Abstract
Objectives:
Polypharmacy is common in home health care (HHC). This study examined the prevalence of medications associated with geriatric syndromes (MAGS), its predictors, and association with subsequent hospitalization in HHC.
Design:
Analysis of HHC electronic medical records, the Outcome and Assessment Information Set (OASIS), and Medicare HHC claims.
Setting and Participants:
A total of 6882 adults ≥65 years old receiving HHC in 2019 from a large, not-for-profit home health agency serving multiple counties in New York State.
Measures:
MAGS use was identified from active medications reconciled during HHC visits (HHC electronic medical records). MAGS use was operationalized as count and in quartiles. Hospitalization during the HHC episode was operationalized as a time-to-event variable (ie, number of days from HHC admission to hospitalization). We used regression analyses to identify predictors of MAGS use, and survival analyses to examine the association between MAGS and hospitalization.
Results:
Nearly all (98%) of the HHC patients used at least 1 MAGS and 41% of all active medications used by the sample were MAGS. More MAGS use was found in HHC patients who were community-referred, taking more medications, and having more diagnoses, depressive symptoms, and functional limitations. Adjusted for covariates, higher MAGS quartiles were not independently associated with the risk of hospitalization, but higher MAGS quartiles combined with multimorbidity (ie, having ≥10 diagnoses) were associated with a 2.3-fold increase in hospitalization risk (hazard ratio 2.24; 95% confidence interval: 1.61‒3.13; P < .001), relative to the lowest quartile of MAGS use and having <10 diagnoses.
Conclusions and Implications:
More than 40% of medications taken by HHC patients are MAGS. Multimorbidity and MAGS use collectively increased the risk of hospitalization by up to 2.3 times. HHC clinicians should carefully review patients’ medications and use information about MAGS to facilitate discussion about deprescribing with patients and their prescribers.
Keywords: Home health care, polypharmacy, medications associated with geriatric, syndromes, deprescribing
Older home health care (HHC) patients have an average of 9 chronic conditions and 15 medications,1,2 and experience frequent medication-related adverse events, including medication errors and discrepancies (67%–100%),3 medication nonadherence (50%),4 and particularly, use of potentially inappropriate medications (PIMs) (20%–93%).5–11 PIMs are medications with potentially unfavorable impact on older adults due to comorbidities, interactions, and/or liver or kidney impairment.12 PIMs may cause and/or worsen geriatric syndromes,13,14 which are also common in HHC, including cognitive impairment and delirium (33%e40%),1,2,15 depression (13.5%e28%),16 falls (6.4%),17 frailty (44%),18 and incontinence (10%).19,20 Saraf et al.13 used comprehensive literature review and expert panel discussion to develop a list of 513 medications associated with geriatric syndromes (MAGS) to supplement existing lists of PIMs (eg, Beers criteria) with a particular focus on 6 types of geriatric syndromes (ie, falls, delirium, cognitive impairment, depression, urinary incontinence, and weight loss).13 More than 42% of the MAGS are medications that are not already included in the Beers criteria, especially those related to depressive symptoms, weight loss, and urinary incontinence.13 Using the MAGS list, Saraf et al.13 found that, among 154 older post-acute skilled nursing facility patients, each was prescribed 14 medications, including approximately 6 MAGS, and more than 40% of all the medications were MAGS,13 underscoring the need for a holistic medication review for shared decision-making about deprescribing, including discontinuation, dosage adjustment, or continuation as prescribed with close monitoring of side effects and new/worsening geriatric syndromes.13
Care transitions in HHC represent unique opportunities for medication review and deprescribing. In 2019, more than 3.3 million Medicare beneficiaries received HHC services,21,22 which were provided through more than 100 million regular home visits (1–3 visits/ week) by multiple disciplines, including registered nurses, physical/ occupational therapists, social workers, and HHC aides.23 More than half of U.S. community-dwelling older adults with multimorbidity return home with HHC after hospital discharge,24 highlighting the importance of HHC medication review, particularly of MAGS, to deprescribing in post-acute care. To date, MAGS has not been examined in HHC.
This study had 3 objectives: (1) examine the prevalence of MAGS use in HHC patients, (2) examine the predictors of MAGS use, and (3) examine the association between MAGS use and subsequent hospitalization during the HHC episode. Because medication use is related to underlying medical complexity,13 we hypothesized that MAGS use was associated with patient characteristics (eg, multimorbidity) and increased risk of subsequent hospitalization during the HHC episode, particularly among patients with multimorbidity.
Methods
Data Source and Study Population
This study used data from the HHC electronic medical records, Outcome and Assessment Information Set (OASIS), and Medicare HHC claims from a large HHC agency in New York State. OASIS is a mandatory patient assessment tool used by all Medicare-certified HHC agencies to collect multidimensional patient information and outcomes. Most OASIS items have validated psychometric properties, particularly the cognitive and physical function domains (Cronbach’s α = 0.86−0.91; Cohen’s κ = 0.4−1.0)25 and hospitalization (high agreement with Medicare claims data; κ = 0.85).26 We extracted information about patient demographics, living arrangement, health status, cognitive and physical function, and hospitalization from OASIS. Medicare HHC claims data were used to extract information about HHC service utilization.
