Abstract
Training healthcare professionals with Design Thinking (DT) can support patient-centred care by recognizing patient/care provider needs through empathizing. This article explored the Design Thinking in improving clinical researchers’ understanding of relatively unexplored and understudied dementia caregiving problems. Following the Double-Diamond, a Design Thinking process model, we conducted a series of workshops and invited family caregivers of patients with dementia as active participants to provide training to clinical researchers on Design Thinking. We then evaluated the benefit of the workshops in improving clinical researchers’ understanding of the caregiving problem and solution space through pre- and post-surveys. Our findings revealed researchers’ overall perception of Design Thinking, their clear insights on dementia caregivers’ challenges, and speculating caregiver-specific interventions. Our paper contributed to the health design community by exploring the benefit of Design Thinking in understudied areas by 1) Recognizing urgent matters in healthcare, 2) Revealing implicit needs through collective expertise and knowledge exchange, and 3) Producing original health care research and contributions. We hope this study inspires and supports training healthcare researchers to advance dementia caregiving and healthcare research initiatives by adopting the Double-Diamond process model.
Keywords: Design Thinking, Health Education, Clinical Research, Dementia Caregiving, Problem Solving, Patient-Centred Intervention
Introduction
Design Thinking (DT) is a human-centred process that prioritizes articulating the right problem by empathizing with people and proposing innovative solutions that meet people’s needs and capabilities (Norman 2013). Empathizing with people can uncover explicit but also implicit human behaviour and associated needs, including emotions and frustrations that are usually not stated directly. The DT process is dependent upon the emergence and diversity of thoughts/inputs gathered from people associated directly or indirectly with a problem at hand. Such an approach is conducive to innovative outcomes supported by co-evolution of problem definition and solution space. Innovation emerges after cycling through several iterative and nonlinear stages that incorporate divergent and convergent thinking. Divergent thinking is used to generate novel ideas/solutions to or create choices for a problem by exploring multiple possible directions; convergent thinking seeks to make choices or define a single well-established solution (Ferreira et al. 2015). The iterative nature of the process encourages designers to ‘move rapidly to early solution conjectures and use these conjectures as a way of exploring and defining problems and solutions together’ (Cross 2001). The process enables design thinkers to make more deliberate and thoughtful decisions in solving complex problems (Jonas and Stolterman 2004). Also, the flexible nature of the method allows its application in varied health care settings and conditions (Altman et al. 2018).
While DT emerged from the design tradition, it is common to incorporate DT in non-design fields to resolve complex or ‘ill-defined’ problems. Nigel Cross asserted that the ill-defined nature of problems means that ‘they cannot be solved simply by collecting and synthesizing information’ (2017). Due to the increasing number and complexity of problems in healthcare, DT can be deployed to resolve persistent issues by fostering human-centred research and collective and diverse teamwork (Roberts et al. 2016). Clinical researchers may benefit from designers’ approach to problem-solving in exploring care recipients’/providers’ challenges, defining their needs, and proposing meaningful research initiatives to improve health-related situations. While the DT approach is well-recognized in healthcare education and clinical practices (see the background section), it has not been applied in academia or advanced healthcare research. While the reason can be correlated with the practice-oriented nature of DT, we argue that the framework can support the initial stages of advanced research in healthcare. Previous studies in the non-medical field revealed the DT benefit to doctoral students and its contributions to establishing scientific research by extending the boundary of knowledge and balancing the novelty and analytical aspects of the research (Cravens et al. 2014).
This article describes the application of DT in the field of dementia caregiving and explores its potential benefit in training clinical researchers/scholars to undertake caregiving research that supports and enhances caregiver’s sense of self-efficacy and mastery (their felt sense of competence). In order to familiarize researchers with DT, we developed and implemented a series of DT workshops that engaged family caregivers of persons living with dementia. The workshops introduced researchers to DT and demonstrated its application to dementia caregiving through a series of activities that encouraged empathizing with dementia family caregivers to identify hidden problems and explore potential caregiving interventions. We define empathy as ways of behaving to support deep connection and understanding of dementia family caregivers’ challenges. We practiced empathy by demonstrating behaviours such as active listening (e.g., restating their problems) and recognizing/responding appropriately to caregivers’ emotions/thoughts/feelings associated with their dementia caregiving challenges.
Additionally, we used DT as an umbrella term for human-centred approach to problem-solving. We employed the Double Diamond, a DT process model (Ferreira et al. 2015), and embedded principles as a leading framework to conduct DT training workshops. The model directly immersed researchers with caregivers’ challenges through empathy-building and exposed them to divergent/convergent thinking to identify problems/solutions for dementia family caregivers. Through a pre- and post-survey, we evaluated researchers’ human-centredness and problem-solving skills as two critical DT skills. We asked researchers to reflect on the application of DT in their research initiatives in identifying caregivers’ challenges and developing caregiving interventions.
