Figure. Maternal SARS-CoV-2 infection may drive maternal and fetoplacental immune activation, with subsequent potential for adverse offspring health outcomes.
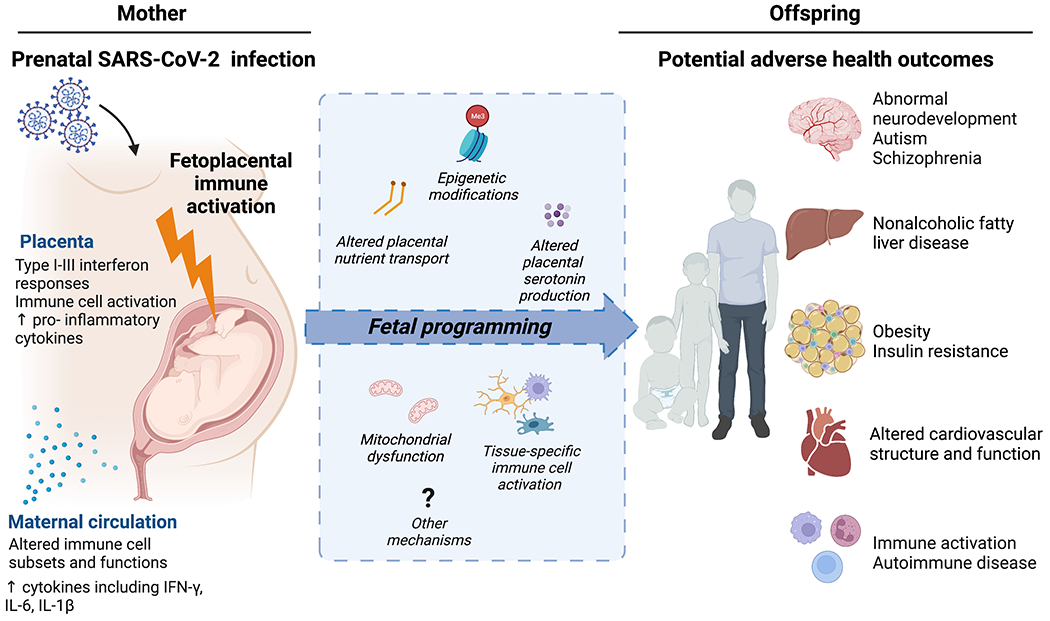
Recent studies demonstrate maternal and fetoplacental immune activation in response to maternal SARS-CoV-2 infection. Selected impacts of SARS-CoV-2 infection on maternal and placental immune activation are detailed on the left panel. Mechanisms implicated in fetal brain and organ programming in response to infectious and non-infectious immune-activating prenatal exposures – which may parallel maternal immune activation in SARS-CoV-2 - are illustrated in the central blue box and include alterations in: placental nutrient (including fatty acid) transport, epigenetic modifications in fetal organs (e.g. brain, liver, white adipose tissue, skeletal muscle), placental serotonin/neurotransmitter production, tissue mitochondrial dysfunction, and tissue-specific macrophage reactivity (e.g., fetal brain microglia, placental macrophages, cardiac and liver macrophages, blood). Although longer-term outcomes of infants and young children born to pregnant individuals with COVID-19 infection have not yet been described, some early reports suggest immune dysregulation and increased neurodevelopmental risk. Maternal-fetoplacental immune activation in other non-SARS-CoV-2 contexts (e.g. obesity, other viral infections) has been linked to multiple other adverse health outcomes in offspring such as those depicted in the right panel. Figure created with BioRender.
