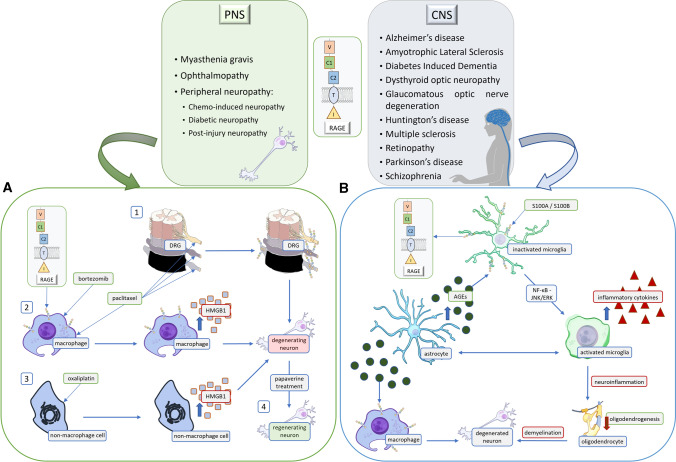
Fig. 4.
RAGE-activation-dependent signaling is present in numerous disorders of the nervous system. The diseases noted in the text are divided into two tables based on the location of the pathological changes. The RAGE ligands listed are assigned to specific conditions. Pro-inflammatory RAGE ligands such as S100A, S100B, and HMGB1 participate in the development of disease by binding to RAGE. Although in some circumstances, low and slightly raised levels of a given molecule may have a neuroprotective, pro-regenerative effect on the neuronal system, excessive levels lead to pathological pathway activation. A Chemo-induced neuropathy is an exemplary peripheral nervous system (PNS) disease. The figure presents multiple mechanisms that lead to neurodegeneration. Paclitaxel is an anti-cancer drug that causes an increased expression of RAGE in the DRG (1). At the same time, it increases the expression of HMGB1 in macrophages (2). Oxaliplatin has a similar effect on non-macrophage cells (3), as it increases the production of HMGB1. Interestingly, recent research provides data suggesting that papaverine treatment increases neuronal recovery, which helps in alleviating neuropathic pain (4). B Multiple sclerosis is an exemplary CNS neurodegenerative disease. Microglial RAGE binds to S100A8/A9, activating NF-κB via JNK/ERK pathway, which then increases the production of inflammatory cytokines. Moreover, due to metabolic changes, astrocytes produce excessive AGEs, which also bind to RAGE on microglia and macrophages within the lesion. Subsequently, this leads to demyelination along with inflammation, to further neurodegeneration and health decline.