Our study revealed that DT is beneficial and applicable to advanced healthcare research. The rapid-iterative nature of DT allows early exploration of problem spaces to support researchers in identifying novel and unexplored areas of studies in healthcare with no or limited established knowledge of the subject matter (i.e., caregiving for persons with dementia).
Background
Design Thinking in Health Care
In healthcare, DT offers human-centred design methods and practices to confront complex challenges by uncovering previously unconceived options and expanding the domain of actions (Rowe et al. 2020). In their review of DT articles in the context of health, McLaughlin et al. (2019) defined DT as a problem-solving framework used to ‘enhance patient experiences, improve clinical outcomes and refine medical curricula.’ Applying DT to health care enhances innovation, efficiency, and effectiveness of interventions by recognizing patient and care provider needs (Altman et al. 2018). DT has been found to be valuable in healthcare management, innovation and practices by fostering human-centred research, collective and diverse teamwork and rapid prototyping to resolve complex and persistent healthcare problems (Roberts et al. 2016) and to support redesigning healthcare interventions to achieve higher efficiency, effectiveness, and user satisfaction (Luna et al. 2017). Despite the importance of incorporating patients’ and providers’ insights into intervention development processes, these populations are rarely involved, which results in less satisfactory results (Lyon and Koerner 2016; Searl et al. 2010).
DT has been used to resolve complex and persistent problems in varied health care settings and across a diverse range of patient populations to improve the quality of care and patients’ conditions. For example, DT has been employed to develop interventions to support patients in chronic obstructive pulmonary disease self-management (Velardo et al. 2017), to provide diabetes medication education (Henderson et al. 2013), and to enhance physical activities of patients with chronic diseases (van der Weegen et al. 2013). Other studies applied the approach to developing interventions to empower nursing staff in their clinical practices by providing drug-drug interaction alerts (Luna et al. 2017), supporting antimicrobial-related tasks (Wentzel et al. 2016), and enhancing handoff communications (Lin et al. 2015).
Design Thinking in Medical and Health Education
DT can be a powerful tool in training future health professionals (Sandars and Goh 2020) and complementing traditional approaches to help educators ‘clearly and empathetically understand the needs and problems faced by their students or trainees’ (Gottlieb et al. 2017) and to stimulated interdisciplinary collaboration (McLaughlin et al. 2019). DT provides opportunities to develop interdisciplinary collaboration and help participants ‘refine problems and identify the appropriate needs with a human- or user-centred approach’ (McLaughlin et al. 2019). Additionally, DT can optimize learners’ educational experiences through empathetic and inclusive approaches that amplify the voices of patients and clinicians (McLaughlin et al. 2019).
Medical educators applied DT in a variety of learner groups and educational settings, including redesigning radiology residents’ ultrasound experience (Deitte and Omary 2019), resolving complex structural health care issues through interdisciplinary collaboration (Van De Grift and Kroeze 2016), and inspiring innovative public health interventions (Abookire et al. 2020). In Nursing education, DT has been used as a powerful tool for training ‘innovative and empathetic nurses’ to tackle healthcare problems and prioritize patients’ needs (Beaird et al. 2018). An experimental research in DT enabled nursing informatics (NI) students to construct their conceptual papers addressing significant challenges in healthcare (Padagas 2021).
More recently, DT has proved a promising approach in pharmacy education (Wolcott and McLaughlin 2020) and as an accelerated process for developing solution to overcome COVID-19 challenges in various areas of medical education (Thakur et al. 2021). The latter discussed the rapid nature of DT helpful in seeking resolution to rapidly changing situations in healthcare. It has also been proposed as a way for medical educators to initiate inter-institutional collaboration, develop, evaluate, and report on curricula on ‘Innovation, empathy, ethics, the health humanities, interprofessional education, patient centered care, or “wicked problems” in healthcare’ (Madson 2021).
Study Design and Methods
We conducted three DT online workshops in the context of family caregiving for persons with dementia and evaluated the outcome through pre- and post-surveys. We provide detailed information about the participants, context, and DT approach in the following sections.
