FIGURE 7.
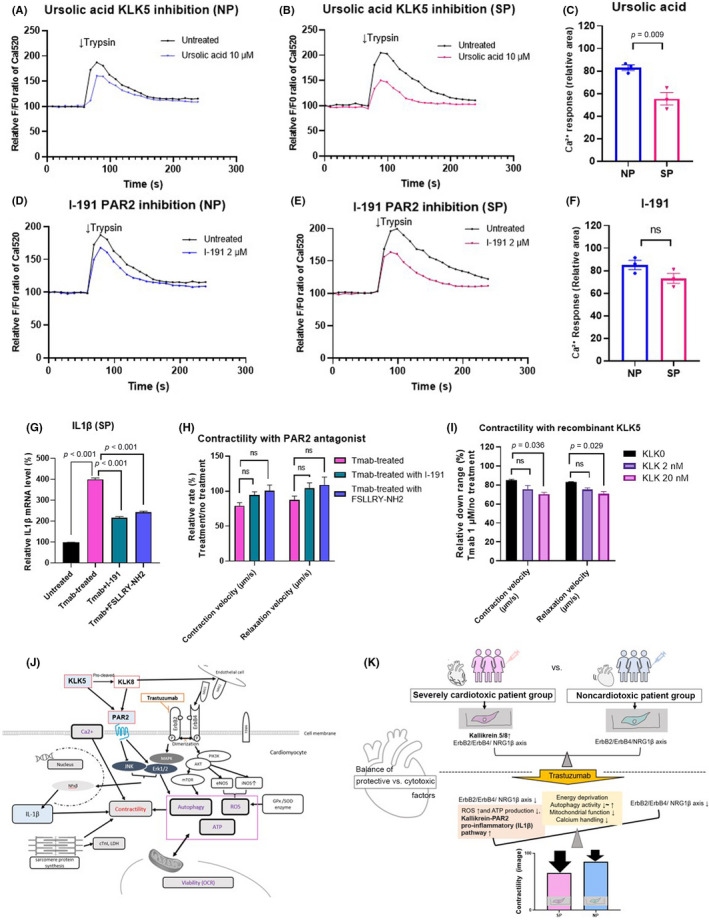
Inhibition of the kallikrein5 (KLK5)–protease‐activated receptor 2 (PAR2) pathway suppresses inflammation and recombinant KLK5‐mediated contractility toxicity in patient‐specific induced pluripotent stem cell‐derived cardiomyocytes (pt‐iPSC‐CM). (A–F) Trypsin (100 nM) induced Ca2+ release in pt‐iPSC‐CMs. (A, B) Representative Ca2+ signaling change with or without the KLK5 antagonist, ursolic acid (UA). (D, E) Representative Ca2+ signaling change with or without the PAR2 antagonist, I‐191. (C, F) Comparison of the relative area of change in Ca2+ response to trypsin under UA and I‐191 treatment. The curved graph area above the F0 baseline was measured using ImageJ. (G) Interleukin‐1β (IL1β) mRNA expression in the severely cardiotoxic patient group (SP) treated with trastuzumab (Tmab) for 7 days ± I‐191 and FSLLRY‐NH2. (H) Contractility in SP treated with Tmab for 7 days ± I‐191 and FSLLRY‐NH2. (I) Contraction and relaxation velocities in noncardiotoxic patient group (NP) treated with Tmab ± recombinant KLK5 (2 nM, 20 nM). (J) Proposed relationship between KLK5/KLK8‐PAR2‐MAPK and ErbB signaling pathways in the pt‐iPSC‐CM model. (K) Schematic showing the multifactorial molecular differences in contractility in SP and NP pt‐iPSC‐CMs and alterations in the balance between protective and cytotoxic effects after Tmab administration. All data are expressed as mean ± SEM. eNOS, endothelial nitric oxide synthase; iNOS, inducible nitric oxide synthase; ns, not significant; OCR, oxygen consumption rate; ROS, reactive oxygen species