Because OASIS does not provide information on specific medications, we obtained medication data from HHC electronic medical records that are collected during medication reconciliation of HHC nurses using multiple data sources. Typically, HHC nurses first review the patient’s written prescriptions from the referring provider (eg, the prescription list on hospital discharge or from a primary care provider), including scheduled and pro-re-nata (PRN) prescriptions, regardless of the planned treatment duration. HHC nurses also visually inspect medication containers in the patient’s home to identify over-the-counter medications, dietary supplements, and prescriptions from other providers not known to the referring provider. HHC nurses then work with the patient/caregiver to determine if each medication is regularly taken by the patient (eg, >1−2/week) and if so, enter it to the HHC electronic medical records. Medication reconciliation is conducted in the initial HHC visit and updated on following visits. A medication was considered active if it existed on the list of reconciled medications on the initial HHC visit with a start date before the initial HHC visit.
Study Sample
The sample included Medicare beneficiaries ≥65 years old who received HHC services from this HHC agency with completed episodes in2019.For patients with multiple HHC episodes during January 1,2019 to December 31, 2019, only the first was included. We excluded long stay nursing home residents (n = 12), because they received medication management routinely from nursing home staff and represented a different population from community-dwelling patients. None of the sample died or was admitted to long-term care settings during the HHC episode. The final sample included 6882 unique HHC patients.
Variables
MAGS use
We used the list developed by Saraf et al.13 to identify MAGS use at the patient level using medication data from the HHC electronic medical records collected at HHC admission. Each medication was coded as a MAGS or non-MAGS. Medications (eg, opioids) that are associated with more than 1 geriatric syndrome (eg, delirium, cognitive impairment, and falls)were counted once to focus on the number of unique MAGS per patient MAGS count. The number of non-MAGS medications per patient was also counted. Both MAGS count and non-MAGS count were categorized into quartiles in inferential analyses.
Hospitalization
Hospitalization during the 60-day HHC episode [OASIS (M2410)] was operationalized as time-to-event (number of days between HHC admission to first hospitalization during the episode).
Covariates
Demographics, health status and caregiver support, and HHC service use were adjusted in all analyses. These variables were obtained from OASIS unless otherwise stated.
Demographic status included age, sex, race/ethnicity, marital status, living arrangement, and dual Medicare and Medicaid eligibility.
Health status included (1) referral source [acute care hospital or post-acute care facility, or community (eg, primary care providers)]; (2) total number of diagnoses [International Classification of Diseases, 10th Revision (ICD-10) codes (HHC claims); categorized as <10 versus ≥10 in interaction analysis with MAGS use (objective 3)]; (3) total number of active medications (HHC electronic medical records); (4) Alzheimer’s disease and related dementias [ADRD; diagnosis (ICD-10 codes; HHC claims) and/or moderate to severe cognitive impairment27–29]; (5) depressive symptoms [diagnosis (ICD-10 codes; HHC claims) and/or Patient Health Questionnaire-2 score ≥2]16; and (6) limitations in activities of daily living (ADLs; grooming, dressing upper body, dressing lower body, bathing, toilet transferring, toilet hygiene, transferring, ambulation, and eating; ranging from 0 to 9, with higher score indicating more limitations).30
Caregiver support was measured by patient self-report and HHC clinicians’ assessment of the availability and frequency of caregiver support and categorized as “adequate caregiver support” and “inadequate caregiver support.”
HHC service use was measured as weekly HHC intensity: average number of HHC visits each patient received from all disciplines per week during the HHC episode (HHC claims).28,31 The duration of the HHC episode was winsorized at 60 days, because it is the maximal duration of 1 Medicare-reimbursed episode in 2019.22,32
Statistical Analysis
First, for objective 1, we calculated the MAGS count per patient, the proportion of MAGS among all active medications, and the proportion of patients using ≥1 MAGS. Second, for objective 2, we conducted ordinal regression analyses with MAGS quartiles as the dependent variable and patient demographic, health, caregiver support, and HHC use variables as independent variables. Third, for objective 3, we used the Cox proportional hazards model to examine the association between MAGS quartiles (independent variable: reference = quartile 1) and time to hospitalization (dependent variable). In this model, total medication count was replaced by non-MAGS medication quartiles, because MAGS count was included into total medication count that caused duplication and high correlation between these 2 variables (correlation coefficient = 0.80, P < .001). In the analyses for objective 3, MAGS and non-MAGS medication counts were categorized into quartiles, because of their nonlinear associations with hospitalization. To examine the role of multimorbidity in the association between MAGS and hospitalization, we included interaction terms between MAGS quartiles and multimorbidity in the model. Scaled Schoenfeld residual analyses suggested that proportionality assumption was met in global tests and for all predictors (P > .05). Sensitivity analyses for objective 3 were conducted by categorizing MAGS count differently (ie, tertiles and quintiles). Statistical analyses were conducted using Stata 15.1 (StataCorp).
Results
The sample (6882) had an average age of 76.4 years (±10.17), was primarily White (85%), female (57%), not married (55%), and referred to HHC from an acute care hospital (64%). On average, the sample had 5.4 ADL limitations and 16.1 diagnoses on HHC admission, with osteoarthritis (43%), diabetes (33%), and heart failure (22%) being the most common. More than one-third (35%) had ADRD and approximately 40% had depressive symptoms. The HHC episode lasted 24 days (±14.9) on average, with approximately 7 total visits per week (Table 1).
Table 1.
