FIGURE 3.
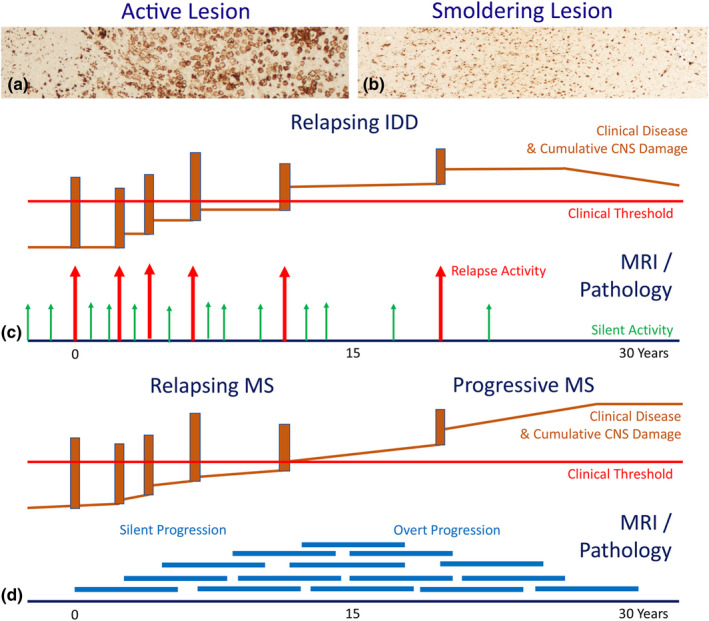
The difference between classic disease activity in acute or relapsing inflammatory demyelinating diseases and disease progression in chronic multiple sclerosis (MS). There are two different lesions types in inflammatory demyelinating diseases [30]: (a) The classic active lesions, characterized by profound inflammation, profound blood–brain barrier damage and synchronous active demyelination throughout the lesion with massive macrophage infiltration. (b) The chronic active (slowly expanding or smoldering) lesions, characterized by inflammation trapped behind a closed or repaired blood–brain barrier, profound microglia activation and moderate to minor ongoing active demyelination and axonal injury. These smoldering lesions gradually expand over years and fuse with adjacent smoldering lesions [31]. (c) Classic active lesions (arrows) are mainly seen in the relapsing stage of disease and are present in MS as well as in myelin oligodendrocyte glycoprotein antibody‐associated disease (MOGAD) and neuromyelitis optica spectrum disorders (NMOSD). When sufficiently severe and located in clinically eloquent regions, they are associated with a relapse of the disease, otherwise they contribute to silent disease activity. Neurodegeneration, associated with active lesions leads to relapse associated permanent non‐progressive neurological deficits. (d) Smoldering lesions (thick blue lines) show persistent low‐grade demyelination and neurodegeneration over several years. Such lesions accumulate in the late relapsing and early progressive stage of MS and give rise to disease progression, which may become clinically manifest as progressive MS, when the neurodegeneration exceeds the threshold of functional compensation [Colour figure can be viewed at wileyonlinelibrary.com]
