Abstract
Background
Persons with dementia spend most time of their day not engaging in activities or social interactions. A care concept of a dementia special care unit that promotes activities and social interaction through a household‐like design and individualised stimuli is studied.
Aim
To evaluate the main outcomes of the care concept of a dementia special care unit, namely, engagement in activities and social interactions.
Methods
We conducted an observational study as part of a theory‐driven evaluation. The Maastricht Daily Life Observation Tool was used to collect momentary assessments multiple times per participant, including engagement in activity, type of activity, engagement in social interaction, interaction partners, location, agitation and mood. Thirty‐three residents of the dementia special care units that implemented the care concept and 54 residents with dementia of two traditional nursing homes participated in the study, resulting in 2989 momentary assessments.
Results
Residents of both settings did not engage in activities or social interaction in approximately half of the observations. Compared to residents of traditional nursing homes, residents of special care units had a significantly higher chance for engagement in activities and social interaction in the afternoon but not in the morning or evening.
Conclusion
The care concept of the special care unit facilitated engagement but had its limitations. Further research is needed to develop and evaluate appropriate interventions to enhance engagement of persons with dementia.
Keywords: activities, dementia, nursing homes, programme evaluation, social interaction, special care unit
BACKGROUND
With the progress of dementia, persons with dementia gradually lose their social and communication skills, it becomes difficult for them to make themselves understood and enjoy conversations or activities in groups [1]. Persons with dementia seem to spend a substantial part of their day by not engaging in activities and with no social interaction, especially in institutional long‐term care. Den Ouden et al. [2] found that nursing home residents were mainly sleeping, doing nothing, watching TV and undertaking activities of daily living, which included mobility, eating and drinking. Engagement in instrumental activities of daily living was rarely observed (up to 3%). Only a few were engaged in self‐directed activities, such as walking or chatting with other residents [3]. Similar results are reported in a variety of studies using different assessment methods [4, 5]. In addition, social interactions between residents or between residents and care staff were seldom observed [6], impinging privacy, loneliness, boredom, autonomy, self‐identity, depression and anxiety [7, 8]. Activities and social interactions are amongst the most prevalent unmet needs of persons with dementia which have a negative impact on their physical, cognitive and psychosocial well‐being [9, 10]. However, engagement in those very needs is associated with positive mood and less boredom and loneliness [11, 12].
Probable reasons for low activity and interaction levels can be found in impaired physical and cognitive functioning [13, 14]. Further persisting problems are hindering spatial layouts and limited time resources of staff members in spite of an often person‐centred approach in care [3, 7, 15]. Other reasons for low activity and interaction levels can be found in residents’ endeavour to ‘fit in’ and act according to a shared definition for specific situations [16]. For example, in communal areas, they try to meet the shared expectations to sit calmly and mind one's own business [17]. However, residents express a desire to engage in activities and relations [15], in particular, participation in individualised activities that matter to them and in enjoyable group activities are regarded as meaningful and dignifying [18]. Therefore, care approaches for persons with dementia are required that include individualised activities and an environment that fosters social interaction. Due to the impact of dementia on a person's skills and views, the provisioning of such interventions on the one hand can be challenging for care providers, on the other it is required to enhance the quality of life of persons with dementia [19].
An approach to enhance quality of care and quality of life is the establishment of dementia special care units (SCU) [20]. They are characterised by their structural design, specifically trained staff and activities adopted to residents’ needs. As there is no shared precises definition of a dementia SCU, they differ in their spatial, structural and care features [21]. Thus, good quality of care in dementia SCUs remains subject to interpretation and demands further research [22].
The current study focuses on SCUs with a specific care concept that aims to provide engagement in purposeful activities and social interactions and is developed specifically for persons with moderate dementia showing challenging behaviours. The main features of the care concept are:
educational interventions (trainings, coaching and supervision sessions) for all staff members on a regular basis
a person‐centred and emotion‐orientated approach in care using Naomi Feil's Validation [23]
small‐scale, homelike wards including a kitchen and living area, adjoining resident rooms and direct garden access
personalised non‐pharmacological interventions offered throughout the whole day to residents including relaxing or activating interventions at group or individual level (such as knitting, cooking, gardening and reading)
Relaxing, personalised interventions and emotion‐orientated care aim to reduce challenging behaviour by making residents feel understood and by addressing their needs. Activating, personalised interventions (such as personalised conversations, provision of favourite leisure activities, provision of personally meaningful items) aim to promote social participation and relations, engagement in purposeful activities and feeling well in a place. The overall concept may have an impact on the affective well‐being, displayed in residents’ emotions [24].
The concept of the SCU, its interventions and mechanisms of impact are assessed and evaluated by using theory‐driven evaluation. As part of the overall project, this article reports on the outcome evaluation of primary outcomes of the care concept. Theory‐driven evaluation is based on a theoretical understanding of the intervention or programme, articulated in a so‐called programme theory, which guides the design of the subsequent outcome and process evaluation. Programme theories include assumptions about the components, processes and desired, as well as undesired changes to be achieved by the specific programme. The programme theory consists of an action and change model. The action model describes the components of the interventions as outlined above. The change model describes the mechanisms through which the interventions achieve the outcomes in detail [25]. For example, the small‐scale household‐like design of the special care units promotes an adequate level of visual, auditory and social stimuli, facilitate orientation and a pleasant atmosphere, and therefore, is believed to reduce residents’ situational stress. As a result, residents tend to spend more time in communal areas, where being part of a social community, engagement in social interactions and purposeful activities is more likely to be promoted. The initial programme theory of the care concept, detailed hypotheses about relationships of interventions, outcomes and impacts, guided the development of the evaluation, including methodology, data collection instruments and methods, as well as analysis of the outcome and process evaluation. The outcome evaluation investigates the outcomes proposed in the programme theory and includes a proxy survey of residents’ outcomes, a study with direct resident observations and a survey of nursing staff members’ outcomes. This article reports as part of the whole project the observational study that evaluated the main outcomes of the care concept of the SCU which are engagement in activities and social interaction of persons with dementia, in comparison with traditional nursing homes (TNH).
