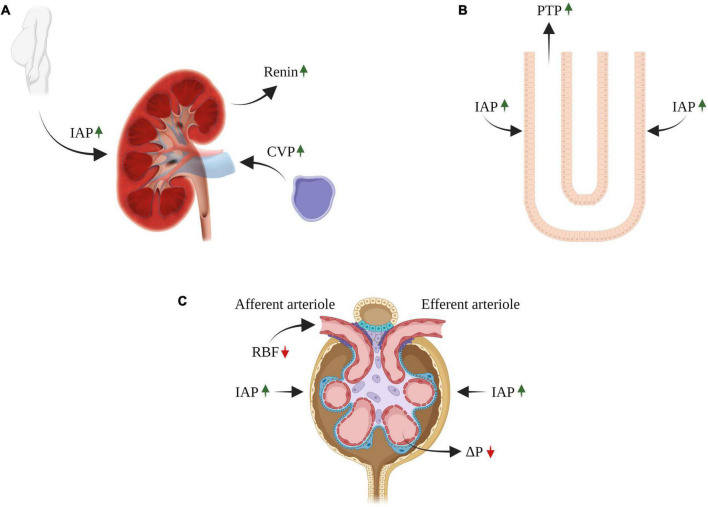
FIGURE 2.
Impact of congestive venous pressure (CVP) and increased intra-abdominal pressure (IAP) on kidney function in heart failure. Elevated CVP is transmitted back to the renal veins leading to renal dysfunction (A). The contribution of renal venous congestion to renal dysfunction in HF is complex and involves multiple mechanisms, including increased pressure along the renal vasculature without decline in ΔP, decreasing the net pressure gradient filtration pressure (NFP) across the glomerulus and thereby reduced GFR (C). In addition, the increase in renal venous pressure can increase intrarenal interstitial pressure leading to compression of the tubules, increased tubular fluid pressure (B), with reduced GFR due to an increase in hydrostatic pressure in the Bowman’s capsule (C). In addition, reduced GFR and sodium excretion may develop secondary to intra-abdominal hypertension (IAH), a hallmark feature of decompensated CHF (A–C). The diverse deleterious renal effects of elevated IAP may overlap with those of venous congestion. There is a direct compression of abdominal contents that result in a prominent reduction in RBF (compression of renal arteries) and elevation in renal parenchymal and renal vein pressures (A–C). RBF, renal blood flow; GFR, glomerular filtration rate; CVP, central venous pressure; IAP, intraabdominal pressure; PTP, proximal tubular pressure. ΔP, hydrostatic pressure gradient.