Abstract
During the COVID-19 pandemic in Japan, various measures have been implemented to prevent the spread of infection, including restrictions on human mobility. A dynamic fluctuation in the number of suicides has been observed during this period. The question is whether the increase/decrease in suicides during the pandemic is related to changes in human mobility. To answer the same, we estimated incidence rate ratios (IRR) of suicide for changes in human mobility using the relative number of suicides by month from March 2020 to September 2021, based on the same months in 2019 as reference. The IRR of suicide during the pandemic were significantly lower in the months when mobility decreased—in both the previous and current month—than in the months when mobility was stable; the IRR of suicide were statistically higher in the months with increased mobility compared with the stable months. The burden from a decrease in one's mobility, which might lead to an increase in suicide, may not occur immediately, as seen in the delayed effects of unemployment. It may be important to investigate people's mental health and stress levels after pandemic restrictions were relaxed. The findings may help practitioners and families consider the timing of intervention.
Keywords: Suicide; Human mobility; Restriction; COVID-19, Japan
1. Introduction
The coronavirus disease 2019 (COVID-19), caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), was first detected in December 2019 and continues today through several variants, persisting as a critical pandemic (Cirrincione et al., 2022). In Japan, COVID-19 infections began to spread in March 2020, with five waves, peaking in August 2021 (Ministry of Health Labour and Welfare, 2022). Since then, the number of infections has decreased sharply, and the declared state of emergency was lifted at the end of September 2021. However, the new variants have led to an increase in the number of infections once more (Karim and Karim, 2021), and Japan is in the midst of the sixth wave in early 2022.
These circumstances have led to several changes in people's lifestyles, such as the amount of teleworking; human mobility has been especially restricted worldwide (Zhang et al., 2022). In Japan, various messages have been issued and measures have been implemented during the pandemic; a state of emergency was also declared to contain the spread of the disease. However, when the disease was believed to be under control, the “Go To” campaign encouraged citizens to resume social activities (Anzai and Nishiura, 2021; Karako et al., 2021). Consequently, the pandemic has created a dynamic change in human mobility (Nagata et al., 2021), which might be reflected in the magnitude of the social impact of the various measures.
Changes in people's mobility can affect their mental health (Gimbrone et al., 2021). Recent reports investigated the positive association between reduced mobility and an increase in psychological distress (Devaraj and Patel, 2021), specifically, feeling lonely (Murayama et al., 2021) when one's mobility decreases. A decline in mobility may also associated with declining in people's well-being, (Chakrabarti et al., 2021) economic consequences and the frenzies and anxieties due to the unknown features of the new virus. In other words, changes in human mobility are an indicator that reflects various social changes, the related deterioration in mental health and well-being may be related to an increase in suicidal tendencies. Several studies have investigated the impact of the pandemic on mental health and suicide in Japan (Fushimi, 2021; Ueda et al., 2021).
Various studies have indicated that suicide trends in Japan changed shortly after the COVID-19 pandemic began (Anzai et al., 2021; Kikuchi et al., 2022; Tanaka and Okamoto, 2021). The studies showed that the number of suicides increased by 37% during the pandemic relative to pre-pandemic conditions, especially among women (Tanaka and Okamoto, 2021). However, in the early period of the COVID-19 pandemic, from March to June 2020, the number of suicides in Japan decreased (Anzai et al., 2021). Thus, the degree of increase in the number of suicides has fluctuated during the pandemic. This raises the question of whether changes in people's mobility were associated with changes in the number of suicides during the pandemic.
To answer this question, we investigated the relationship between changes in monthly human mobility (decrease, increase, and stable) and the number of suicides during the pandemic in the period between March 2020 and September 2021. In September 2021, Japan lifted its state of emergency at the end of the fifth wave. We attempted to evaluate the impact of the COVID-19 pandemic on suicide, in the period when human mobility was restricted as a result of various pandemic prevention measures and interventions under COVID-19, by assessing the association between the number of suicides and human mobility relative to the pre-pandemic period in 2019.
2. Methods
2.1. Data and materials
We collected data on the monthly number of suicides from Japan's National Police Agency from March 2020 to September 2021 as the COVID-19 pandemic period, and from January to December 2019 as the reference period. GPS-based location data of the ratio of population mobility during the COVID-19 pandemic period relative to that in 2019 were downloaded from the AGOOP Corp and Cabinet Office websites (2021) and data regarding population mobility in 2019 were taken from the Geospatial Information Authority of Japan (Geospatial Information Center, 2021). The monthly unemployment rate during the pandemic period and that in 2019 were obtained from the Statistics Bureau of Japan. As we only used publicly available aggregate data, a formal ethical review was not required for our study.