METHODS
The theory‐driven evaluation of this study follows the approach of van Belle et al. [26]. This approach includes the following six steps: First, the scope of the evaluation and the appropriateness of theory‐driven evaluation is assessed. In the second step, the initial programme theory, is critically reconstructed, followed by step 3 – choice of data collection methods and development tools. Subsequently, the initial action model (step 4) and the initial change model (step 5) are assessed in comparison with the evaluation results. In Step 6, all findings are translated into the refined programme theory. For the programme being explored in the current study, the steps 1–3 have already been undertaken [24] and the article reports on a comparative cross‐sectional study with direct resident observations as part of the outcome evaluation. The main outcomes of this care concept yielded by the programme theory are engagement in activities and social interactions. These two outcomes are investigated in the present study in persons with dementia living in SCUs and persons with dementia living in TNHs.
Setting
The study was conducted in three nursing homes located in rural regions of Austria. One group, subsequently referred to as SCU, consisted of residents of two dementia SCUs in one nursing home with the same care concept which is described in the background. Each SCU consists of three wards for ten residents connected via a common space and staffed with one Registered Nurse and three nursing aides during the daytime. The entire nursing staff is trained as certified Level I or II Validation Workers (Level I: five two‐day theoretical courses and four practice phases within nine to eleven months; Level II: another three two‐day theoretical courses and two practice phases within seven to nine months), and all other staff members, including managers and cleaning staff, completed a three‐day basic course in Validation. Personalised non‐pharmacological interventions are offered by all nursing staff members and especially by one nurse who is assigned to offer activities to residents.
The comparison group consists of residents with dementia in TNHs. TNHs represent the comparison group because in the regions included in the study, persons with dementia in long‐term care either reside in SCUs or in traditional, non‐specialised nursing homes. The two selected TNHs included in the study represent typical TNHs in the area. They are also home to enough residents in order to provide a large enough sample size of people with dementia for the study. These nursing homes do not have a specific concept of dementia care. However, it was assumed that some nursing staff members would occasionally and proactively apply dementia‐specific care components to individual residents. To account for these probable but unsystematic differences in direct care interactions, two different TNHs were included in the study. In both nursing homes, 128 residents with and without dementia live together on three wards, of which about 70 have a dementia diagnosis. Both nursing homes consist of three wards, with each being laid out for about 45 people and staffed with two Registered Nurses and three to four nursing aides during the daytime. Large common spaces form the centre of the wards, with a dining area, some resting furniture and the nurses’ station. Long corridors lead to the rooms of the residents. They offer a programme with one to two group activities per day.
Participants
SCU and TNH residents were eligible for participation if they (a) had been living there for six months or longer and (b) had a dementia diagnosis according to their medical record or scored less than 24 points in the Mini Mental State Examination [MMSE, ranging from 0 to 30 points, 30 points indicate no cognitive impairment] [27]. MMSE scores in the medical records had to be not older than five months. If residents were eligible for participation, they and their legal representative were informed about the study and were asked for their consent to participate by a research assistant. The sample of the SCU was limited to the residents living in the study‐SCUs. The sample size of TNH is designed to be double in size in order to compensate potential unsystematic differences in direct care interventions that might be observed at TNHs. However, the TNH sample size was only met in approximation due to the actual participation rate.
Outcome variables and measures
Outcomes were derived from the underpinning programme theory and represent the main outcomes of the SCU: engagement in (I) purposeful activities and (II) social interactions. Engagement is defined as ‘being occupied or involved with an external stimulus’ [9]. An activity is considered purposeful if it aims to achieve something, is set intentionally, and is distinguished from activities that do not seem to have a purpose apparent to the observers. The German version of the Maastricht Electronic Daily Live Observation tool (MEDLO‐tool) was used to investigate engagement in both activities and social interactions [28, 29]. With this tool, the activities performed by the resident were assessed in 32 categories (e.g. eating/drinking, playing a game, walking), as well as social interactions in five categories (no social interaction, one‐way interaction from the resident's perspective, one‐way interaction from someone else, two‐way interaction, interactions with more than one person). In addition, both outcome variables were dichotomised (0 = no engagement in activities/social interactions, 1 = engagement in activities/social interactions). Further variables assessed with the MEDLO‐tool were the level of physical activity, the location, the type of social interaction, the interaction partners and agitation, measured with the Pittsburgh Agitation Scale ranging from 0 (no agitation) to 16 (highest level of agitation). Mood was also an item of the MEDLO‐tool, but since it led to considerable interrater discrepancies between the two ratters in the training sessions of the current study (distinction between small and considerable signs of positive or negative mood), the Observed Emotion Rating Scale (OERS) was used instead [30]. The OERS ranges from 0 to 10, with higher scores indicating higher levels of positive emotions. After training the interrater‐reliability of the OERS showed Cohen's Kappa values between 0.63 and 0.86 [31]. The other items of the MEDLO‐tool are regarded as valid and feasible, with Cohen's Kappa values for interrater‐reliability ranging between 0.5 and 1 [28].
Sociodemographic and other personal data, including gender, age and MMSE score, were extracted from residents’ records.
Procedures
The observations were conducted over 30 days between October 2018 and March 2019 by two researchers who were trained to use the tool by the principal investigator of the German version of the MEDLO‐tool. They conducted several training observations to get comfortable with handling the tool, detect and solve any pitfalls in the procedure and increase interrater accordance. Observations took place on all wards of the SCU and TNH in the morning (07:00–11.59), afternoon (12:00–16:59) and evening (17:00–20:00). Every resident was supposed to be observed one morning, one afternoon and one evening on three different days. During these sessions, momentary assessments were made with the tool every twenty minutes for the included residents. Each resident was observed for one minute, after which the researcher scored the items of the MEDLO‐tool. Each researcher observed a maximum of eight residents during one session. The selection of the eight residents amongst all participating residents was made by the researcher in consultation with the ward manager and was based on practicability issues, such as planned absence during the session (e.g. hospital visits for check‐ups). The sequence of the residents within the twenty‐minute slots was defined by a random number generator. Data were entered into a password‐protected electronic database.
