FIGURE 3.
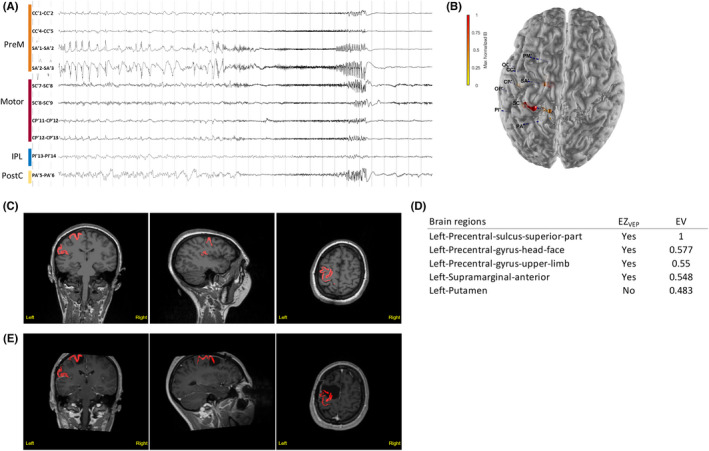
Illustrative Case 1. Motor–premotor epileptogenic zone (EZ) network is shown. The subject was a 23‐year‐old woman with sleep‐related, focal aware tonic seizures (tonic posture of the right arm) and negative magnetic resonance imaging (MRI). (A) Stereoelectroencephalographic (SEEG) recordings of a habitual seizure that starts from the left premotor and primary motor regions. IPL, inferior parietal lobule; PostC, the postcentral cortex; PreM, premotor cortex. (B) Patient's three‐dimensional (3D) brain mesh with SEEG electrodes. The maximal Epileptogenicity Index (EI) values are represented as spheres on the respective contacts according to a color map. The EI shows maximal epileptogenicity within the left supplementary motor area, the precentral gyrus and central sulcus, the precentral sulcus in its superior part, and the left caudal superior frontal sulcus. (C, D) Clinical report: heatmap (C) and list of brain regions with respective epileptogenicity values (EV; D). Regions identified as EZVEP (EZ predicted by the virtual epileptic patient) are displayed in red on the coronal, sagittal, and axial views of the patient's 3D T1‐MRI, also available as 3DViewer in HTML format. The color intensity varies according to the median of epileptogenicity. (E) Heatmap showing EZVEP regions on the postoperative T1‐MRI. The EZVEP included premotor–motor regions (left precentral sulcus, superior part; left precentral gyrus, head–face; and left precentral gyrus, upper limb) and left supramarginal gyrus, anterior. The patient benefited from a tailored resection of the left lateral and mesial premotor cortex, sparing the central region. The extent of resection of EZC (EZ defined by clinical analysis incorporating the EI) was estimated as 43% and that of EZVEP as 25%. The patient had residual focal aware seizures with clonic jerks of the right hand, a semiology suggestive of seizure origin in the primary motor cortex.