2.2. Measurements
As the main outcome, we evaluated the ratio of the number of suicides , for each gender , prefecture , and point of time (month) (; i.e., ) during the COVID-19 pandemic from March 2020 to September 2021, relative to the number of suicides, , in 2019 before the pandemic.
As the primary factor of interest, three categories of change in human mobility—decrease, increase, and stable—at time in each prefecture were defined as follows:
-
1)
We obtained the population mobility in prefecture in week at time during the pandemic period as and . and are the ratios of the number of people who visited (or stayed in) a particular point in prefecture , and “outside” and “inside” refer to their estimated residency (outside prefecture or inside) relative to that in 2019 for prefecture in week at time after March 2020. Note that residency excluded the same municipality from “inside.” and are people who visited a particular point in prefecture in the same week in month in 2019, and “outside” and “inside” indicated residency same as for and .
-
2)
As human mobility, the ratio of the total number of people who visited the point from inside and outside prefecture at time in the pandemic period relative to that in the same month in 2019 during the reference period, was calculated by , where and .
-
3)
The monthly changes in human mobility for prefecture between time and during the pandemic period were labeled as (decreased) for , (increased) for , and (stable) otherwise to evaluate the non-linear relationship between changes in human mobility and suicide.
2.3. Statistical analysis
First, we summarized the monthly number of suicides and the unemployment rate for the pandemic and the reference period. Second, we plotted the calculated human mobility during the pandemic. Third, we evaluated the impact of the change in human mobility from the previous month at time and on the ratio of suicide during the pandemic period relative to , based on the model as follows:
where is a Poisson distribution with mean , the superscript “T” means “transpose,” change in human mobility at time (i.e., changes in human mobility between time and ) , and are dummy variables indicating ; similarly, vector of dummy variable of change in human mobility at time , , gender , and the ratio of the unemployment rates at time , time , and = are also dummy variables indicating prefectures (reference: Okinawa). The model included the ratio of the unemployment rates at time relative to that in the same month in 2019 with logarithmic transformation to interchange the increasing and decreasing scales, and the delayed effects of the unemployment rates at time (Nordt et al., 2015). and are the coefficients to be estimated by using the generalized estimating equation method assuming repeated measures within prefecture that can consider the overdispersion of the number of suicides (Kruppa and Hothorn, 2021). The number of suicides in 2019, , was added to 1 to account for the case of 0 as the offset term. Based on the above model, the incidence rate ratios (IRRs) were estimated as the exponential transformed value of each coefficient with their 95% confidence intervals (CIs) estimated. We also performed univariate analysis for the variable changes in mobility; the model was adjusted only for gender, without including the unemployment rate. A sensitivity analysis was conducted, where the threshold for the definition of “stable” in human mobility was replaced with 10%. Furthermore, to consider the impact of the first three months after declaration of the state of emergency, a main analysis excluding data from March to May 2020 was also performed.
The significance level was set at for both sides of all statistical analyses. All statistical analyses were performed using R software version 4.1.2 (R Core Team, 2021).
3. Results
The number of monthly suicides during the COVID-19 pandemic in Japan varied from a minimum of 1356 to a maximum of 2210 (Table 1 ). The range of the number of monthly suicides in the pandemic period was larger than that in the reference period. The number of suicides per month per prefecture during the pandemic period ranged from 6.7 to 134.5, showing considerable variation among prefectures. The unemployment rate in the pandemic period ranged from 2.5% to 3.1%, which was larger than that in the reference period and greater than or equal to the maximum rate in the reference period.
Table 1.
Summary of suicide, human mobility, and unemployment rates during the pandemic period and the reference period.
| COVID-19 pandemic period(Mar 2020 – Sep 2021) | Reference period(Jan 2019 – Dec 2019) | |
|---|---|---|
| Total number of suicides for all prefectures per month, median [min, max] | ||
| Both genders | 1696 [1356, 2210] | 1520 [1420, 1700] |
| Male | 1112 [946, 1334] | 1046 [975, 1186] |
| Female | 589 [410, 876] | 467 [435, 522] |
| Average number of suicides for each prefecture throughout the perioda, median [min, max] | 22.7 [6.7, 134.5] | 13.2 [3.5, 113.3] |
| Average human mobility for each prefecture throughout the periodb, median [min, max], (%) | –34.9 [–18.6, –55.6] | – |
| Unemployment rate (%), median [min, max] | 2.9 [2.5,3.1] | 2.4 [2.2, 2.5] |
Average number of suicides for each prefecture throughout the period was derived as follows: (1) calculating arithmetic mean of the number of suicides by prefecture, (2) calculating the summary statistics value for each prefecture derived in (1).