Sample Characteristics
| Variable | Sample (N = 6882) |
|---|---|
| Age, mean (SD) | 76.4 (10.17) |
| Female, n (%) | 3901 (56.7) |
| Married, n (%) | 3113 (45.2) |
| Race/ethnicity, n (%) | |
| White | 5858 (85.1) |
| Non-White | 1024 (14.9) |
| Living arrangement, n (%) | |
| Living with others | 4200 (61.0) |
| Living alone | 1940 (28.2) |
| Living in aggregate settings | 742 (10.8) |
| Insurance, n (%) | |
| Medicare only | 6513 (94.6) |
| Medicare-Medicaid dual eligibility | 369 (5.4) |
| Referral source | |
| Acute care hospital | 4429 (64.4) |
| Post-acute care facilities | 774 (11.3) |
| Community | 1679 (24.4) |
| Total number of diagnoses, mean (SD) | 16.1 (11.19) |
| Number of active medications, mean (SD) | 12.5 (5.41) |
| Alzheimer disease and related dementias (diagnosis or symptom), n (%) | 2406 (35.0) |
| Depressive symptom (diagnosis or symptom), n (%) | 2716 (39.5) |
| Composite ADL limitation score, mean (SD) | 5.4 (1.01) |
| Caregiver assistance, n (%) | |
| Adequate caregiver assistance | 5488 (79.7) |
| Inadequate caregiver assistance | 1394 (20.3) |
| Days of index home health episode, mean (SD) | 24 (14.9) |
| Number of home health visits per week, mean (SD) | 6.8 (24.82) |
| Number of MAGS use per patient, mean (SD) | 5.1 (2.85) |
| Number of non-MAGS medications per patient, mean (SD) | 7.4 (3.55) |
Nearly all (98%) of the sample used at least 1 MAGS. On HHC admission, each HHC patient had an average of 13 total active medications, including 5 MAGS. Of the total 70,443 unique, active, reconciled medications used by the sample, 41% were MAGS. The 3 most common MAGS included metoprolol (2384, 3.4% of all 70,443 medications), oxycodone (2307, 3.3%), and gabapentin (1901, 2.7%) (see the full list of MAGS in Supplementary Table 1).
Adjusted ordinal regression showed that community referral (versus acute care referral), taking more non-MAGS medications, having more diagnoses, having depressive symptoms, and greater ADL limitations were consistently associated with higher MAGS quartiles, whereas older age, ADRD, and inadequate caregiver support were associated with lower MAGS quartiles (Table 2).
Table 2.
Predictors of Quartiles of MAGS Use
| Outcome: MAGS Quartiles | Relative Risk Ratio | P Value | 95% Confidence Interval | |
|---|---|---|---|---|
| Quartile 1 (0—3, mean = 2.13) | Base Outcome | |||
| Quartile 2 (4—5, mean = 4.47) | ||||
| Age | 0.987 | <.001 | 0.980 | 0.994 |
| Female | 0.990 | .883 | 0.868 | 1.130 |
| Married (vs not married) | 1.032 | .688 | 0.886 | 1.201 |
| Race/ethnicity | ||||
| Non-White (vs White) | 1.058 | .564 | 0.873 | 1.283 |
| Living arrangement (ref = living with others) | ||||
| Living alone | 1.211 | .023 | 1.026 | 1.428 |
| Living in aggregate settings (eg, assisted living) | 1.109 | .394 | 0.875 | 1.405 |
| Medicare-Medicaid dual eligible (vs Medicare only) | 0.994 | .969 | 0.720 | 1.371 |
| Referral source (ref: community) | ||||
| After hospitalization | 1.054 | .523 | 0.896 | 1.240 |
| Post-acute care settings (eg, inpatient rehab and skilled nursing facilities) | 0.774 | .027 | 0.618 | 0.971 |
| Quartiles of non-MAGS medications (ref = non-MAGS quartile 1, [0—5 non-MAGS medications, mean = 3.65]) | ||||
| Non-MAGS quartile 2 (6—7, mean = 6.50) | 1.725 | <.001 | 1.470 | 2.024 |
| Non-MAGS quartile 3 (8—10, mean 8.88) | 2.177 | <.001 | 1.843 | 2.571 |
| Non-MAGS quartile 4 (11—21, mean = 13.12) | 2.594 | <.001 | 2.062 | 3.263 |
| Total number of diagnoses | 1.030 | <.001 | 1.022 | 1.039 |
| Alzheimer disease and related dementias (diagnosis or symptoms) | 0.773 | .001 | 0.667 | 0.894 |
| Depressive symptoms | 1.392 | <.001 | 1.206 | 1.607 |
| ADL limitation score | 1.079 | .029 | 1.008 | 1.155 |
| Caregiver support (inadequate vs adequate) | 0.828 | .019 | 0.707 | 0.969 |
| Number of home health visits per wk | 0.998 | .241 | 0.995 | 1.001 |
| Duration of HHC episode (d) | 0.999 | .727 | 0.995 | 1.004 |
| Quartile 3 (6—7, mean = 6.44) | ||||
| Age | 0.971 | <.001 | 0.963 | 0.979 |
| Female | 0.930 | .334 | 0.802 | 1.078 |
| Married (vs not married) | 1.004 | .965 | 0.846 | 1.191 |
| Race/ethnicity | ||||
