FIGURE 2.
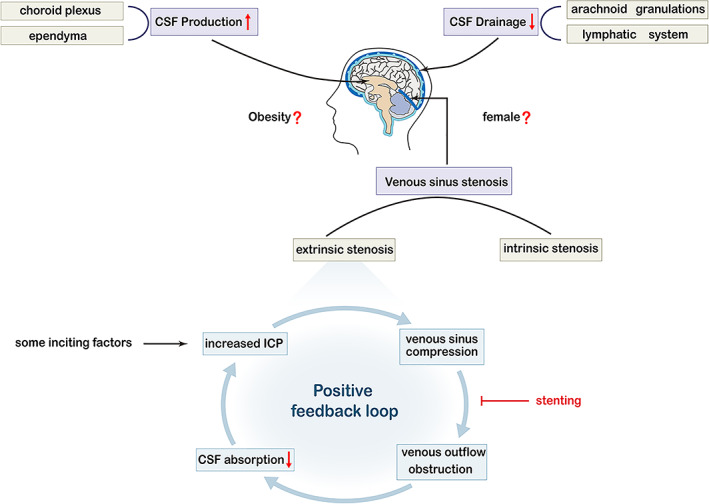
Schematic illustration of the possible pathophysiological mechanisms of idiopathic intracranial hypertension (IIH). Three primary mechanisms have been suggested to lead to IIH: enhanced cerebrospinal fluid (CSF) production at the choroid plexus or ependymal cells, decreased CSF drainage across the arachnoid granulations or lymphatic system, and venous sinus stenosis, which is the most important part of IIH and can be intrinsic or extrinsic. Some inciting factors such as weight gain and hormonal changes can cause an elevation in intracranial pressure (ICP), compressing the collapsible transverse sinus, causing extrinsic compression, blocking the venous outflow, leading to further venous hypertension, reducing the absorption of CSF, causing a consequent further elevation in ICP, and thus perpetuating the entire cycle. This positive feedback loop is referred to as the Starling‐like resistor. This vicious circle can be ended by some treatments, such as venous stenting. In addition, obesity and female sex are known predisposing risk factors for IIH development and may directly affect CSF dynamics.