Average human mobility for each prefecture throughout the period was derived as follows: (1) calculating arithmetic mean of human mobility by prefecture, (2) calculating the summary statistics value for each prefecture derived in (1).
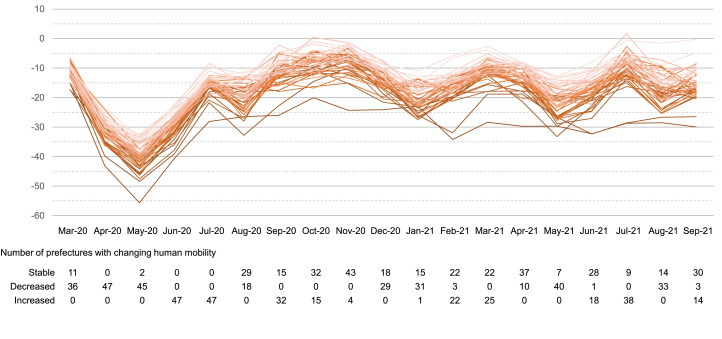
Monthly human mobility in each prefecture is plotted in Fig. 1 . The number of prefectures with changes in human mobility relative to the previous month is shown at the bottom of the figure. The waves of human mobility were similar in most prefectures. Human mobility in Japan during the pandemic was generally below 0%, ranging from –55.7% to 1.6%, relative to 2019. Decreased human mobility was observed in more than half of the prefectures in April, March, and December of 2020 and in January, May, and August of 2021. Increased human mobility was observed in approximately half of the prefectures in June, July, and September of 2020, and March and July of 2021.
Fig. 1.
Human mobility in each prefecture and changes in mobility from the previous month.
Here, the association between changes in human mobility and fluctuation in the number of suicides were evaluated; the estimated IRRs of the number of suicides and their 95% CIs in the pandemic period relative to those in 2019 are shown in Table 2 . In the univariate analysis, the ratio of suicides in the pandemic period relative to the reference was significantly lower in the months when human mobility decreased than in the months when human mobility was stable (IRR = 0.83, 95% CI (0.79–0.88) for the previous month; 0.80, 95% CI (0.77–0.84) for the current month). These results were similar in Model 1 adjusted for gender and the IRRs and 95% CIs were 0.87 (0.83–0.92) for the previous month and 0.85 (0.81–0.89) for the current month, respectively.
Table 2.
Estimated incidence rate ratio of suicide in the COVID-19 pandemic period.
| Univariatea |
Model 1b |
Model 2c |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| IRR | 95%CI | p-value | IRR | 95%CI | p-value | IRR | 95%CI | p-value | |
| Mobility changes at previous month | |||||||||
| Stable | 1.00 | Reference | – | 1.00 | Reference | – | 1.00 | Reference | – |
| Decreases | 0.83 | (0.79, 0.88) | <0.001 | 0.87 | (0.83, 0.92) | <0.001 | 0.93 | (0.89, 0.97) | 0.001 |
| Increases | 1.04 | (0.97, 1.11) | 0.258 | 1.03 | (0.97, 1.10) | 0.294 | 1.06 | (1.01, 1.10) | 0.031 |
| Mobility changes at current month | |||||||||
| Stable | 1.00 | Reference | – | 1.00 | Reference | – | 1.00 | Reference | – |
| Decreases | 0.80 | (0.77, 0.84) | <0.001 | 0.85 | (0.81, 0.89) | <0.001 | 0.89 | (0.85, 0.94) | <0.001 |
| Increases | 0.97 | (0.90, 1.05) | 0.510 | 1.00 | (0.91, 1.09) | 0.995 | 0.99 | (0.92, 1.05) | 0.689 |
IRR, Incidence rate ratio.
95%CI, 95% confidence interval.
Analysis are based on generalized estimating equations which considering the repeated measurement within prefectures including each variable of mobility change as an explanatory variable.
Analysis is based with generalized estimating equations which considering the repeated measurement within prefectures including categorized mobility change at time and , gender as explanatory variable.
Ratio of unemployment rate at time and relative to that of 2019, and indicator of prefectures were added to model 1.
Furthermore, in Model 2, adjusted for gender and unemployment rate relative to 2019, the IRRs and 95% CIs of the months when human mobility decreased were also significantly lower than 1.00: 0.93, 95% CI (0.89–0.97) for the previous month, and 0.89, 95% CI (0.85–0.94) for the current month. At the same time, in this model, the IRR was 1.06, 95% CI (1.01–1.10), and the ratio of the number of suicides in the pandemic to the reference period was statistically higher in the months when the previous month's human mobility increased, compared with the month when human mobility was stable. However, the IRR when the current month's mobility increased was not statistically significant.