| Non-White (vs White) | 1.146 | .207 | 0.928 | 1.415 |
| Living arrangement (ref = living with others) | ||||
| Living alone | 1.070 | .479 | 0.887 | 1.290 |
| Living in aggregate settings (eg, assisted living) | 1.027 | .844 | 0.789 | 1.336 |
| Medicare-Medicaid dual eligible (vs Medicare only) | 1.011 | .949 | 0.717 | 1.426 |
| Referral source (ref: community) | ||||
| After hospitalization | 0.968 | .727 | 0.808 | 1.160 |
| Post-acute care settings (eg, inpatient rehab and skilled nursing facilities) | 0.580 | <.001 | 0.447 | 0.752 |
| Quartiles of non-MAGS medications (ref = non-MAGS quartile 1, [0—5 non-MAGS medications, mean = 3.65]) | ||||
| Non-MAGS quartile 2 (6—7, mean = 6.50) | 1.897 | <.001 | 1.566 | 2.298 |
| Non-MAGS quartile 3 (8—10, mean 8.88) | 3.135 | <.001 | 2.595 | 3.787 |
| Non-MAGS quartile 4 (11—21, mean = 13.12) | 5.398 | <.001 | 4.250 | 6.855 |
| Total number of diagnoses | 1.050 | <.001 | 1.041 | 1.059 |
| Alzheimer disease and related dementias (diagnosis or symptom) | 0.856 | .061 | 0.727 | 1.007 |
| Depressive symptoms | 1.743 | <.001 | 1.491 | 2.038 |
| ADL limitation score | 1.115 | .005 | 1.033 | 1.204 |
| Caregiver support (inadequate vs adequate) | 0.794 | .011 | 0.665 | 0.948 |
| Number of home health visits per wk | 0.997 | .084 | 0.993 | 1.000 |
| Duration of HHC episode (d) | 1.000 | .951 | 0.995 | 1.005 |
| Quartile 4 (8—20, mean = 9.69) | ||||
| Age | 0.944 | <.001 | 0.935 | 0.953 |
| Female | 0.989 | .901 | 0.837 | 1.170 |
| Married (vs not married) | 1.002 | .983 | 0.824 | 1.218 |
| Race/ethnicity | ||||
| Non-White (vs White) | 1.217 | .100 | 0.963 | 1.538 |
| Living arrangement (ref = living with others) | ||||
| Living alone | 1.092 | .418 | 0.883 | 1.351 |
| Living in aggregate settings (eg, assisted living) | 0.929 | .636 | 0.684 | 1.261 |
| Medicare-Medicaid dual eligible (vs Medicare only) | 1.271 | .183 | 0.893 | 1.810 |
| Referral source (ref: community) | ||||
| After hospitalization | 0.933 | .512 | 0.759 | 1.147 |
| Post-acute care settings (eg, inpatient rehab and skilled nursing facilities) | 0.494 | <.001 | 0.367 | 0.666 |
| Quartiles of non-MAGS medications (ref = non-MAGS quartile 1, [0—5 non-MAGS medications, mean = 3.65]) | ||||
| Non-MAGS Quartile 2 (6—7, mean = 6.50) | 3.140 | <.001 | 2.453 | 4.019 |
| Non-MAGS Quartile 3 (8—10, mean 8.88) | 5.579 | <.001 | 4.393 | 7.084 |
| Non-MAGS quartile 4 (11—21, mean = 13.12) | 14.226 | <.001 | 10.813 | 18.716 |
| Total number of diagnoses | 1.074 | <.001 | 1.065 | 1.083 |
| Alzheimer disease and related dementias (diagnosis or symptoms) | 0.701 | <.001 | 0.582 | 0.845 |
| Depressive symptoms | 2.751 | <.001 | 2.312 | 3.274 |
| ADL limitation score | 1.226 | <.001 | 1.122 | 1.340 |
| Caregiver support (inadequate vs adequate) | 0.724 | .002 | 0.592 | 0.887 |
| Number of home health visits per wk | 0.998 | .282 | 0.996 | 1.001 |
| Duration of HHC episode (d) | 1.003 | .308 | 0.997 | 1.008 |
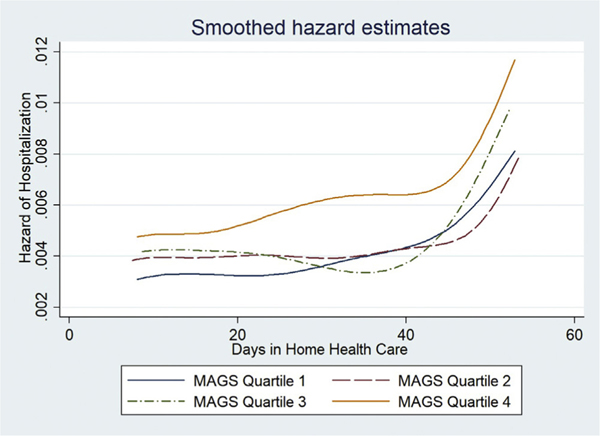
During the HHC episode, 11.4% of the sample was hospitalized (n = 784), with an average of 14 days between HHC admission and the first hospitalization. Adjusting for covariates, higher MAGS quartiles were not significantly associated with the risk of hospitalization during the HHC episode (Supplementary Table 2). The interaction between MAGS use and multimorbidity showed that HHC patients with higher quartiles of MAGS use and multimorbidity had greater risk of hospitalization (Table 3). Relative to patients with the lowest quartile of MAGS use and <10 diagnoses, those with the highest quartile of MAGS use and ≥10 diagnoses had a 2.3-fold increase in hospitalization risk during the HHC episode (hazard ratio 2.23; 95% confidence -Interval: 1.61e3.13; P < .001). Figure 1 illustrates that the survival estimates of hospitalization are generally higher in lower than higher quartiles of MAGS use, indicating higher quartiles of MAGS use being associated with greater hospitalization risk. Sensitivity analyses using tertiles and quintiles of MAGS count generated consistent results (Supplementary Tables 3 and 4).
Table 3.
