To the Editor,
There is a growing evidence of increased antiviral humoral immune responses and inflammatory immune signatures in adult patients with autoantibodies during COVID‐19, as well as transient autoantibody production. 1 These findings confirm previous studies, and, as also mentioned by the authors, highlight the possibility that a “misdirected immune response” may play a role in the development of post‐COVID conditions, also commonly known as long COVID.
However, available research is mostly focusing on adults, while in my opinion, there is an unfruitful discussion to raise a discussion on pediatric post covid conditions (PCCs). It is important to highlight that PCCs can also affect children and we are in urgent need of a better understanding of this entity in this group. Although it is plausible to speculate that an immune dysregulation can be involved in pediatric PCCs as well, this aspect has never been investigated so far. Unfortunately, current studies mostly focused on weak surveys investigating how many children were complaining persisting symptoms after COVID‐19. 2 This approach has led to an unfruitful discussion focusing on whether PCCs are a real entity in children, or a psychological consequence of social restrictions. 3 In turn, such an approach risks hindering funds availability for the management and in‐depth biomolecular studies for the characterization of pediatric PCCs. As a consequence, families are struggling to find answers to their children's illnesses. 4
As a pediatrician involved in the follow‐up of children with SARS‐CoV‐2 infection, I have so far clinically assessed >500 children and managed children with chronic relapsing pericarditis, new‐onset diabetes, rise in autoantibodies in children with previously well‐controlled celiac disease, and a larger number of children with chronic fatigue, musculoskeletal pains, headache, rashes without an alternative known etiology. However, here I want to focus on a recent adolescent I assessed in March 2022, which may well fit with the findings of Taeschler and colleagues. 1
A. is a 16‐years‐old previously healthy girl, having mild COVID‐19 on December 14, 2021 (prevalent Delta wave in Italy), and March 5, 2022 (Omicron wave in Italy) (unvaccinated). On March 16 started complaining of progressively worsening chest pain, dyspnea, and high‐grade fever. On admission, she presented anemia and elevated C‐reactive protein but normal procalcitonine. Chest X‐ray showed diffuse bilateral alveolar infiltrates, confirmed on chest computed tomography (Figure 1). She was started on azithromycin and ceftriaxone with no benefits. Heart ultrasound showed mild pericardial effusion with normal myocardial function, normal ECG, and troponin. Due to lack of improvement, she underwent a bronchoalveolar lavage which documented alveolar hemorrhage, while extended microbiological studies were negative. Autoimmunity studies were positive for perinuclear antineutrophil cytoplasmic antibodies (pANCA). The girl was diagnosed with pANCA+ diffuse alveolar hemorrhage and treated with high‐dose steroids, plasmapheresis and rituximab with rapidly improving clinical conditions. 5
Figure 1.
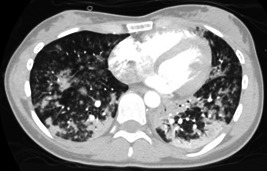
Chest computed tomography scan showing multiple bilateral bronchopulmonary infiltrates
Although the detailed description of this case is out of the purpose of this commentary, and a proven link with SARS‐CoV‐2 is not demonstrated, it cannot be excluded as well, particularly in light of Taeschler's study, 1 and three similar previous reports of post‐COVID p‐ANCA vasculitis. 6 , 7 , 8 All together, these observations drive me to ask the whole scientific community to recognize that post‐viral illness (and, therefore, PCCs), although less frequently than in adults, can impact on children as well. Only if the whole scientific community and major international journals recognize this problem, researchers involved in pediatric PCCs and families will have the possibility to access the needed resources for research, diagnostics, and treatments. Ultimately, this will help all the hidden and neglected children and young people that have suffered or are still suffering from uncharacterized postinfectious chronic diseases. 9
AUTHOR CONTRIBUTION
Danilo Buonsenso: Conceptualization; investigation; writing—original draft; validation; writing—review and editing.
CONFLICTS OF INTEREST
I have participated to peer‐to‐peer educational programs supported by Pfizer on the impact of COVID‐19 in children. I have received a Pfizer grant for the definition of long‐term outcomes of COVID‐19.
ACKNOWLEDGMENTS
The management of this case required the multidisciplinary involvement of several child health experts from different areas of expertise in our Institution. The detailed description and management of this case is, however, out of the purpose of this paper, aimed at raising a call for a better understanding of PCCs in children.
DATA AVAILABILITY STATEMENT
Not applicable.
REFERENCES
- 1. Taeschler P, Cervia C, Zurbuchen Y, et al. Autoantibodies in COVID‐19 correlate with antiviral humoral responses and distinct immune signatures. Allergy. 2022;77(8):2415‐2430. 10.1111/all.15302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Toh ZQ, Anderson J, Mazarakis N, et al. Comparison of seroconversion in children and adults with mild COVID‐19. JAMA Netw Open. 2022;5(3):e221313. 10.1001/jamanetworkopen.2022.1313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Molteni E, Absoud M, Duncan EL. Assessing the impact of the pandemic in children and adolescents: SARS‐CoV‐2 infection and beyond. Lancet Child Adolesc Health. 2022;6(4):216‐217. 10.1016/S2352-4642(22)00035-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Mcfarland S, Citrenbaum S, Sherwood O, van der Togt V, Rossman JS. Long COVID in children. Lancet Child Adolesc Health. 2022;6(1):e1. 10.1016/S2352-4642(21)00338-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Park MS. Diffuse alveolar hemorrhage. Tuberc Respir Dis (Seoul). 2013;74(4):151‐162. 10.4046/trd.2013.74.4.151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Fireizen Y, Shahriary C, Imperial ME, Randhawa I, Nianiaris N, Ovunc B. Pediatric P‐ANCA vasculitis following COVID‐19. Pediatr Pulmonol. 2021;56(10):3422‐3424. 10.1002/ppul.25612 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Hussein A, Al Khalil K, Bawazir YM. Anti‐neutrophilic cytoplasmic antibody (ANCA) vasculitis presented as pulmonary hemorrhage in a positive COVID‐19 patient: a case report. Cureus. 2020;12(8):e9643. 10.7759/cureus.9643 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Powell WT, Campbell JA, Ross F, Peña Jiménez P, Rudzinski ER, Dickerson JA. Acute ANCA vasculitis and asymptomatic COVID‐19. Pediatrics. 2021;147:e2020033092. 10.1542/peds.2020-033092 [DOI] [PubMed] [Google Scholar]
- 9. Buonsenso D, Di Gennaro L, De Rose C, et al. Long‐term outcomes of pediatric infections: from traditional infectious diseases to long covid. Future Microbiol. 2022;17:551‐571. 10.2217/fmb-2022-0031 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.


