FIGURE 4.
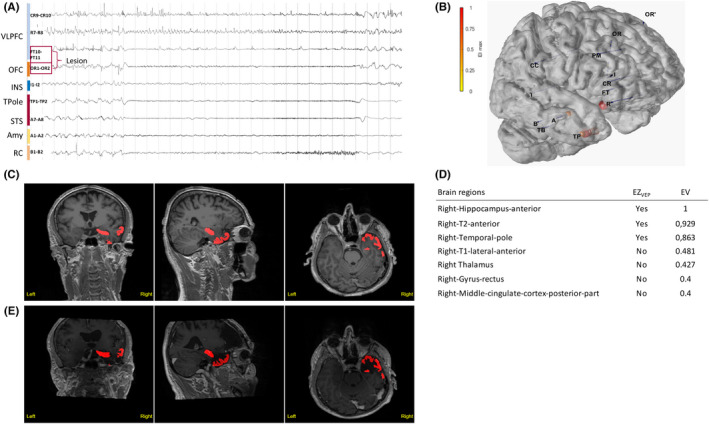
Illustrative Case 2. Temporofrontal epileptogenic zone (EZ) network is shown. A 56‐year‐old right‐handed man suffered from focal drug‐resistant epilepsy since the age of 11 years. He experienced weekly focal seizures with impaired awareness, with subjective signs including anxiety or fear, ascending epigastric sensation and chills, and as objective semiology, verbal and gestural automatisms, as well as hypermotor behavior during nocturnal seizures. His magnetic resonance imaging (MRI) was suggestive of a focal cortical dysplasia (FCD) within the right orbitofrontal cortex (OFC) and fronto‐opercular region. (A) Stereoelectroencephalography (SEEG) recordings of a habitual seizure. The seizure starts with rapid discharge in gamma‐band within the right anterior temporal structures and the OFC, whereas the opercular part of the lesion is not involved. Amy, amygdala; INS, insula; RC, rhinal cortex; STS, superior temporal sulcus; TPole, temporal pole; VLPFC, ventrolateral prefrontal cortex. (B) The patient's three‐dimensional (3D) brain mesh with implanted SEEG electrodes showing the maximal Epileptogenicity Index (EI) values within the right OFC, the amygdala, the temporal pole, and the superior temporal sulcus. (C, D) Clinical report. (C) Heatmap displays regions identified as EZVEP (EZ predicted by the virtual epileptic patient) in red on the patient's 3D T1‐MRI. (D) List of detected brain regions with respective epileptogenicity values (EV). (E) Heatmap showing EZVEP regions on the postoperative T1‐MRI. EZVEP included the right anterior temporal lobe (the temporal pole, the anterior hippocampus, and the anterior T2), but not the right orbitofrontal region. A tailored resection including the lateral prefrontal and orbitofrontal lesional and perilesional cortex, as well as the right anterior temporal lobe, led to complete seizure freedom (Engel Class I at 9‐year follow‐up), without any functional deficit. The extent of resection was 100% for both EZC (EZ defined by clinical analysis incorporating the EI) and EZVEP. The histopathological finding was right frontal FCD type 2b. The interpretation in this situation is not univocal. Either this region was not epileptogenic and resection could have spared it, or the region was epileptogenic and here the VEP lacks sensitivity.