Association Between Quartiles of MAGS Use and Hospitalization During the Index 60-Day HHC Episode (With Interaction)
| Outcome: Hospitalization | Hazard Ratio | P Value | 95% Confidence Interval | |
|---|---|---|---|---|
| Grouping based on MAGS quartiles and number of diagnoses Ref = MAGS quartile 1 [0—3, mean = 2.13] and total diagnoses <10 | ||||
| MAGS quartile 2 (4—5, mean = 4.47)*Diagnoses <10 | 0.852 | .479 | 0.548 | 1.327 |
| MAGS quartile 3 (6—7, mean = 6.44)* Diagnoses <10 | 1.397 | .158 | 0.878 | 2.223 |
| MAGS quartile 4 (8—20, mean = 9.69)* Diagnoses <10 | 1.126 | .697 | 0.620 | 2.044 |
| MAGS quartile 1*Diagnoses ≥10 | 1.969 | <.001 | 1.423 | 2.725 |
| MAGS quartile 2*Diagnoses ≥10 | 2.210 | <.001 | 1.610 | 3.034 |
| MAGS quartile 3*Diagnoses ≥10 | 2.020 | <.001 | 1.458 | 2.800 |
| MAGS quartile 4*Diagnoses ≥10 | 2.245 | <.001 | 1.609 | 3.132 |
| Quartiles of non-MAGS medications (ref = non-MAGS quartile 1, [0—5 non-MAGS medications, mean = 3.65]) | ||||
| Non-MAGS quartile 2 (6—7, mean = 6.50) | 0.845 | .131 | 0.679 | 1.052 |
| Non-MAGS quartile 3 (8—10, mean = 8.88) | 1.078 | .456 | 0.884 | 1.315 |
| Non-MAGS quartile 4 (11—21,mean = 13.12) | 1.290 | .019 | 1.043 | 1.596 |
| Age | 0.996 | .288 | 0.988 | 1.004 |
| Female | 0.854 | .035 | 0.737 | 0.989 |
| Married (vs not married) | 0.911 | .282 | 0.770 | 1.079 |
| Race/ethnicity (ref = White) | ||||
| Non-White | 1.151 | .158 | 0.947 | 1.398 |
| Living arrangement (ref = living with others) | ||||
| Living alone | 0.862 | .116 | 0.716 | 1.038 |
| Living in aggregate settings | 0.885 | .358 | 0.681 | 1.149 |
| Medicare-Medicaid dual eligibility (ref = Medicare only) | 1.153 | .347 | 0.857 | 1.550 |
| Referral source (ref: community) | ||||
| Acute care hospital | 1.504 | <.001 | 1.247 | 1.812 |
| Post-acute care facilities | 1.092 | .515 | 0.837 | 1.425 |
| Alzheimer disease and related dementias (diagnosis or symptom) | 1.110 | .195 | 0.948 | 1.299 |
| Depression (diagnosis of symptom) | 1.068 | .396 | 0.918 | 1.243 |
| Limitations in ADL activities | 1.017 | .665 | 0.942 | 1.097 |
| Caregiver support (ref = adequate caregiver assistance) | ||||
| Inadequate caregiver assistance | 0.918 | .351 | 0.767 | 1.099 |
| Average number of HHC visits per week | 1.004 | <.001 | 1.003 | 1.004 |
Fig. 1.
Smooth hazard estimates of hospitalization by MAGS quartiles.
Discussion
This study examined the prevalence and predictors of MAGS and its association with hospitalization among older HHC patients, with 3 principal findings. First, hyper-polypharmacy (ie, taking ≥10 medications concurrently) is common in the HHC population and, among these medications, MAGS were also common, as 41% of all medications used by HHC patients were MAGS. Second, patient characteristics were associated with MAGS use, suggesting that certain patients are at higher risk of MAGS use, including community-referred patients and patients with multimorbidity, depressive symptoms, and ADL limitations. Third, more MAGS use was associated with increased hospitalization risk during the HHC episode, but this association only existed among patients with multimorbidity.
The prevalence of MAGS in HHC is consistent with that of PIMs in this population (20%−67%),5–10 which was assessed using different tools (eg, Beers criteria12). Common MAGS identified in HHC (eg, analgesics and anticholinergics) are also common PIMs in HHC.6,7,9 Findings regarding leading predictors of MAGS used–polypharmacy and multi-morbidityd–are consistent with prior evidence on the predictors of PIMs.9,10 Specifically, the leading predictor of PIMs is total number of medications.33 Moreover, patients with multimorbidity often have multiple care providers, where lack of provider-provider communication and gaps in care coordination34 can increase MAGS use. The association between greater depressive symptoms and ADL limitations and more MAGS use is consistent with existing evidence, and it highlights the importance of assessing association with medication use when trying to understand or improve geriatric syndromes.14
Findings also suggest that certain groups in the HHC population, such as community-referred patients, are at particularly high risk for MAGS use. In the literature and in clinical practice, post-acute care HHC patients are known to be at risk for medication-related adverse events due to the multiple regimen changes during and after hospital discharge.34–36 The finding that community-referred HHC patients had more MAGS use than post-acute care HHC patients is unexpected and might be explained by their use of multiple providers, pharmacies, and frequent use of over-the-counter medications, as well as greater cognitive and functional impairment than post-acute care HHC patients.37 Further, it is likely the very HHC referral made for community patients, often by primary care providers, is for problems with medication use.37
It is unknown why older age, ADRD, and inadequate caregiver support in HHC were associated with less MAGS use. Possible explanations may include more clinician awareness of deprescribing of MAGS for patients with reduced life expectancy (eg, the oldest old and those with advanced ADRD38) and patients who are likely unable to manage multiple medications (eg, those without a caregiver).