Data analysis
First, differences between SCU and TNH on socio‐demographic characteristics were assessed with Chi‐square‐tests for nominal data and t‐test for independent samples for metric data. Second, percentages were calculated for purposeful activity, interaction partners and locations. The aggregated observational data of one individual per session was used to compute means, standard deviations and Cohen's d for the two dichotomous variables engagement in purposeful activities and social interaction (0 = no engagement, 1 = engagement) as well as the two metric measures the Pittsburgh Agitation Scale and the OERS. Third, to test differences between SCU and TNH in the primary outcomes activity and social interaction, a generalised linear mixed model (GLMM) was applied. A random effect for individuals was used to model the correlation between the observations of one person. The following fixed effects were entered in the model: the group (SCU, TNH), the session and their interaction. MMSE score, gender and age were considered as possible further fixed effects, but for each primary outcome, only those variables were added to the model, which were statistically significant. For the analysis of the primary endpoints, data from all residents were used. Fourth, we performed a sensitivity analysis where the participants in SCU and TNH were matched by sex and MMSE scores to account for differences between the two groups in these variables. After matching, GLMMs for the primary outcomes were calculated with the same fixed factors as in the main analyses. Missing values and dropouts were not replaced. We considered a significance level α = 0.05, and due to the exploratory nature of this study, we did not perform any correction for multiple testing.
Ethics
The ethics board of the German Society of Nursing Research approved the study [N° 16‐024]. To ensure all participants were able to decide on the highest possible level of information and understanding, they received information about the study adapted to their abilities. Informed consent was obtained from all participants with the capacity to consent, tested with the German version of the University of California, San Diego Brief Assessment of Capacity to Consent [32]. If residents with dementia were not able to give consent because of their cognitive impairment, they were asked for their assent and, if designated, their legal representative was asked for their informed consent. Consent and assent have been revisited and re‐established at each observation session to account for changes in participants’ opinion and consent and to enhance self‐determination.
RESULTS
Sample characteristics
Data from 33 persons with dementia in SCU and 54 persons with dementia in TNH were collected. Participation rate of eligible residents was 52% in SCU and 35% in TNH, respectively. Reasons for non‐participation were mainly no interest in study subject, no time due to other appointments and no person available to sign the informed consent. As not all participants were present throughout the length of all sessions, the number of momentary assessments per resident varied, resulting in 1227 assessments in SCU and 1762 in TNH (see Table 1). No significant differences in age, gender and MMSE scores were identified between the samples. Since the sample is small, differences are not significant, but show remarkable differences. The smaller range of MMSE scores in the SCU is a result of moderate dementia being an admission criterium for the SCU, excluding persons with mild or severe dementia. Hence, the samples were matched for gender and MMSE scores on an individual level in a sensitivity analysis.
TABLE 1.
Sample characteristics
| SCU | TNH | p‐value | |
|---|---|---|---|
| Number of observed residents, n (%) | 33 (37.9) | 54 (62.1) | – |
| Number of momentary assessments, n (%) | 1227 (41.1) | 1762 (58.9) | – |
| Average number of momentary assessments per resident, n | 37.18 | 32.63 | – |
| Gender, % women | 81.8 | 66.7 | 0.125† |
| Age, mean (SD) | 82.55 (7.27) | 83.91 (8.33) | 0.440‡ |
| MMSE, mean (SD) | 14.01 (2.98) | 14.52 (6.16) | 0.660‡ |
Abbreviations: SCU, special care unit; TNH, traditional nursing home; SD, standard deviation.
Chi‐square test.
t‐test for independent samples.
Engagement in activities
The participants in both settings spent approximately a quarter of the observed time sleeping and resting and another quarter with passive or purposeless activities (e.g. sitting, wandering, repetitive behaviour – see Table 2). Consequently, they engaged in purposeful activities (e.g. reading, eating, chatting, watching TV) in approximately half of all momentary assessments (49% in SCU, 43% in TNH). Figure 1 and Table 3 show the engagement in purposeful activities in the three sessions morning, afternoon and evening. In the morning, no differences between SCU and TNH in engagement in purposeful activities could be seen (SCU: mean = 0.51; SD = 0.21; TNH: mean = 0.49; SD = 0.21). In the afternoon, engagement in purposeful activities was higher in SCU than in TNH (SCU: mean = 0.63; SD = 0.27; TNH: mean = 0.48; SD = 0.28). In the evening, activity levels were lower than in the morning and afternoon in both groups, though engagement in purposeful activities was higher in TNH than in SCU (SCU: mean = 0.26; SD = 0.28; TNH: mean = 0.36; SD = 0.32).
TABLE 2.
Frequencies of activities in the morning, afternoon, and evening
|
SCU n of momentary assessments (%) |
TNH n of momentary assessments (%) |
|
|---|---|---|
| Morning (n = 490/628 momentary assessments) | ||
| (self) care activities a , m | 43 (8.8) | 57 (9.1) |
| Social, communicative activities b , m | 9 (1.8) | 12 (1.9) |
| Eating and drining c , m | 88 (18) | 122 (19.4) |
| Activities outside d , m | 0 (0.0) | 5 (0.8) |
| Household activities e , m | 2 (0.4) | 7 (1.1) |
| Recreational activities f , m | 94 (19.2) | 84 (13.4) |
| Walking g , m | 9 (1.8) | 19 (3.0) |
| Other activities h , m | 3 (0.6) | 4 (0.6) |
| Passive activities i , n | 53 (10.8) | 122 (19.4) |
| Meaningless (repetitive) behaviour j , n | 14 (2.9) | 2 (0.3) |
| Resting k , n | 9 (1.8) | 0 (0.0) |
| Slepping l , n | 166 (33.9) | 194 (30.9) |
| Afternoon (n = 407/589 momentary assessments) | ||
| (self) care activities a , m | 16 (3.9) | 24 (4.1) |
| Social, communicative activities b , m | 15 (3.7) | 16 (2.7) |
| Eating and drining c , m | 93 (22.9) | 71 (12.1) |
| Activities outside d , m | 0 (0.0) | 3 (0.5) |
| Household activities e , m | 13 (3.2) | 2 (0.3) |
| Recreational activities f , m | 80 (19.7)1 | 130 (22.1) |
| Walking g , m | 41 (10.1) | 13 (2.2) |
| Other activities h , m | 2 (0.5) | 14 (2.4) |
| Passive activities i , n | 48 (11.8) | 158 (26.8) |
| Meaningless (repetitive) behaviour j , n | 22 (5.4) | 16 (2.7) |
| Resting k , n | 7 (1.7) | 6 (1.0) |
| Slepping l , n | 70 (17.2) | 136 (23.1) |
| Evening (n = 306/492 momentary assessments) | ||
| (self) care activities a , m | 13 (4.2) | 24 (4.9) |
| Social, communicative activities b , m | 13 (4.2) | 3 (0.6) |
| Eating and drining c , m | 3 (1.0) | 19 (3.9) |
| Activities outside d , m | 0 (0.0) | 1 (0.2) |
| Household activities e , m | 2 (0.7) | 1 (0.2) |
| Recreational activities f , m | 30 (9.8) | 96 (19.5) |
| Walking g , m | 10 (3.3) | 16 (3.3) |
| Other activities h , m | 10 (3.3) | 6 (1.2) |
| Passive activities i , n | 7 (2.3) | 82 (16.7) |
| Meaningless (repetitive) behaviour j , n | 17 (5.6) | 1 (0.2) |
| Resting k , n | 10 (3.3) | 2 (0.4) |
| Slepping l , n | 191 (62.4) | 241 (49.0) |
Abbreviations: SCU, special care unit; TNH, traditional nursing home.