The ratio of the number of suicides relative to the reference period was significantly lower for male than for female. In addition, the ratio of the number of suicides in the pandemic period relative to the reference period was significantly greater when the ratio of the unemployment rate relative to the reference period in the previous month was larger. (Supplemental Table 1)
In the sensitivity analysis in which the definition of “stable” in human mobility was replaced with 10%, similar results were observed for the factors that were significantly different in the above model. However, we also found that the number of suicides decreased when the current month's human mobility increased. Another sensitivity analysis excluding March to May 2020 showed no results that differed significantly from the analysis based on Model 2 with respect to presence or absence of statistically significant differences and direction of the estimates.
4. Discussion
This study focused on the association between the changes in human mobility and suicide rates during a particular period of the COVID-19 pandemic in Japan. Although no significant increase in suicide during the COVID-19 pandemic was observed in other developed countries (Liu et al., 2021; Perez et al., 2022; Pirkis et al., 2021), there was an increase in suicides in Japan, and several reports speculated that this was due to increased anxiety caused by restricted activity during the pandemic (Gunnell et al., 2020; McGinty et al., 2020; Murayama et al., 2021; Pirkis et al., 2022). However, no study has quantitatively evaluated these observations in Japan. Our research results, derived using data from the National Police Agency, which collects all suicide data in Japan, revealed that changes in human mobility were related to the timing of the increase and decrease in suicides, and contrary to expectations, the number of suicides did not increase when human mobility decreased. Rather, this study demonstrated, for the first time, that suicides increased during the months of increased human mobility during the COVID-19 pandemic in Japan.
One possible reason for the above results is that a decrease in human mobility related to restricted measures might lead to depression and bipolar disorder (Chakrabarti et al., 2021; Devaraj and Patel, 2021; Gimbrone et al., 2021; Tanaka and Okamoto, 2021) and an increase in suicides. Past research has highlighted the impact of the COVID-19 pandemic on major depression, schizophrenia, and bipolar disorder and pointed out the need for patient-specific interventions (Fornaro et al., 2021). A decline in mobility may also lead to a decline in people's well-being (Chakrabarti et al., 2021). Along with the direct impact of reduced human mobility, the change in mobility during the COVID-19 pandemic can be interpreted as the output of the impact of various anti-COVID-19 measures on people's behavior, for example, economic impact, frenzies and anxiety associated with the unknown nature of the new virus. In other words, the impact of COVID-19, which cannot be measured (Carpio-Arias et al., 2022), is captured and evaluated by an index of mobility that includes both outside-prefecture and inside-prefecture mobility. However, the impact might not occur immediately, as seen in the delayed effects of unemployment (Nordt et al., 2015). Our results show that the effect of the unemployment rate in the previous month was greater than the effect of the current unemployment rate, possibly reflecting such a situation.
Several studies have stated that suicides decreased when restrictive measures were taken (Duarte and Jiménez-Molina, 2022). For example, the main protective factors against suicide include, related to mobility, family support and bonding with significant others (O'Connor and Nock, 2014), and quarantine conditions increased time spent with others, strengthening family relationships (Evans et al., 2020). The number of suicides occurring at home was the highest in Japan for both genders before the pandemic (Ministry of Health, Labour and Welfare, 2021). When people become less mobile, there is a possibility that family time increases, and it becomes difficult to carry out suicide at home (Perez et al., 2022). It is important to note that when there is a decrease in human mobility, the number of suicides is relatively low compared to a steady state of human mobility. Throughout the pandemic, suicides have been increasing; therefore, we should consider that the number of suicides increases when human mobility is steady and/or increased.
In our results, increased human mobility in the previous month was associated with a larger ratio of suicides relative to the reference period; however, the increase in mobility during the pandemic was relative to a prior decrease in mobility. A previous study has shown that suicides increase when social activities resume after a disaster that could affect socioeconomics (Kõlves et al., 2013; Orui et al., 2015); the results of our study might imply that similar phenomena occur after movement is resumed. In the context of a disaster, family support can act as a buffer against the worst effects (Tang et al., 2010). Thus, understanding the changes and characteristics of help-seeking behavior during the COVID-19 pandemic may be useful for suicide prevention once social restrictions have been relaxed (Czyz et al., 2013).
In addition, returning to the original environment from an altered environment (e.g., resuming commute to office, increasing interaction with others), such as after holidays (Beauchamp et al., 2014; Plöderl, 2021), may also be related to an increase in stress (Suzuki et al., 2021). Thus, the pressure to resume one's activities on people burdened by the pandemic may increase when restrictions are relaxed from a restriction in mobility or a change in one's living environment. Notably, we observed that there was only a small difference in the increase in the number of suicides when human mobility increased compared with when mobility was stable. The stable month might be interpreted as predicting the recovery of social activities. This might cause the IRR for increased human mobility to be similar to 1.0 for stable human mobility.