Findings in this study add to our knowledge about PIMs use in a vulnerable population of older adultse–HHC patients, especially considering recent calls for additional insights on the appropriateness of medications (such as if a medication is PIM or MAGS) beyond the total number of medications in polypharmacy research.39 Multiple studies have demonstrated a close relationship between PIMs and hospitalization,9,34 especially among patients with multimorbidity and (hyper-)polypharmacy.40 For instance, a Swedish study showed that 41.3% of acute hospitalizations in patients with ADRD were related to medications.41 In a prior study examining PIMs using the Beers criteria in HHC, researchers found that HHC patients who used at least 1 PIM were 13% more likely to be hospitalized during the HHC episode.9
In this study, higher quartiles of MAGS use were not independently associated with hospitalization during the HHC episode. This may be because virtually all (98%) of the HHC patients used at least 1 MAGS, which, albeit highlighting the prevalent use of risky medications, might have muted the predictive power of MAGS toward hospitalization. Nevertheless, we found that HHC patients with multimorbidity are more likely to use MAGS and that multimorbidity and greater MAGS use collectively contributed to a 2.3-fold risk of hospitalization, suggesting the potential value of assessing MAGS use in routine HHC practice among patients with multimorbidity. Efforts that reduce the use of MAGS may play a role in reducing multimorbid HHC patients’ hospitalization risk, such as by facilitating deprescribing in collaboration with prescribers.42
MAGS and polypharmacy are complex, difficult-to-solve issues in clinical practice, calling for a concerted team approach involving the patients, providers, pharmacists, nurses, and other allied health professionals. To this end, the MAGS list can facilitate a holistic medication review and identify potential targets for patient-centered deprescribing,13 which may be challenging for patients with multimorbidity, as many medications are often necessary for symptom control. For instance, if a patient with polypharmacy has a new onset or worsening of fall, knowing a medication is on the Beers list and the MAGS list for increasing fall risk offers valuable information that can help the clinician bolster the rationale for deprescribing, such as continuing with this medication with intensive monitoring or replacing it with a safer alternative. Such knowledge will also help clinicians talk to patients about the risks and benefits of their medications. Systematic reviews showed mixed effects of deprescribing on falls43 and hospitalizations,44 suggesting the need for deprescribing interventions to consider symptoms and experiences that are important to patients (eg, geriatric syndromes), and findings in this study may inform future intervention development as such. Last, comprehensive medication review and deprescribing requires a significant amount of clinician time for older adults with multiple chronic conditions. Thus, for the MAGS list (or any other list of PIMs) to be routinely incorporated into practice, clinical decision support tools should be developed to build a workflow for automatic identification of PIMs or MAGS in the patient-specific context.
HHC nurses are uniquely positioned to facilitate deprescribing.42 First, HHC nurses review all the medications in the patient’s home, including expired medications, duplicates, and over-the-counter medications or supplements that may cause interactions with prescriptions (eg, gingko tablets, pain and sleep aides). Second, HHC nurses routinely support the patients and providers to reconcile medications,3,24,45 educate the patients/caregivers, and monitor symptoms,27,46 which can facilitate effective communication among providers about deprescribing.35,36,45 Third, HHC nurses already screen for geriatric syndromes (eg, depression, ADL limitation, incontinence, cognitive impairment, fall risk) using mandated patient assessment tools (eg, OASIS) on home visits. Therefore, they are ideally positioned to educate patients about medications that may contribute to these geriatric syndromes. Fourth, HHC nurses can help implement deprescribing, such as by helping the patients to safely dispose of deprescribed medications and teach the patients and caregivers to use tools (eg, daily pill boxes, medication reminder or dispenser) to ensure correct intake of medications.
Study Limitations
The study has several limitations. First, we used data from 1 HHC agency in New York State, because detailed medication data are not available in publicly available datasets (eg, OASIS). Thus, findings may not be generalizable to HHC agencies in other regions, although this study sample had comparable degrees of polypharmacy, as recently reported in other regions.47 Second, we focused on information collected in the initial nursing HHC visit because of its better accuracy than that collected in follow-up visits. Third, the crosssectional study design did not allow us to ascertain causality in the association between MAGS use and hospitalization risk, especially given that we did not know the causes of the hospitalizations. Fourth, we examined hospitalization risk using data from 1 HHC episode, and we did not have data on long-term outcomes following this episode.
Conclusions and Implications
Forty-one percent of all active medications taken by HHC patients are MAGS that may contribute to or worsen geriatric syndromes. HHC patients taking more MAGS and having multimorbidity are up to 2.3 times as likely to be hospitalized. The frequent home-based encounters of HHC clinicians (weekly for approximately 1 month) provide an ideal opportunity to identify potentially unnecessary MAGS and to provide follow-up after deprescribing, such as dose reduction and symptom monitoring.
Supplementary Material
Acknowledgments
The authors thank Mr. Timothy Claremont, Mr. Andrew Wooding, Ms. Bethany Rague, and Ms. Jessica Middleton at the University of Rochester Medical Center Home Care for assistance with acquisition of data.
Footnotes
This study was conducted with the support of the following funders: U.S. Deprescribing Research Network (1R24AG064025; JW: 2021e2022 Pilot Award); Alliance for Home Health Quality and Innovation (JW: 2021 Home Health Care Research Funding); Elaine C. Hubbard Center for Nursing Research on Aging (JW: Research Endowed Award), Terry Family Research Endowed Award (JW) and The Valerie and Frank Furth Fund (JW: The Valerie and Frank Furth Fund Award). The views expressed in this article are those of the authors and do not necessarily represent the view of the funders. The funders had no role in study design, data collection, analyses, or interpretation of results. This manuscript has not been previously published and is not under consideration in the same or substantially similar form in any other peer-reviewed media. All authors listed have contributed sufficiently to the project to be included as authors, and all of those who are qualified to be authors are listed in the author byline.