(self) care activities: washing, doing your hair, going to the toilet, brushing teeth, or receiving care from a nurse or aid such as getting medication, etc., visitation bei medical services, beauty activity (mainicure, hairdresser, …).
Social, communicative activities: having a chat, having a phone call, talking groups, helping others.
Eating and drinking: consuming food or drinks.
Activities outside: farm activities, gardening, excursion or shopping, taking a walk outside, doing an activity with family or others outside the care facility.
Household activities: domestic activities (setting the table, cleaning dishes, etc.), cooking or preparing a meal, taking care of plants.
Recreational activities: exercising, sports, dancing, spiritual or religious activities, handcrafts, arts, musig, singing, playing cards, plaing a game, doing a puzzle, reading, writing, crossword puzzle, using the comuter, sensory stimulation, watching television or listening to the radio.
Walking: walking around the living room or the building and is relaxed (not wandering).
Other activities: activities that do not match any of the other categories (e.g. smoking, participating in an informational event).
Passive activities: sitting or lying, there is no activity taking place.
Meaningless (repetitive) behaviour: tapping on table, rubbing hands without reason, picking, wandering, mumbling, etc (see manual of the MEDLO‐tool).
Resting: being put to rest by a caregiver (either in bed or in a wheelchair) and only scoredy if the resident is actually resting and awake.
Sleeping: being put to rest by a caregiver (either in bed or in a wheelchair) and only scored if the resident is actually sleeping.
Counts as engagement in purposeful activities: active engagement (obvious participation with the activity), passive engagement (looking or having a clear focus on the activity) or active engagement with something else.
Counts as engagement in purposeless activities, resting or sleeping: no engagement whilst staring/no focus, no engagement whilst resting or sleeping.
FIGURE 1.
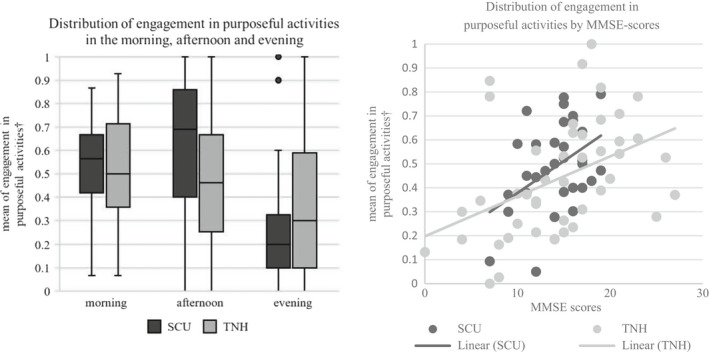
Distribution of engagement in purposeful activities in the morning, afternoon, and evening as well as by MMSE scores in SCU and TNH. SCU, special care unit; TNH, traditional nursing home. † shows the distribution of the aggregated data (=mean) per resident of engagement in purposeful activities; 0 = engagement in purposeless activities, resting or sleeping at all momentary assessments, 1 = engagement in purposeful activities at all momentary assessments
TABLE 3.
Mean scores of engagement in purposeful activities, social interaction, agitation and emotion
|
SCU mean (SD) |
TNH mean (SD) |
Cohen's d | |
|---|---|---|---|
| Engagement in purposeful activities: no (0)/yes (1) | |||
| Morning (n = 32/47 residents) | 0.51 (0.21) | 0.49 (0.21) | −0.095 |
| Afternoon (n = 32/48 residents) | 0.63 (0.27) | 0.48 (0.28) | −0.545b |
| Evening (n = 24/44 residents) | 0.26 (0.28) | 0.36 (0.32) | 0.333a |
| Engagement in social interaction: no (0)/yes (1) | |||
| Morning (n = 32/47 residents) | 0.25 (0.20) | 0.25 (0.18) | 0.000 |
| Afternoon (n = 32/48 residents) | 0.37 (0.24) | 0.15 (0.15) | −1.009c |
| Evening (n = 24/44 residents) | 0.12 (0.18) | 0.11 (0.15) | −0.060 |
| Pittsburgh Agitation Scale (0–16) | |||
| Morning (n = 32/47 residents) | 0.19 (0.31) | 0.26 (0.47) | 0.176 |
| Afternoon (n = 32/48 residents) | 0.12 (0.24) | 0.25 (0.57) | 0.297a |
| Evening (n = 24/44 residents) | 0.25 (0.52) | 0.23 (0.45) | −0.041 |
| Observed Emotion Rating Scale (0–10) | |||
| Morning (n = 32/47 residents) | 7.38 (0.61) | 7.55 (0.74) | 0.251a |
| Afternoon (n = 32/48 residents) | 7.72 (0.65) | 7.63 (0.57) | −0.147 |
| Evening (n = 24/44 residents) | 7.50 (0.75) | 7.62 (0.54) | 0.168 |
Abbreviations: SCU, special care unit; TNH, traditional nursing home; SD, standard deviation.
Small effect at d > 0.2.
Medium effect at d > 0.5.
Large effect at d > 0.8.
Figure 1 also depicts the distribution of engagement in purposeful activities depending on MMSE scores in SCU and TNH. Cognitive impairment had a negative influence on engagement in purposeful activities in both groups: the mean engagement in purposeful activities declined with lower MMSE scores. However, SCU residents with MMSE scores above 10 performed purposeful activities more often than TNH residents with the same MMSE scores.