As the above, changes in human mobility and changes in suicide during the COVID-19 period showed positive correlations. However, the suicide rate during the pandemic was higher than that in 2019 (Nomura et al., 2021; Tanaka and Okamoto, 2021), when human mobility during the COVID-19 pandemic had been significantly suppressed. Thus, our results do not argue against returning to the mobility levels of 2019. However, a rapid increase in human mobility or a change in the environment may be associated with a larger increase in suicide rates, compared to a moderate increase in human mobility. These relationships will need to be carefully monitored.
It is certain that isolating the cause of suicide is necessary for preventing it. Timely access to emotional support is a well-known way to prevent suicide (World Health Organization, 2014). Although this study did not clarify the causes of suicide, the findings might help practitioners and families consider the timing of intervention (Plöderl, 2021). Furthermore, future research might be able to identify additional triggers for those feeling the burden of the pandemic when human mobility and social activities change. Research investigating the impact of decreased or increased social activity by occupation, as well as by the factors influencing suicide for those who feel the heaviest burden during the pandemic might provide important information.
This study assessed the relationship between restricting human mobility and changes in the number of suicides under the COVID-19 pandemic using available human mobility and suicide data with reference to the year 2019 as control, considering monthly variations and prefecture-by-prefecture differences in suicide. As mentioned earlier, changes in human mobility can be captured by the reaction of society to restrictive measures, and the results in this study can be interpreted as an impact of the change in social conditions on the number of suicides. Since the number of suicides in 2019 does not differ significantly from other years (Supplemental Fig. 1), the bias in analyzing the 2019 value as control year is not considered significant.
Several limitations of our study need to be mentioned. First, we considered only monthly data; it may also be important to examine the effects of reduced human mobility on suicide rates in more detail using daily or weekly data. Second, we evaluated human mobility based on the assumption that if movements in and out of the prefecture increased, then movement from the home had increased. However, we only evaluated movements in and out of the prefecture, and not whether people stayed in their homes. In the future, more detailed movement data could be captured within sub-regions. Third, biases in the estimates of human mobility at the population level may occur due to differences in cellphone ownership and other factors, which may affect the interpretation of the results (Wesolowski et al., 2013). As we focused on long-term changes in human mobility by prefecture, we may have been able to reduce such biases. Human mobility is an indicator that includes the impact of restrictive measures to prevent infection. Therefore, in the present analysis, it was difficult to isolate whether the effect was a direct effect of changes in mobility or correlated with the effects of other variables. Further studies may be needed to evaluate the causal relationship between these variables. Fourth, the current COVID-19 situation may change based on the continual spread of the new Omicron strain (Karim and Karim, 2021). Thus, in the future, it may be important to evaluate whether the number of suicides will return to the pre-pandemic downward trend, using a model of excess mortality (Anzai et al., 2021).
Data sharing
The datasets generated and/or analyzed during the study are available on the website of the Ministry of Health, Labour and Welfare of Japan: https://www.mhlw.go.jp/stf/seisakunitsuite/bunya/0000140901.html, Cabinet Office, and the Geospatial Information Authority of Japan: https://v-resas.go.jp and https://www.geospatial.jp
Patient consent and ethical approval
We only used publicly available aggregate data; a formal ethical review was not required for our study.
CRediT authorship contribution statement
Tatsuhiko Anzai: Methodology, Formal analysis, Writing – original draft. Kohtaro Kikuchi: Formal analysis, Writing – original draft. Keisuke Fukui: Methodology, Writing – review & editing. Yuri Ito: Conceptualization, Writing – review & editing. Kunihiko Takahashi: Conceptualization, Methodology, Writing – review & editing, Supervision.
Declaration of Competing Interest
None declared.
Funding
This work was partially supported by a JSPS KAKENHI Grant Number 21H03402.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.psychres.2022.114898.
Appendix. Supplementary materials
References
- AGOOP Corp., 2021. V-RESAS . URL https://v-resas.go.jp (accessed 12.10.21).
