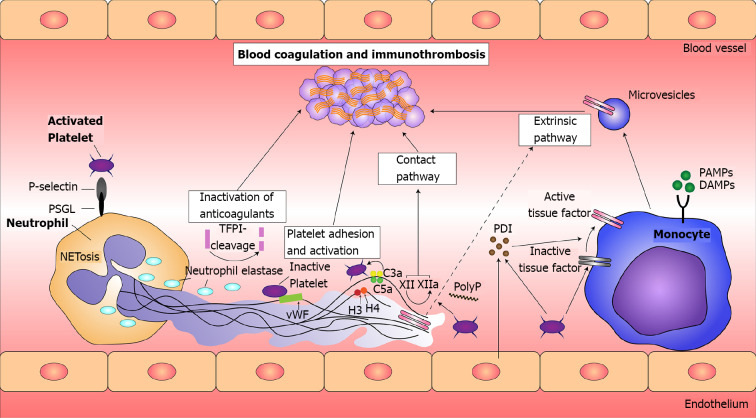
Figure 3.
Principles of immunothrombosis. Monocytes and their microvesicles release activated intravascular tissue factor (TF) in response to pathogen-associated molecular patterns (PAMPs) or damage-associated molecular patterns (DAMPs), which initiates the extrinsic pathway of coagulation. Activated platelets and endothelium secrete protein disulfide isomerase (PDI), which activates microvesicle-derived TF. Interaction between P-selectin on activated platelets and P-selectin glycoprotein ligand (PSGL) on leukocytes enhance recruitment of leukocytes and increase TF production. Neutrophil extracellular traps (NETs) provide a scaffold consisting of DNA, histones, and neutrophil serine proteases, and they support immunothrombosis through several pathways. (1) NETs bind to von Willebrand factor (vWF) and support the recruitment of platelets; (2) Histones H3 and H4 on NETs can trigger the activation of platelets; (3) NETs bind to TF leading to TF-mediated thrombingeneration through the extrinsic pathway (dotted arrow); (4) Neutrophil elastase and other neutrophil serine proteases cleave and inactivate anticoagulants, including TF pathway inhibitor and thrombomodulin; and (5) NETs can directly activate factor XII (the contact pathway of coagulation) mediated by platelet-derived polyphosphates (PolyP). The complement system (specifically the activated complement components C3a and C5a) also enhances platelet activation. TFPI: Tissue factor pathway inhibitor. Citation: Jayarangaiah A, Kariyanna PT, Chen X, Jayarangaiah A, Kumar A. COVID-19-Associated Coagulopathy: An Exacerbated Immunothrombosis Response. Clin Appl Thromb Hemost 2020; 26: 1076029620943293. Copyright ©The Author(s) 2020. Published by SAGE.