Engagement in social interactions
The observed persons did not engage in social interactions during the predominant part of the assessments (see Table 3). However, social interactions were more frequently observed in SCU than in TNH (25.6% vs. 17.1%). Differences in engagement in social interactions between the groups were mainly observed in the afternoon: persons with dementia in SCU interacted socially in 27% of the momentary assessments, compared to 15% in TNH (SCU: mean = 0.37; SD = 0.24; TNH: mean = 0.15; SD = 0.15). In the morning and in the evening, engagements in social interactions were rather similar in both groups. In the morning, social interactions occurred in approximately a quarter (SCU: mean = 0.25; SD = 0.20; TNH: mean = 0.25; SD = 0.18), and in the evening in one‐eighth of the momentary assessments (SCU: mean = 0.12; SD = 0.18; TNH: mean = 0.11; SD = 0.15).
In Figure 2, differences in MMSE scores in the distribution of engagement in social interactions in SCU and TNH are displayed. Residents with MMSE scores between 19 and 8 showed a higher chance of social interaction in the SCU than in TNH. In SCU, the chance for engagement in social interactions declined with lower MMSE scores. In the data of TNH, a similar, but considerably less strong trend was observed, all included persons with dementia engaged less in social interactions than in SCU.
FIGURE 2.
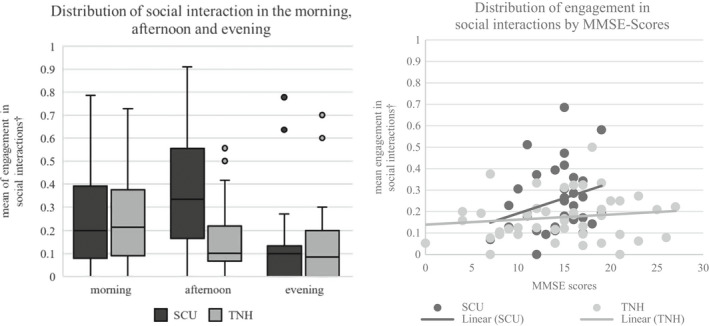
Distribution of engagement in social interactions in the morning, afternoon, and evening as well as by MMSE scores in SCU and TNH. SCU, special care unit; TNH, traditional nursing home. † shows the distribution of the aggregated data (=mean) per resident of engagement in social interactions; 0 = no engagement in social interaction at all momentary assessments, 1 = engagement in social interactions at all momentary assessments
Most frequently, persons with dementia interacted with staff members (SCU 46.5% vs. TNH 58.7%) and other residents (SCU 36.6% vs. TNH 25.1%). SCU residents interacted socially with each other approximately 10% points more than TNH residents, who on the other side engaged more often in conversations with staff members. Interactions with family members, friends, or others (e.g. visitors of other residents, children groups, visiting service members) were observed seldomly (see Table 4).
TABLE 4.
Interaction partners in the observed social interactions in SCU and TNH
|
SCU n = 284 social interactions n of social interactions (%) |
TNH n = 283 social interactions n of social interactions (%) |
|
|---|---|---|
| Staff members | 132 (46.5) | 166 (58.7) |
| Other residents | 104 (36.6) | 71 (25.1) |
| Family members and friends | 13 (4.6) | 7 (2.5) |
| Others | 16 (5.6) | 29 (10.2) |
| Combination of these groups | 19 (6.7) | 10 (3.5) |
Differences between SCU and TNH in social interaction partners could not be calculated due to low frequencies in some categories.
Abbreviations: SCU, special care unit; TNH, traditional nursing home.
Location
In comparison with TNH, residents of SCU spent more time in communal areas in the morning (56.8% vs. 45.7%, p = 0.001, see Table 5) and afternoon (70.0% vs. 47.9%, p < 0.001). Residents spent the evenings mostly in their own rooms (77.9% vs. 85.7%, p < 0.001).
TABLE 5.
Frequencies of locations in the morning, afternoon, and evening
|
SCU n of momentary assessments (%) |
TNH n of momentary assessments (%) |
|
|---|---|---|
| Morning (n = 489/624 momentary assessments, p = 0.001*) | ||
| Own room | 168 (34.4) | 286 (45.8) |
| Bathroom/toilet | 11 (2.2) | 16 (2.6) |
| Communal area on the ward | 280 (56.8) | 285 (45.7) |
| Corridor | 17 (3.5) | 14 (2.2) |
| Communal area off the ward | 13 (2.7) | 20(3.2) |
| Outside | 0 (0) | 3 (0.5) |
| Afternoon (n = 407/589 momentary assessments, p < 0.001*) | ||
| Own room | 61 (15) | 235 (38.7) |
| Bathroom/toilet | 2 (0.5) | 4 (0.7) |
| Communal area on the ward | 285 (70) | 282 (47.9) |
| Corridor | 25 (6.1) | 29 (4.9) |
| Communal area off the ward | 34 (8.4) | 30 (5.1) |
| Outside | 0 (0) | 9 (1.5) |
| Evening (n = 308/495 momentary assessments, p < 0.001*) | ||
| Own room | 240 (77.9) | 424 (85.7) |
| Bathroom/toilet | 0 (0) | 10 (2.0) |
| Communal area on the ward | 33 (10.7) | 43 (8.7) |
| Corridor | 26 (8.4) | 16 (3.2) |
| Communal area off the ward | 9 (2.9) | 1 (0.2) |
| Outside | 0 (0) | 1 (0.2) |
Abbreviations: SCU, special care unit; TNH, traditional nursing home.
Chi‐square test, significant at p < 0.05
Agitation
Agitation level, measured with the Pittsburgh Agitation scale, ranging from 0 (no agitation) to 16 (highest level of agitation), was relatively low in both groups, with mean scores <1. Agitation was less often observed in SCU than in TNH in the morning and afternoon (see Table 3). The agitation level in the TNH was evenly distributed, whereas in the SCU, it was highest in the evening. No significant differences between the groups were found.
Emotions
The scores of the OERS were relatively stable in the three sessions and homogeneous in SCU and TNH (see Table 3). The rather high mean values, ranging from 7.38 to 7.72, were mostly the result of the absence of negative emotions. In most momentary assessments, residents were generally alert but did not show either positive (pleasure) or negative (anger, anxiety/fear and sadness) emotions.