The authors declare no conflicts of interest, financial, personal, or other related to this manuscript.
References
- 1.Murtaugh C, Peng T, Totten A, Costello B, Moore S, Aykan H. Complexity in geriatric home healthcare. J Healthc Qual. 2009;31:34–43. [DOI] [PubMed] [Google Scholar]
- 2.Centers for Medicare and Medicaid Services (CMS). Home health qualitymeasures. 2019. Accessed January 5, 2020. https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HomeHealthQualityInits/Home-Health-Quality-Measures
- 3.Brody AA, Gibson B, Tresner-Kirsch D, et al. High prevalence of medication discrepancies between home health referrals and Centers for Medicare and Medicaid Services home health certification and plan of care and their potential to affect safety of vulnerable elderly adults. J Am Geriatr Soc. 2016;64: e166–e170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gray SL, Mahoney JE, Blough DK. Medication adherence in elderly patients receiving home health services following hospital discharge. Ann Pharmacother. 2001;35:539–545. [DOI] [PubMed] [Google Scholar]
- 5.Bao Y, Shao H, Bishop TF, Schackman BR, Bruce ML. Inappropriate medication in home health care. J Gen Intern Med. 2012;27:491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cannon KT, Choi MM, Zuniga MA. Potentially inappropriate medication use in elderly patients receiving home health care: A retrospective data analysis. Am J Geriatr Pharmacother. 2006;4:134–143. [DOI] [PubMed] [Google Scholar]
- 7.Meyer-Massetti C, Meier CR, Guglielmo BJ. The scope of drug-related problems in the home care setting. Int J Clin Pharm. 2018;40:325–334. [DOI] [PubMed] [Google Scholar]
- 8.Tsao CH, Tsai CF, Lee YT, et al. Drug prescribing in the elderly receiving home care. Am J Med Sci. 2016;352:134–140. [DOI] [PubMed] [Google Scholar]
- 9.Lohman MC, Cotton BP, Zagaria AB, et al. Hospitalization risk and potentially inappropriate medications among Medicare home health nursing patients. J Gen Intern Med. 2017;32:1301–1308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cotton BP, Lohman MC, Brooks JM, et al. Prevalence of and factors related to prescription opioids, benzodiazepines, and hypnotics among medicare home health recipients. Home Healthc Now. 2017;35:304–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ibrahim IA, Kang E, Dansky KH. Polypharmacy and possible drug-drug interactions among diabetic patients receiving home health care services. Home Health Care Serv Q. 2005;24:87–99. [DOI] [PubMed] [Google Scholar]
- 12.American Geriatrics Society Beers Criteria Update Expert Panel. American Geriatrics Society 2019 updated AGS beers criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2019;67:674–694. [DOI] [PubMed] [Google Scholar]
- 13.Saraf AA, Petersen AW, Simmons SF, et al. Medications associated with geriatric syndromes and their prevalence in older hospitalized adults discharged to skilled nursing facilities. J Hosp Med. 2016;11:694e700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Inouye SK, Studenski S, Tinetti ME, Kuchel GA. Geriatric syndromes: clinical, research, and policy implications of a core geriatric concept. J Am Geriatr Soc. 2007;55:780–791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bond SM. Delirium at home: strategies for home health clinicians. Home Healthc Nurse. 2009;27:24e34. quiz 35−26. [DOI] [PubMed] [Google Scholar]
- 16.Wang J, Kearney JA, Jia H, Shang J. Mental health disorders in elderly people receiving home care: prevalence and correlates in the national U.S. population. Nurs Res. 2016;65:107–116. [DOI] [PubMed] [Google Scholar]
- 17.Lewis CL, Moutoux M, Slaughter M, Bailey SP. Characteristics of individuals who fell while receiving home health services. Phys Ther. 2004;84:23–32. [PubMed] [Google Scholar]
- 18.Wang J, Dietrich MS, Bell SP, Maxwell CA, Simmons SF, Kripalani S. Changes in vulnerability among older patients with cardiovascular disease in the first 90 days after hospital discharge: A secondary analysis of a cohort study. BMJ Open. 2019;9:e024766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Drennan VM, Rait G, Cole L, Grant R, Iliffe S. The prevalence of incontinence in people with cognitive impairment or dementia living at home: A systematic review. Neurourol Urodyn. 2013;32:314–324. [DOI] [PubMed] [Google Scholar]
- 20.Harris-Kojetin L, Sengupta M, Lendon JP, Rome V, Valverde R, Caffrey C. LongTerm Care Providers and Services Users in the United States, 2015−2016. National Center for Health Statistics, Vital and Health Statistics; Series 3, Number 43. 2019. [PubMed] [Google Scholar]
- 21.Medicare Payment Advisory Commission. March 2022 Report to the Congress: Medicare Payment Policy. The Medicare Payment Advisory Commission. 2022. Accessed April 28, 2022. https://www.medpac.gov/document/march-2022report-to-the-congress-medicare-payment-policy/ [Google Scholar]
- 22.O’Connor M, Hanlon A, Naylor MD, Bowles KH. The impact of home health length of stay and number of skilled nursing visits on hospitalization among Medicare-reimbursed skilled home health beneficiaries. Res Nurs Health. 2015; 38:257–267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Centers for Medicare and Medicaid Services. Home health services. 2021. Accessed May 25, 2021. https://www.medicare.gov/coverage/home-healthservices
- 24.Medicare Payment Advisory Commission. July 2021 Data Book: Health Care Spending and the Medicare Program. The Medicare Payment Advisory Commission. 2021. Accessed April 28, 2022. https://www.medpac.gov/document/http-medpac-gov-docs-default-source-data-book-july2021_medpac_databook_sec-pdf/ [Google Scholar]
