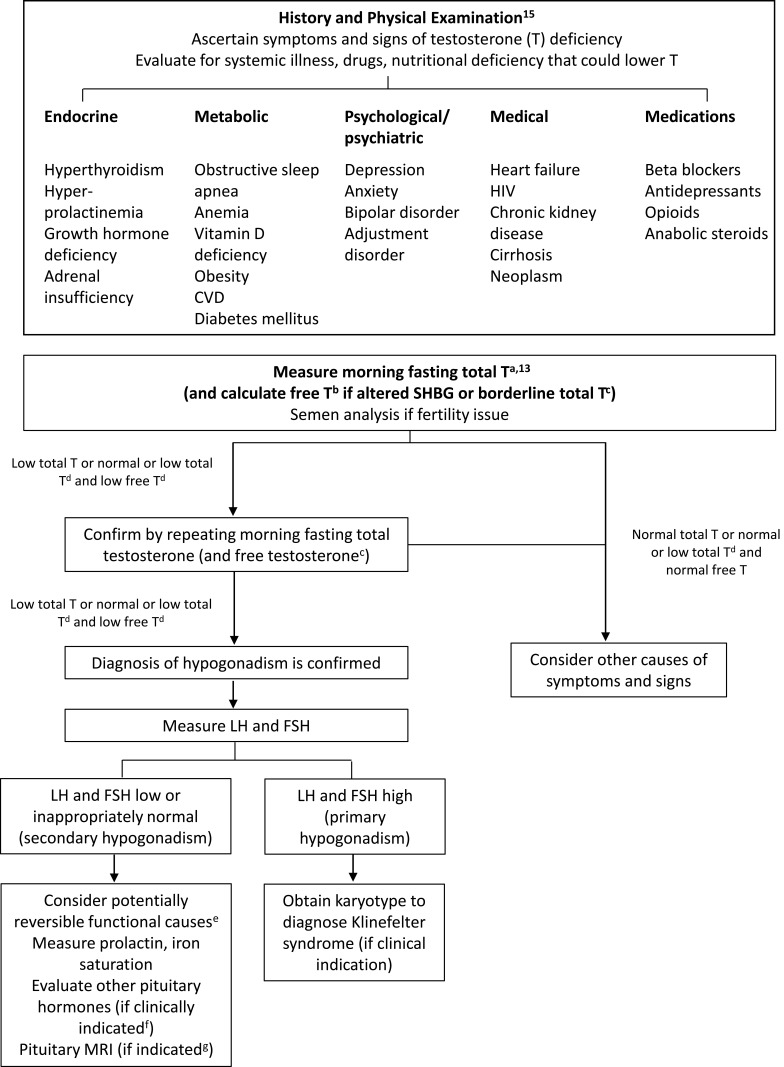
Figure 1.
Evaluation and diagnosis of testosterone deficiency.
Notes: aThe lower limit of the normal TT harmonized to the CDC standard in healthy, nonobese young men is 264 ng/dL (9.2 nmol/L); this limit could be used for TT assays that are CDC certified. For laboratories that are not CDC certified and do not participate in an accuracy-based quality control program, the reference range may vary considerably depending on the assay and reference population used. Using the lower limit of the range established in local laboratories may not accurately identify men with hypogonadism. bFT should be measured by an equilibrium dialysis method or estimated from total testosterone, SHBG, and albumin using a formula that accurately reflects FT by equilibrium dialysis. A harmonized reference range for FT has not been established, so reference ranges may vary considerably depending on the specific equilibrium dialysis method or the algorithm used to calculate FT. Therefore, until a harmonized reference range is established, the lower limits established by the laboratory may be used. cConditions in which measurement of FT concentration is recommended are listed in Table 1. Conditions that alter SHBG levels include obesity, diabetes mellitus, use of glucocorticoids, some progestins and androgenic steroids, nephrotic syndrome, acromegaly, aging, HIV, cirrhosis and hepatitis, hypo- or hyperthyroidism, use of some anticonvulsants, estrogen use, and polymorphisms in the SHBG gene. dTT may also be high in some conditions in which SHBG levels are high, such as HIV or use of some anticonvulsants. ePotentially reversible functional causes of secondary hypogonadism include hyperthyroidism, hyperprolactinemia, growth hormone deficiency, adrenal insufficiency, obstructive sleep apnea, anemia, vitamin D deficiency, obesity, CVD, diabetes mellitus, depression, anxiety, bipolar disorder, adjustment disorder, heart failure, HIV, chronic kidney disease, cirrhosis, neoplasm, and use of beta blockers, antidepressants, opioids, and anabolic steroids. fIf there is clinical indication of hypopituitarism or sella abnormality on imaging, evaluation of other pituitary hormones (eg, free thyroxine, morning cortisol, and adrenocorticotropic hormone stimulation test if clinical hypocortisolism is suspected) should be performed. gPerform pituitary imaging (MRI) to exclude pituitary and/or hypothalamic tumor or infiltrative disease when severe secondary hypogonadism (eg, serum T <150 ng/dL [5.2 nmol/L]), panhypopituitarism, persistent hyperprolactinemia, or symptoms or signs of tumor mass effect (such as new-onset headache, visual impairment, or visual field defect) are present. CT scan may be sufficient if macroadenoma is suspected or to assess parasellar bone involvement. Bhasin S, Brito JP, Cunningham GR, et al. Testosterone therapy in men with hypogonadism: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2018;103(5):1715–1744, doi:10.1210/jc.2018-00229. Adapted by permission of Oxford University Press on behalf of the Endocrine Society.13
Abbreviations: CDC, Centers for Disease Control and Prevention; CT, computed tomography; CVD, cardiovascular disease, FSH, follicle-stimulating hormone; FT, free testosterone; LH, luteinizing hormone; MRI, magnetic resonance imaging; SHBG, sex hormone−binding globulin; TT, total testosterone.