Generalised linear mixed models (GLMM) of engagement in purposeful activities and social interactions
GLMMs were calculated for the primary outcomes, engagement in purposeful activities and engagement in social interactions, and the results of the main and sensitivity analyses are depicted in Table 6. The main analyses for engagement in purposeful activities indicated rather similar chances in the morning in SCU and TNH, a 2.238 higher chance for engagement in purposeful activities in SCU in the afternoon (p < 0.001) and a slightly smaller chance in SCU in the evening (adjusted OR = 0.857; p = 0.570). For the matched data of the sensitivity analyses, based on gender and MMSE scores, the difference in the afternoon was even larger (adjusted OR = 2.870; p < 0.001). For engagement in social interactions, we again observed only small differences between SCU and TNH in the morning and evening, but a 3.25 higher chance for engagement in social interactions in SCU in the afternoon (see Table 6). The sensitivity analysis yielded similar results as the main analysis by also indicating a significantly higher chance for social interaction in the SCU in the afternoon compared to TNH.
TABLE 6.
Results of generalised linear mixed models for the primary outcomes
| Main analyses | Sensitivity analyses† (matching for gender and MMSE scores) | |||||
|---|---|---|---|---|---|---|
| Adjusted odds ratio | Confidence interval 95% | p‐value | Adjusted odds ratio | Confidence interval 95% | p‐value | |
| Engagement in purposeful activities | ||||||
| Morning | 1.092 | 0.680, 1.752 | 0.716 | 1.364 | 0.817, 2.276 | 0.235 |
| Afternoon | 2.238 | 1.374, 3.645 | <0.001* | 2.870 | 1.697, 4.855 | <0.001* |
| Evening | 0.857 | 0.504, 1.458 | 0.570 | 0.716 | 0.390, 1.315 | 0.282 |
| MMSE scores | 1.101 | 1.055, 1.149 | <0.001* | 1.223 | 1.140, 1.313 | <0.001* |
| Engagement in social interaction | ||||||
| Morning | 0.891 | 0.589, 1348 | 0.585 | 0.946 | 0.547, 1.636 | 0.842 |
| Afternoon | 3.250 | 2.107, 5.013 | <0.001* | 2.970 | 1.694, 5.209 | <0.001* |
| Evening | 0.978 | 0.567, 1.687 | 0.936 | 1.328 | 0.651, 2.708 | 0.435 |
| Gender | 0.531 | 0.352, 0.801 | 0.003* | 0.505 | 0.261, 0.977 | 0.043* |
Abbreviations: SCU, special care unit; TNH, traditional nursing home.
Significant at p < 0.05
For the analysis of engagement in purposeful activity, the model considering MMSE scores as a further fixed effect factor was the most appropriate one (p‐value: sex = 0.629; MMSE < 0.001). For the analysis of engagement in social interactions, the model considering gender as a further fixed effect factor was the most appropriate one (p‐values: sex = 0.003; MMSE < 0.171).
DISCUSSION
The study aimed to evaluate the outcomes of an existing care concept of a SCU and showed that SCU residents engaged more often in activities and social interactions during the afternoon than TNH residents. No significant differences were found in the morning and evening. However, in both settings persons with dementia spent half of their time without engaging in activities and social interactions. These results and further results of the outcome evaluation are used together with those of the process evaluation for the assessment of the initial change model (step 5 according to van Belle et al. [26]) and the revision of the programme theory (step 6). The revised programme theory answers the overarching question of the effect of the SCU care concept on persons with dementia and nursing staff and describes the mechanisms triggered by the interventions and the outcomes they produce.
The findings reinforce those of Abbott, Sefcik and van Haitsma [33], and complement those of a study also using the MEDLO‐tool in different long‐term care settings [6]. De Boer et al. [6] also found significant differences between the settings but did not report variations across periods in time. The distinction between periods in time shows insights into undeveloped potentials as well as ceilings for engagement across settings. The high overall engagement in the morning, also described by van Alphen et al. [11], results from morning routines, including self‐care activities, breakfast, a variety of organised (group) activities in the late morning and high staff presence. In the afternoon staff presence declines in the TNHs and less group activities are scheduled. This resulted in fewer and mainly self‐initiated, passive activities, such as watching TV, and less social interactions in the TNH. However, staff members in the SCU were present in the communal area the entire afternoon, continuously engaging residents in social and leisure activities. These activities were mostly brief and addressed persons individually on one‐to‐one levels, for example, singing a favourite song together or reading the horoscope and talking about it. According to Helgesen, Larsson and Athlin [34] as well as Dobbs et al. [35], staff presence promotes engagement in activities and interactions, as persons with dementia often rely on others to initiate activities. In SCUs, residents and staff members as well as volunteers and family members form a caring community that facilitates participation in activities and social life throughout the day [36]. In the evening, fewer activities and social interactions were observed in SCUs, with most residents sleeping – this trend was less prominent in TNHs. The higher activity levels in the SCUs in the afternoon could be a possible explanation for the increased tiredness of these residents in the evening which would correspond with a daily routine that society considers ‘normal’. Persons with moderate dementia seem to benefit the most from the SCU, as with increasing cognitive impairment, displayed by decreasing MMSE values, the engagement in activity and social interactions declined and approximated in both settings.
In both settings in the current study, persons with dementia spent half of their time without engaging in activities or social interaction. However, there are indications that a prolonged lack of stimulation is detrimental for persons with dementia [9, 10]. Eventhough we do not know how much activity and interaction a person with dementia prefers or needs, the high amount not engaging, and its negative consequences suggest a need for interventions facilitating engagement in activities and social interactions. As this study suggests, SCUs seem to succeed better in engaging persons with dementia in activities and social interactions. A probable reason for that may be the longer time periods residents of SCUs spent in communal areas, where engagement is more likely to take place. Social interactions occur more often in communal areas that also provide privacy [37]. These are more often found in SCUs with a small‐scale household‐like design than in TNHs. Additionally, staff members were more present in the SCUs throughout the day, thereby facilitating engagement. Furthermore, the SCU offered activities and interactions tailored to a person's characteristics and interests as well as to the social and physical environment.
In the current study, agitation levels and emotions did not differ significantly between the settings. Agitation was only sporadically observed. Similar results were found in other studies [6, 38]. Consequently, the data do not support a conclusion on whether agitation may hinder engagement in activities or social interactions. Furthermore, emotions did not differ between the settings, and negative as well as positive emotions could only be observed seldomly. Conversely, Beerens et al. [12] reported positive mood in 73% of all observations of persons with dementia in different institutional long‐term care settings and found an association with engagement in activities and social interaction.