- Anzai A., Nishiura H. Go To Travel” Campaign and travel-associated coronavirus disease 2019 cases: a descriptive analysis, July–August 2020. J. Clin. Med. 2021;10:1–8. doi: 10.3390/jcm10030398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anzai T., Fukui K., Ito T., Ito Y., Takahashi K. Excess mortality from suicide during the early covid-19 pandemic period in Japan: a time-series modeling before the pandemic. J. Epidemiol. 2021;31:152–156. doi: 10.2188/jea.JE20200443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beauchamp G.A., Ho M.L., Yin S. Variation in suicide occurrence by day and during major American holidays. J. Emerg. Med. 2014;46:776–781. doi: 10.1016/j.jemermed.2013.09.023. [DOI] [PubMed] [Google Scholar]
- Carpio-Arias T.V., Piedra-Andrade J.S., Nicolalde-Cifuentes T.M., Padilla-Samaniego M.V., Tapia-Veloz E.C., Vinueza-Veloz M.F. Mobility restrictions and mental health among young adults during the COVID-19 pandemic in Ecuador. Gac. Sanit. 2022 doi: 10.1016/j.gaceta.2021.12.008. S0213-9111(22)00025–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chakrabarti S., Hamlet L.C., Kaminsky J., Subramanian S.V. Association of human mobility restrictions and race/ethnicity–based, sex-based, and income-based factors with inequities in well-being during the COVID-19 pandemic in the United States. JAMA Netw. Open. 2021;4 doi: 10.1001/jamanetworkopen.2021.7373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cirrincione L., Plescia F., Ledda C., Rapisarda V., Martorana D., Lacca G., Argo A., Zerbo S., Vitale E., Vinnikov D., Cannizzaro E. COVID-19 pandemic: new prevention and protection measures. Sustainability. 2022;14:4766. [Google Scholar]
- Czyz E.K., Horwitz A.G., Eisenberg D., Kramer A., King C.A. Self-reported barriers to professional help seeking among college students at elevated risk for suicide. J. Am. Coll. Health. 2013;61:398–406. doi: 10.1080/07448481.2013.820731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Devaraj S., Patel P.C. Change in psychological distress in response to changes in reduced mobility during the early 2020 COVID-19 pandemic: evidence of modest effects from the U.S. Soc. Sci. Med. 2021;270 doi: 10.1016/j.socscimed.2020.113615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duarte F., Jiménez-Molina Á. Suicide and quarantine during the COVID-19 pandemic: do we know everything? Soc. Sci. Med. 2022;309 doi: 10.1016/j.socscimed.2022.115253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans S., Mikocka-Walus A., Klas A., Olive L., Sciberras E., Karantzas G., Westrupp E.M. From “It Has Stopped Our Lives” to “Spending More Time Together Has Strengthened Bonds”: the varied experiences of Australian families during COVID-19. Front. Psychol. 2020:11. doi: 10.3389/fpsyg.2020.588667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fornaro M., De Prisco M., Billeci M., Ermini E., Young A.H., Lafer B., Soares J.C., Vieta E., Quevedo J., de Bartolomeis A., Sim K., Yatham L.N., Bauer M., Stein D.J., Solmi M., Berk M., Carvalho A.F. Implications of the COVID-19 pandemic for people with bipolar disorders: a scoping review. J. Affect. Disord. 2021;295:740–751. doi: 10.1016/j.jad.2021.08.091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fushimi M. Student mental health consultations at a Japanese university and the current state of affairs on the increase in suicide victims in Japan during the COVID-19 pandemic. Psychol. Med. 2021:1–2. doi: 10.1017/S0033291721001240. [DOI] [PubMed] [Google Scholar]
- Geospatial Information Center. 2021. National Human Flow Open Data. URL https://www.geospatial.jp/gp_front/ (accessed 12.10.21).
- Gimbrone C., Rutherford C., Kandula S., Martínez-Alés G., Shaman J., Olfson M., Gould M.S., Pei S., Galanti M., Keyes K.M. Associations between COVID-19 mobility restrictions and economic, mental health, and suicide-related concerns in the US using cellular phone GPS and Google search volume data. PLoS ONE. 2021;16 doi: 10.1371/journal.pone.0260931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gunnell D., Appleby L., Arensman E., Hawton K., John A., Kapur N., Khan M., Connor R.C.O., Pirkis J., COVID-19 Suicide Prevention Research Collaboration Suicide risk and prevention during the COVID-19 pandemic. Lancet Psychiatry. 2020;7:468–470. doi: 10.1016/S2215-0366(20)30171-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karako K., Song P., Chen Y., Tang W., Kokudo N. Overview of the characteristics of and responses to the three waves of COVID-19 in Japan during 2020-2021. Biosci. Trends. 2021;15:1–8. doi: 10.5582/bst.2021.01019. [DOI] [PubMed] [Google Scholar]