- 25.O’Connor M, Davitt JK. The outcome and assessment information set (OASIS): a review of validity and reliability. Home Health Care Serv Q. 2012;31:267–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wolff JL, Meadow A, Weiss CO, Boyd CM, Leff B. Medicare home health patients’ transitions through acute and post-acute care settings. Med Care. 2008;46: 1188e1193. [DOI] [PubMed] [Google Scholar]
- 27.Wang J, Monroe TB, Simning A, et al. Pain management in home health care: relationship with dementia and facility admissions. Pain Manag Nurs. 2021;22: 36–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wang J, Caprio TV, Simning A, et al. Association between home health services and facility admission in older adults with and without Alzheimer’s disease and related dementias. J Am Med Dir Assoc. 2020;21:627–633.e9. [DOI] [PubMed] [Google Scholar]
- 29.Wang J, Caprio TV, Tempkin-Greener H, Cai X, Simning A, Li Y. Relationship of Medicare-Medicaid dual eligibility and dementia with unplanned facility admissions among Medicare home health care recipients. J Aging Health. 2020;32: 1178–1187. [DOI] [PubMed] [Google Scholar]
- 30.Madigan EA, Gordon N, Fortinsky RH, Koroukian SM, Piña I, Riggs JS. Predictors of functional capacity changes in a US population of Medicare home health care patients with heart failure. Arch Gerontol Geriatr. 2012;54:e300–e306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wang J, Liebel DV, Yu F, Caprio TV, Shang J. Inverse dose-response relationship between home health care services and rehospitalization in older adults. J Am Med Dir Assoc. 2019;20:736–742. [DOI] [PubMed] [Google Scholar]
- 32.Centers for Medicare and Medicaid Services (CMS). Home health PPS. 2019. Accessed July 1, 2019. https://www.cms.gov/Medicare/Medicare-Fee-forService-Payment/HomeHealthPPS/index.html
- 33.Scott IA, Anderson K, Freeman CR, Stowasser DA. First do no harm: A real need to deprescribe in older patients. Med J Aust. 2014;201:390–392. [DOI] [PubMed] [Google Scholar]
- 34.Squires A, Ridge L, Miner S, McDonald MV, Greenberg SA, Cortes T. Provider perspectives of medication complexity in home health care: A qualitative secondary data analysis. Med Care Res Rev. 2020;77:609–619. [DOI] [PubMed] [Google Scholar]
- 35.Jones CD, Jones J, Richard A, et al. “Connecting the dots”: A qualitative study of home health nurse perspectives on coordinating care for recently discharged patients. J Gen Intern Med. 2017;32:1114–1121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kollerup MG, Curtis T, Schantz Laursen B. Visiting nurses’ posthospital medication management in home health care: An ethnographic study. Scand J Caring Sci. 2018;32:222–232. [DOI] [PubMed] [Google Scholar]
- 37.Fout B, Plotzke M, Jung OS. Heterogeneity in Medicare home health patients by admission source. Home Health Care Management & Practice. 2019;30:9–15. [Google Scholar]
- 38.Niznik JD, Aspinall SL, Hanson LC, et al. Patterns of oral bisphosphonate deprescribing in older nursing home residents with dementia. Osteoporos Int. 2022;33:379–390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hanlon JT, Hajjar ER. Isn’t it time we stop counting the number of drugs to define polypharmacy in this new era of deprescribing and what related outcomes should be measured? J Am Med Dir Assoc. 2018;19:644–645. [DOI] [PubMed] [Google Scholar]
- 40.Parameswaran Nair N, Chalmers L, Peterson GM, Bereznicki BJ, Castelino RL, Bereznicki LR. Hospitalization in older patients due to adverse drug reactionsdthe need for a prediction tool. Clin Interv Aging. 2016;11:497–505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Gustafsson M, Sjölander M, Pfister B, Jonsson J, Schneede J, Lövheim H. Drugrelated hospital admissions among old people with dementia. Eur J Clin Pharmacol. 2016;72:1143–1153. [DOI] [PubMed] [Google Scholar]
- 42.Sun W, Tahsin F, Barakat-Haddad C, Turner JP, Haughian CR, Abbass-Dick J. Exploration of home care nurse’s experiences in deprescribing of medications: A qualitative descriptive study. BMJ Open. 2019;9:e025606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lee J, Negm A, Peters R, Wong EKC, Holbrook A. Deprescribing fall-risk increasing drugs (FRIDs) for the prevention of falls and fall-related complications: A systematic review and meta-analysis. BMJ Open. 2021;11: e035978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bloomfield HE, Greer N, Linsky AM, et al. Deprescribing for communitydwelling older adults: A systematic review and meta-analysis. J Gen Intern Med. 2020;35:3323–3332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wang J, Simmons S, Maxwell CA, Schlundt DG, Mion L. Home health nurses’ perspectives and care processes related to older persons’ frailty and depression: a mixed method pilot study. J Community Health Nurs. 2018;35:118–136. [DOI] [PubMed] [Google Scholar]
- 46.Brody AA, Guan C, Cortes T, Galvin JE. Development and testing of the Dementia Symptom Management at Home (DSM-H) program: An interprofessional home health care intervention to improve the quality of life for persons with dementia and their caregivers. Geriatr Nurs. 2016;37:200–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Champion C, Sockolow PS, Bowles KH, et al. Getting to complete and accurate medication lists during the transition to home health care. J Am Med Dir Assoc. 2021;22:1003–1008. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.