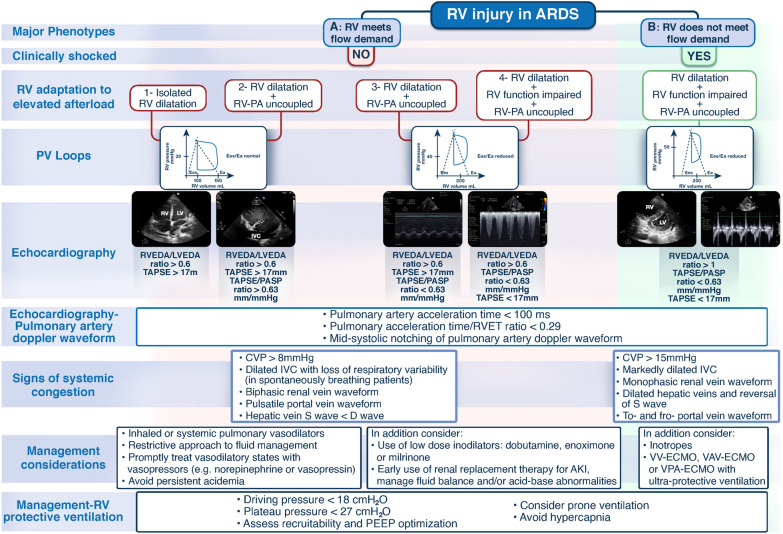
Fig. 1.
Proposed theoretical RV injury major phenotypes based on RV biomechanics as assessed by clinical examination, RV P–V relationship at different loading conditions, and echocardiography. It should be noted that the different methods and combination of parameters proposed to differentiate the different phenotypes and management strategies need to be validated in prospective studies since this is not a ‘standard’ time sequence regularly encountered on clinical grounds; in practice, the hemodynamic assessment is often performed at various timepoints in the RV injury course. The RV P–V loops show the RV pressure–volume relation at different loading conditions wherein the RV may or may not meet flow demand. Assessment of systemic venous congestion using central venous pressure and right-sided venous flow patterns in hepatic, portal and intra-renal veins, and IVC may also be part of RV injury severity evaluation (morphology of S and D venous Doppler waveforms, during RV contraction and relaxation respectively, for hepatic and intra-renal veins; pulsatility or interruption of flow giving a to-and-fro appearance, for portal vein; and size and respirophasic variation, for IVC). AKI acute kidney injury, ARDS acute respiratory distress syndrome, CVP central venous pressure, COVID-19 coronavirus disease-19, Ea pulmonary arterial elastance, ECMO extracorporeal membrane oxygenation, Ees right ventricular end-systolic elastance, IVC inferior vena cava, LV left ventricle, LVEDA left ventricular end-diastolic area, PV loops pressure–volume loops, PA pulmonary artery, PASP pulmonary artery systolic pressure, PEEP positive end-expiratory pressure, RV right ventricle, RVEDA right ventricular end-diastolic area, RVET right ventricle ejection time, TAPSE tricuspid annular plane systolic excursion, VAV-ECMO veno-arterio-venous extracorporeal membrane oxygenation, VPA- ECMO veno-pulmonary arterial extracorporeal membrane oxygenation, VV-ECMO veno-venous extracorporeal membrane oxygenation