- Karim S.S.A., Karim Q.A. Omicron SARS-CoV-2 variant: a new chapter in the COVID-19 pandemic. Lancet Lond. Engl. 2021;6736:19–21. doi: 10.1016/S0140-6736(21)02758-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kikuchi K., Anzai T., Takahashi K. The unusual increase in suicides among women in Japan during the COVID-19 pandemic: a time-series analysis until October 2021. J. Epidemiol. 2022 doi: 10.2188/jea.JE20220186. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kõlves K., Kõlves K.E., De Leo D. Natural disasters and suicidal behaviours: a systematic literature review. J. Affect. Disord. 2013;146:1–14. doi: 10.1016/j.jad.2012.07.037. [DOI] [PubMed] [Google Scholar]
- Kruppa J., Hothorn L. A comparison study on modeling of clustered and overdispersed count data for multiple comparisons. J. Appl. Stat. 2021;48:3220–3232. doi: 10.1080/02664763.2020.1788518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu L., Capaldi C.A., Dopko R.L. Suicide ideation in Canada during the COVID-19 pandemic. Health Promot. Chronic Dis. Prev. Can. Res. Policy Pract. 2021;41:378–391. doi: 10.24095/hpcdp.41.11.06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGinty E.E., Presskreischer R., Han H., Barry C.L. Psychological distress and loneliness reported by US adults in 2018 and April 2020. JAMA - J. Am. Med. Assoc. 2020;324:93–94. doi: 10.1001/jama.2020.9740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ministry of Health Labour and Welfare . NIKKEI PRINTING INC; Tokyo: 2021. 2020 White Paper On Suicide Prevention in Japan. [Google Scholar]
- Ministry of Health Labour and Welfare, 2022. Outbreaks in Japan. URL https://www.mhlw.go.jp/stf/covid-19/kokunainohasseijoukyou.html. (accessed 12.10.21).
- Murayama H., Okubo R., Tabuchi T. Increase in social isolation during the covid-19 pandemic and its association with mental health: findings from the jacsis 2020 study. Int. J. Environ. Res. Public. Health. 2021;18 doi: 10.3390/ijerph18168238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagata S., Nakaya T., Adachi Y., Inamori T., Nakamura K., Arima D., Nishiura H. Mobility change and covid-19 in japan: mobile data analysis of locations of infection. J. Epidemiol. 2021;31:387–391. doi: 10.2188/jea.JE20200625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nomura S., Kawashima T., Yoneoka D., Tanoue Y., Eguchi A., Gilmour S., Kawamura Y., Harada N., Hashizume M. Trends in suicide in Japan by gender during the COVID-19 pandemic, up to September 2020. Psychiatry Res. 2021;295 doi: 10.1016/j.psychres.2020.113622. [DOI] [PubMed] [Google Scholar]
- Nordt C., Warnke I., Seifritz E., Kawohl W. Modelling suicide and unemployment: a longitudinal analysis covering 63 countries, 2000-11. Lancet Psychiatry. 2015;2:239–245. doi: 10.1016/S2215-0366(14)00118-7. [DOI] [PubMed] [Google Scholar]
- O'Connor R.C., Nock M.K. The psychology of suicidal behaviour. Lancet Psychiatry. 2014;1:73–85. doi: 10.1016/S2215-0366(14)70222-6. [DOI] [PubMed] [Google Scholar]
- Orui M., Sato Y., Tazaki K., Kawamura I., Harada S., Hayashi M. Delayed increase in male suicide rates in tsunami disaster-stricken areas following the Great East Japan Earthquake: a Three-year follow-up study in miyagi prefecture. Tohoku J. Exp. Med. 2015;235:215–222. doi: 10.1620/tjem.235.215. [DOI] [PubMed] [Google Scholar]
- Perez V., Elices M., Vilagut G., Vieta E., Blanch J., Laborda-Serrano E., Prat B., Colom F., Palao D., Alonso J. Suicide-related thoughts and behavior and suicide death trends during the COVID-19 in the general population of Catalonia, Spain. Eur. Neuropsychopharmacol. 2022;56:4–12. doi: 10.1016/j.euroneuro.2021.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pirkis J., Gunnell D., Shin S., Del Pozo-Banos M., Arya V., Aguilar P.A., Appleby L., Arafat S.M.Y., Arensman E., Ayuso-Mateos J.L., Balhara Y.P.S., Bantjes J., Baran A., Behera C., Bertolote J., Borges G., Bray M., Brečić P., Caine E., Calati R., Carli V., Castelpietra G., Chan L.F., Chang S.