FIGURE 1.
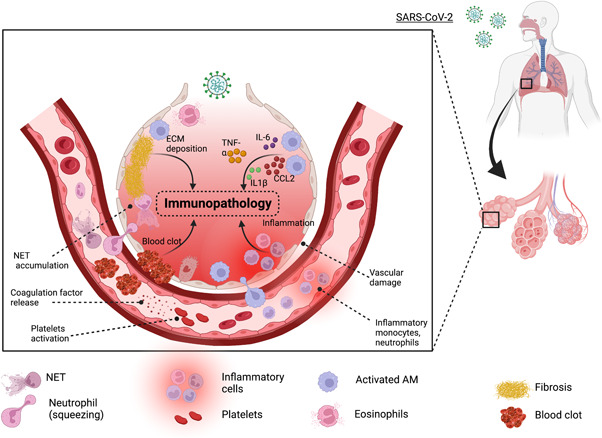
Innate cell‐mediated immunopathology in COVID‐19: Upon viral entry, there is a cascade of events that leads to inflammation, vascular damage, and blot. Tissue‐resident alveolar macrophages (AMs) and interstitial macrophages are among the first responders to SARS‐CoV‐2, which secret inflammatory cytokines including TNF, IL‐6, IL‐1β, and CCL2 that in addition to building up local inflammation but also attract monocyte and neutrophils to the site of infection. Furthermore, IL‐1β favors the expansion of pathological fibroblasts that further contribute to fibrosis. SARS‐CoV‐2 can also stimulate platelets and neutrophils to secrete coagulation factors resulting in the formation of leukocyte–platelet aggregates and NETs, respectively. Lastly, fibroblast proliferation leads to the deposition of extracellular matrix (ECM) and fibrin in alveolar space further complicating the lung alveolar structure. COVID‐19, coronavirus disease 2019; IL‐6, interleukin 6; NET, neutrophil extracellular trap; SARS‐CoV‐2, severe acute respiratory syndrome coronavirus 2; TNF, tumor necrosis factor.