Limitations
The study focussed on one specific care concept, which led to a small sample due to the small number of eligible residents in the SCU but increased the internal validity and enabled substantial results for the specific complex intervention and setting. Furthermore, only few persons with mild or severe dementia participated in the study. This applies especially for the SCU, as the target group of the care concept consists of persons with moderate dementia. The MEDLO‐tool assesses the quantity of time spent with engagement in activities and social interactions but does not allow for conclusions on how the amount of engagement is experienced by the persons with dementia. A further restriction is that each resident was only observed once at each time point and that no conclusions about the duration of single engagements or non‐engagements can be drawn. However, a practicable realisation of the project required this procedure of data collection and resulted in comparable data between groups.
Moreover, the absent differences between SCU and TNH in agitation and emotions may be affected by the assessment method used. Observations of agitation and emotions, especially of persons with dementia, are prone to be confounded by intra‐ and interindividual variability in expression and frequency [39].
CONCLUSION
The evaluation of the care concept in the SCU shows a significantly higher chance for engagement in activities and social interactions in the afternoon than in the TNH. Due to established busy routines, engagement was high in both groups in the morning. In the evening, there was a trend that SCU residents spent more time sleeping and resting. The results are favourable for the care concept. However, residents of both groups did not engage in purposeful activities or social interactions the predominant part of the time. Despite not knowing how much activity and interaction one person with dementia prefers or needs, the high amount of no engagement during the day suggests a need for interventions targeting the issue. Further research is needed to examine the types and extent of engagement in activity and social interactions needed and preferred by persons with dementia. The results of further research can be used to investigate appropriate and feasible approaches and interventions to address the issue. Within the framework of theory‐driven evaluation, the results of the study in conjunction with those of the process evaluation contribute to the revised programme theory and, subsequently, serve to further develop the care concept of the SCU.
CONFLICT OF INTEREST
The authors declare that even though the study was supported by SeneCura, the funder did not influence the study or its outcomes, and the authors are free to report any unfavourable results. The authors have no conflicts of interest to report.
AUTHOR CONTRIBUTION
All authors have made substantial contributions to the conception and the design of the study. LA and TN collected data, whereas LA, FF and HM where involved in data analysis, all authors were involved in the interpretation of the data. LA drafted the manuscript and TN, FF, SB and HM revised it critically and made important contributions. All authors gave their final approval of the version to be published.
TRIAL REGISTRATION NUMBER
DRKS00011513.
APPROVAL OF ETHICS COMMITTEE
The ethics board of the German Society of Nursing Research approved this study (N° 16‐024).
ACKNOWLEDGEMENTS
The authors would like to thank all the staff members and managers at the study sites who gave valuable time effort and support for the co‐ordination of data collection.
Adlbrecht L, Nemeth T, Frommlet F, Bartholomeyczik S, Mayer H. Engagement in purposeful activities and social interactions amongst persons with dementia in special care units compared to traditional nursing homes: An observational study. Scand J Caring Sci. 2022;36:650–662. 10.1111/scs.13017
Funding information
The study was funded by SeneCura, the nursing home operator of the participating nursing homes in the study.
REFERENCES
- 1. Aasgaard HS, Landmark BT, Öresland S. Healthcare personnel’s experiences of enhancing social community for people living in dementia special care units. Nord J Nurs Res. 2017;37:186–93. [Google Scholar]
- 2. den Ouden M, Bleijlevens MHC, Meijers JMM, Zwakhalen SMG, Braun SM, Tan FES, et al. Daily (in)activities of nursing home residents in their wards: an observation study. J Am Med Dir Assoc. 2015;16:963–8. [DOI] [PubMed] [Google Scholar]
- 3. Tak SH, Kedia S, Tongumpun TM, Hong SH. Activity engagement: perspectives from nursing home residents with dementia. Educ Gerontol. 2015;41:182–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Morgan‐Brown M, Brangan J, McMahon R, Murphy B. Engagement and social interaction in dementia care settings. A call for occupational and social justice. Health Soc Care Community. 2019;27:400–8. [DOI] [PubMed] [Google Scholar]
- 5. Smit D, de Lange J, Willemse B, Twisk J, Pot AM. Activity involvement and quality of life of people at different stages of dementia in long term care facilities. Aging Ment Health. 2016;20:100–9. [DOI] [PubMed] [Google Scholar]
- 6. de Boer B, Hamers JPH, Zwakhalen SMG, Tan FES, Beerens HC, Verbeek H. Green care farms as innovative nursing homes, promoting activities and social interaction for people with dementia. J Am Med Dir Assoc. 2017;18:40–6. [DOI] [PubMed] [Google Scholar]
- 7. Bradshaw SA, Playford ED, Riazi A. Living well in care homes: a systematic review of qualitative studies. Age Ageing. 2012;41:429–40. [DOI] [PubMed] [Google Scholar]
- 8. Haugan G, Innstrand ST, Moksnes UK. The effect of nurse‐patient interaction on anxiety and depression in cognitively intact nursing home patients. J Clin Nurs. 2013;22:2192–205. [DOI] [PubMed] [Google Scholar]
- 9. Cohen‐Mansfield J, Dakheel‐Ali M, Marx MS. Engagement in persons with dementia: the concept and its measurement. Am J Geriatr Psychiatry. 2009;17:299–307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Cohen‐Mansfield J, Dakheel‐Ali M, Marx MS, Thein K, Regier NG. Which unmet needs contribute to behavior problems in persons with advanced dementia? Psychiatry Res. 2015;228:59–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. van Alphen HJM, Volkers KM, Blankevoort CG, Scherder EJA, Hortobágyi T, van Heuvelen MJG. Older adults with dementia are sedentary for most of the day. PLoS One. 2016;11:e0152457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Beerens HC, Zwakhalen SMG, Verbeek H, E.S. Tan F, Jolani S, Downs M, et al. The relation between mood, activity, and interaction in long‐term dementia care. Aging Ment Health. 2018;22:26–32. [DOI] [PubMed] [Google Scholar]