-S., Colchester D., Coss-Guzmán M., Crompton D., Ćurković M., Dandona R., Jaegere E.D., Leo D.D., Deisenhammer E.A., Dwyer J., Erlangsen A., Faust J.S., Fornaro M., Fortune S., Garrett A., Gentile G., Gerstner R., Gilissen R., Gould M., Gupta S.K., Hawton K., Holz F., Kamenshchikov I., Kapur N., Kasal A., Khan M., Kirtley O.J., Knipe D., Kõlves K., Kölzer S.C., Krivda H., Leske S., Madeddu F., Marshall A., Memon A., Mittendorfer-Rutz E., Nestadt P., Neznanov N., Niederkrotenthaler T., Nielsen E., Nordentoft M., Oberlerchner H., O'Connor R.C., Papsdorf R., Partonen T., Phillips M.R., Platt S., Portzky G., Psota G., Qin P., Radeloff D., Reif A., Reif-Leonhard C., Rezaeian M., Román-Vázquez N., Roskar S., Rozanov V., Sara G., Scavacini K., Schneider B., Semenova N., Sinyor M., Tambuzzi S., Townsend E., Ueda M., Wasserman D., Webb R.T., Winkler P., Yip P.S.F., Zalsman G., Zoja R., John A., Spittal M.J. Suicide numbers during the first 9-15 months of the COVID-19 pandemic compared with pre-existing trends: an interrupted time series analysis in 33 countries. eClinicalMedicine. 2022;51 doi: 10.1016/j.eclinm.2022.101573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pirkis J., John A., Shin S., DelPozo-Banos M., Arya V., Analuisa-Aguilar P., Appleby L., Arensman E., Bantjes J., Baran A., Bertolote J.M., Borges G., Brečić P., Caine E., Castelpietra G., Chang S.S., Colchester D., Crompton D., Curkovic M., Deisenhammer E.A., Du C., Dwyer J., Erlangsen A., Faust J.S., Fortune S., Garrett A., George D., Gerstner R., Gilissen R., Gould M., Hawton K., Kanter J., Kapur N., Khan M., Kirtley O.J., Knipe D., Kolves K., Leske S., Marahatta K., Mittendorfer-Rutz E., Neznanov N., Niederkrotenthaler T., Nielsen E., Nordentoft M., Oberlerchner H., O’Connor R.C., Pearson M., Phillips M.R., Platt S., Plener P.L., Psota G., Qin P., Radeloff D., Rados C., Reif A., Reif-Leonhard C., Rozanov V., Schlang C., Schneider B., Semenova N., Sinyor M., Townsend E., Ueda M., Vijayakumar L., Webb R.T., Weerasinghe M., Zalsman G., Gunnell D., Spittal M.J. Suicide trends in the early months of the COVID-19 pandemic: an interrupted time-series analysis of preliminary data from 21 countries. Lancet Psychiatry. 2021;8:579–588. doi: 10.1016/S2215-0366(21)00091-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plöderl M. Suicide risk over the course of the day, week, and life. Psychiatr. Danub. 2021;33:438–445. doi: 10.24869/psyd.2021.438. [DOI] [PubMed] [Google Scholar]
- R Core Team, 2021. R: A language and Environment For Statistical computing. R Foundation For Statistical Computing, Vienna, Austria.
- Suzuki K., Takeshima T., Igarashi H., Imai N., Danno D., Yamamoto T., Nagata E., Haruyama Y., Mitsufuji T., Suzuki S., Ito Y., Shibata M., Kowa H., Kikui S., Shiina T., Okamura M., Tatsumoto M., Hirata K. Impact of the COVID-19 pandemic on migraine in Japan: a multicentre cross-sectional study. J. Headache Pain. 2021;22:1–10. doi: 10.1186/s10194-021-01263-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanaka T., Okamoto S. Increase in suicide following an initial decline during the COVID-19 pandemic in Japan. Nat. Hum. Behav. 2021;5:229–238. doi: 10.1038/s41562-020-01042-z. [DOI] [PubMed] [Google Scholar]
- Tang T.C., Yen C.F., Cheng C.P., Yang P., Chen C.S., Yang R.C., Huang M.S., Jong Y.J., Yu H.S. Suicide risk and its correlate in adolescents who experienced typhoon-induced mudslides: a structural equation model. Depress. Anxiety. 2010;27:1143–1148. doi: 10.1002/da.20748. [DOI] [PubMed] [Google Scholar]
- Ueda M., Nordström R., Matsubayashi T. Suicide and mental health during the COVID-19 pandemic in Japan. J. Public Health. 2021;44(3):541–548. doi: 10.1093/pubmed/fdab113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wesolowski A., Eagle N., Noor A.M., Snow R.W., Buckee C.O. The impact of biases in mobile phone ownership on estimates of human mobility. J. R. Soc. Interface. 2013;10 doi: 10.1098/rsif.2012.0986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization, 2014. Preventing Suicide: A Global Imperative. WHO Press, Geneva.
- Zhang M., Wang S., Hu T., Fu X., Wang X., Hu Y., Halloran B., Li Z., Cui Y., Liu H., Liu Z., Bao S. Human mobility and COVID-19 transmission: a systematic review and future directions. Ann. GIS. 2022;0:1–14. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.