AL, Rumas RL, Best MW. Coping during the COVID-19 pandemic: Relations with mental health and quality of life. Canadian Psychology/Psychologie canadienne. 2021;62(1):92–100. doi: 10.1037/cap0000263. [DOI] [Google Scholar]
- Shilton, T., Mancini, A. D., Perlstein, S., Didomenico, G. E., Visoki, E., Greenberg, D. M., & Barzilay, R. (2021). Prospective predictors of risk and resilience trajectories during the early stages of the COVID-19 pandemic: a longitudinal study. medRxiv, 2021.2010.2008.21264752. 10.1101/2021.10.08.21264752 [DOI] [PMC free article] [PubMed]
- Skinner, E. A., & Zimmer-Gembeck, M. J. (2011). Perceived control and the development of coping. The Oxford handbook of stress, health, and coping (pp. 35–59). Oxford University Press.
- Skoda EM, Teufel M, Stang A, Jöckel KH, Junne F, Weismüller B, Bäuerle A. Psychological burden of healthcare professionals in Germany during the acute phase of the COVID-19 pandemic: differences and similarities in the international context. Journal of Public Health. 2020;42(4):688–695. doi: 10.1093/pubmed/fdaa124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer RL, Kroenke K, Williams JBW, Patient Health Questionnaire Primary Care Study Group Validation and Utility of a Self-report Version of PRIME-MDThe PHQ Primary Care Study. Journal Of The American Medical Association. 1999;282(18):1737–1744. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- Thiébaut R, Walker S. When it is better to estimate a slope with only one point. QJM: Monthly Journal of the Association of Physicians. 2008;101(10):821–824. doi: 10.1093/qjmed/hcn099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Truskauskaite-Kuneviciene I, Brailovskaia J, Margraf J, Kazlauskas E. Evidence on resilient initial response to COVID-19 pandemic among youth: Findings from the prospective study of mental health in two European countries. Emerging Adulthood. 2021 doi: 10.1177/21676968211031120. [DOI] [Google Scholar]
- van de Weijer, M. P., Pelt, D. H. M., de Vries, L. P., Huider, F., van der Zee, M. D., Helmer, Q., & Bartels, M. (2022). Genetic and environmental influences on quality of life: The COVID-19 pandemic as a natural experiment. Genes Brain Behavior, e12796. 10.1111/gbb.12796 [DOI] [PMC free article] [PubMed]
- Vindegaard N, Benros ME. COVID-19 pandemic and mental health consequences: Systematic review of the current evidence. Brain Behavior and Immunity. 2020;89:531–542. doi: 10.1016/j.bbi.2020.05.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yalçın İ, Can N, Mançe Çalışır Ö, Yalçın S, Çolak B. Latent profile analysis of COVID-19 fear, depression, anxiety, stress, mindfulness, and resilience. Current Psychology. 2022;41(1):459–469. doi: 10.1007/s12144-021-01667-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available because participants’ informed consent did not cover public deposition of data.