- 13. Sampaio A, Marques‐Aleixo I, Seabra A, Mota J, Marques E, Carvalho J. Physical fitness in institutionalized older adults with dementia: association with cognition, functional capacity and quality of life. Aging Clin Exp Res. 2020;32:2329–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Lara E, Caballero FF, Rico‐Uribe LA, Olaya B, Haro JM, Ayuso‐Mateos JL, et al. Are loneliness and social isolation associated with cognitive decline? Int J Geriatr Psychiatry. 2019;34:1613–22. [DOI] [PubMed] [Google Scholar]
- 15. Clarke N, Smith R, Wood J, Koskela S, Jones F, Hurley M. A qualitative interview study comparing and contrasting resident and staff perspectives of engaging in meaningful activity in a UK care home. Arch Gerontol Geriatr. 2019;83:257–62. [DOI] [PubMed] [Google Scholar]
- 16. Harnett T. Framing spaces in places: creating “respite spaces” in dementia care settings. Dementia. 2014;13:396–411. [DOI] [PubMed] [Google Scholar]
- 17. Andersen EM, Kristiansen ED, Rasmussen G. Routines of “sitting” and “enjoying ourselves” in the common room of a dementia unit. Logoped Phoniatr Vocol. 2019;44:23–30. [DOI] [PubMed] [Google Scholar]
- 18. Slettebø Å, Saeteren B, Caspari S, Lohne V, Rehnsfeldt AW, Heggestad AKT, et al. The significance of meaningful and enjoyable activities for nursing home resident’s experiences of dignity. Scand J Caring Sci. 2017;31:718–26. [DOI] [PubMed] [Google Scholar]
- 19. O'Rourke HM, Duggleby W, Fraser KD, Jerke L. Factors that affect quality of life from the perspective of people with dementia: a metasynthesis. J Am Geriatr Soc. 2015;63:24–38. [DOI] [PubMed] [Google Scholar]
- 20. Joyce NR, McGuire TG, Bartels SJ, Mitchell SL, Grabowski DC. The impact of dementia special care units on quality of care: an instrumental variables analysis. Health Serv Res. 2018;53:3657–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Palm R, Bartholomeyczik S. Specialist dementia care units. In: Michel JP, Beattie L, Finbarr M, Watson J, editors. Oxford textbook of geriatric medicine. Oxford: Oxford University Press; 2018. p. 281–5. [Google Scholar]
- 22. Gilbert J, Ward L, Gwinner K. Quality nursing care in dementia specific care units: a scoping review. Dementia. 2019;18:2140–57. [DOI] [PubMed] [Google Scholar]
- 23. Feil N. Group therapy in a home for the aged. Gerontologist. 1967;7:192–5. [DOI] [PubMed] [Google Scholar]
- 24. Adlbrecht L, Bartholomeyczik S, Mayer H. Entwicklung einer Programmtheorie als Grundlage für die Evaluation einer Demenzstation. Pflege. 2018;31:125–34. [DOI] [PubMed] [Google Scholar]
- 25. Chen HT. Practical program evaluation: theory‐driven evaluation and the integrated evaluation perspective. Los Angeles, London, New Dehli, Singapore, Washington DC: SAGE; 2015. [Google Scholar]
- 26. van Belle SB, Marchal B, Dubourg D, Kegels G. How to develop a theory‐driven evaluation design? Lessons learned from an adolescent sexual and reproductive health programme in West Africa. BMC Public Health. 2010;10:741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Folstein MF, Folstein SE, McHugh PR. Mini‐mental state. J Psychiatr Res. 1975;12:189–98. [DOI] [PubMed] [Google Scholar]
- 28. de Boer B, Beerens HC, Zwakhalen SMG, Tan FES, Hamers JPH, Verbeek H. Daily lives of residents with dementia in nursing homes: development of the Maastricht electronic daily life observation tool. Int Psychogeriatr. 2016;28:1333–43. [DOI] [PubMed] [Google Scholar]
- 29. Dichter MN, de Boer B, Verbeek H, Halek M. Benutzerhandbuch für die deutschsprachige Maastricht electronic daily life observation tool (MEDLO‐Tool). Version 1.0. Witten. Bonn, Germany: German Centre for Neurodegenerative Diseases (DZNE); 2018. [Google Scholar]
- 30. Lawton MP, Van Haitsma K, Klapper J. Observed affect in nursing home residents with Alzheimer’s disease. J Gerontol B Psychol Sci Soc Sci. 1996;51:P3–14. [DOI] [PubMed] [Google Scholar]
- 31. Phillips LJ, Reid‐Arndt SA, Pak Y. Effects of a creative expression intervention on emotions, communication, and quality of life in persons with dementia. Nurs Res. 2010;59:417–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Jeste DV, Palmer BW, Appelbaum PS, Golshan S, Glorioso D, Dunn LB, et al. A new brief instrument for assessing decisional capacity for clinical research. Arch Gen Psychiatry. 2007;64:966–74. [DOI] [PubMed] [Google Scholar]
- 33. Abbott KM, Sefcik JS, Van Haitsma K. Measuring social integration among residents in a dementia special care unit versus traditional nursing home: a pilot study. Dementia. 2017;16:388–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Helgesen AK, Larsson M, Athlin E. ‘Patient participation’ in everyday activities in special care units for persons with dementia in Norwegian nursing homes. Int J Older People Nurs. 2010;5:169–78. [DOI] [PubMed] [Google Scholar]
- 35. Dobbs D, Munn J, Zimmerman S, Boustani M, Williams CS, Sloane PD, et al. Characteristics associated with lower activity involvement in long‐term care residents with dementia. Gerontologist. 2005;45(suppl_1):81–6. [DOI] [PubMed] [Google Scholar]
- 36. Allison TA, Balbino RT, Covinsky KE. Caring community and relationship centred care on an end‐stage dementia special care unit. Age Ageing. 2019;48:727–34. 10.1093/ageing/afz030 [DOI] [PubMed] [Google Scholar]
- 37. Ferdous F, Moore KD. Field observations into the environmental soul: spatial configuration and social life for people experiencing dementia. Am J Alzheimers Dis Other Demen. 2015;30:209–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Kolanowski A, Litaker M. Social interaction, premorbid personality, and agitation in nursing home residents with dementia. Arch Psychiatr Nurs. 2006;20:12–20. [DOI] [PubMed] [Google Scholar]
- 39. Woods DL, Buckwalter K. Taking another look: thoughts on behavioral symptoms in dementia and their measurement. Healthcare (Basel). 2018;6:126. [DOI] [PMC free article] [PubMed] [Google Scholar]