Participants Configuration
Two to five caregivers from the Integrated Memory Care Clinic (IMCC) at Emory University and 20–24 researchers from different US institutions attended three webinar sessions. The caregivers were family members who have provided extended daily care and assistance to persons living with dementia. The IMCC is a nurse practitioner-led patient-centred medical home that provides dementia-sensitive and comprehensive primary care for persons living with dementia and their caregivers (Clevenger et al. 2018). All caregivers had experience receiving care from IMCC. The researchers had different academic ranks from postdoctoral fellows to full professors, and a variety of healthcare specialties, including geriatric medicine, nursing, neurodegenerative/ Alzheimer’s disease movement disorders, neurology, geriatric dentistry, and academic fields including indigenous aging and psychology. The inclusion criteria for recruiting researchers were their work experience and interest in initiating research in the dementia caregiving context (e.g., caregiver social connectedness, cultural understandings of dementia caregiving).
We recruited family caregivers of individuals with dementia through IMCC. We invited the clinical researchers to participate by sending announcements to National Institutes of Health Roybal Centers, Geriatrics and Gerontology Faculty at Emory University and the Atlanta Veterans Affairs Medical Center, and research interest groups at several other universities (e.g., Rush Alzheimer’s Disease Center; Layton Aging, and Alzheimer’s Disease Center). The researchers reported little or no familiarity with DT and its application in healthcare before attending the workshops.
Design Thinking Workshops
From September to December 2020, we engaged the caregivers and researchers in three 90-minute Design Thinking workshops aimed at developing caregiver mastery interventions (Table 1). In each workshop, we described the particular DT process to be used and then illustrated its application to caregiving by exploring caregivers’ experiences in and thoughts about the IMCC. The IMCC case study allowed us to concentrate on a particular point of care, guide the workshop conversation within the domain of dementia care, and focus the DT process on understanding how to improve primary care for people with dementia and identify interventions that can support patient-clinicians at the point of care. We video-recorded the workshops and summarized each workshop takeaways to facilitate/inform the next session (e.g., challenges shared by caregivers).
Table 1.
DT workshops structures and configurations
| DT Workshops | Workshop 1 (Discover) | Workshop 2 (Define) | Workshop 3 & 4 (Deliver & Develop) | |
|---|---|---|---|---|
|
| ||||
| Topic | DT overview; Empathizing with caregivers | Defining a key caregiving problem | Ideating caregiving interventions | Evaluating caregiving interventions |
| Method | Divergent thinking | Convergent thinking | Divergent thinking | Convergent thinking |
| Participants | 2 caregivers Both females |
2 caregivers Both females |
2 caregivers Both females |
5 caregivers (3 new) 4 females / 1 male |
| 22 researchers 3 males / 19 females |
24 researchers 3 males / 21 females |
20 clinical researchers 4 males / 16 females |
||
| Duration | 90-minute | 90-minute | 90-minute | |
| Outcome | A List of caregiving challenges | A clear problem statement | A list of caregiving intervention concepts | A caregiving intervention concept |
The three DT workshops provided training to the researchers in the early phases of developing research initiatives by demonstrating ways to empathize with caregivers, explore their challenges as they provide care, and speculate about future caregiving interventions to support caregiving mastery. We encouraged researchers to participate in the DT workshop and provide expert opinion/input on caregivers’ challenges when appropriate, particularly in exploring caregiving interventions. Thus, they took the role of observers and active participants during the workshops.
Design Thinking Approach
We adapted Double Diamond, a DT process model initiated by the British Design Council in 2005 (Ferreira et al. 2015). The flexible and straightforward nature of the Double Diamond model allowed its practical implementation in the context of dementia caregiving and online workshops. The process is divided into four phases of Discover, Define, Develop, and Deliver that emphasizes on divergent and convergent modes of thinking (Figure 1). The process engages divergent thinking in exploring a problem/solution space and then employs convergent thinking to find the right problem and develop the right solution. More specifically, the Discover stage corresponds to a deep contextual understanding of the challenges through empathizing with people. This stage uses divergent thinking and inquiry/field research methods (e.g., interviews, observations, and focus groups) to gain insight into people’s explicit/implicit needs, experiences, and motivations. The Define phase identifies core problems using convergent thinking by analysing/synthesizing recurring patterns in contextual data gathered during the empathize stage. Insight cards and affinity diagram methods can be used in this phase to facilitate organizing, clustering, and visualizing complex data. The third phase, or Develop, seeks to generate conceptual ideas and identify novel solutions to the problem statement using divergent thinking methods (e.g., brainstorming, storytelling, and co-creation workshops). Finally, Deliver uses convergent thinking and focuses on adjusting and validating the proposed concepts at a small-scale and rejecting those that are not feasible/promising, using evaluation methods (e.g., surveys, think aloud, and shadowing). Despite the linear illustration of the Double Diamond model, the process is most effective after cycling through the four iterative and non-sequential stages that incorporate divergent and convergent thinking.
Figure 1.
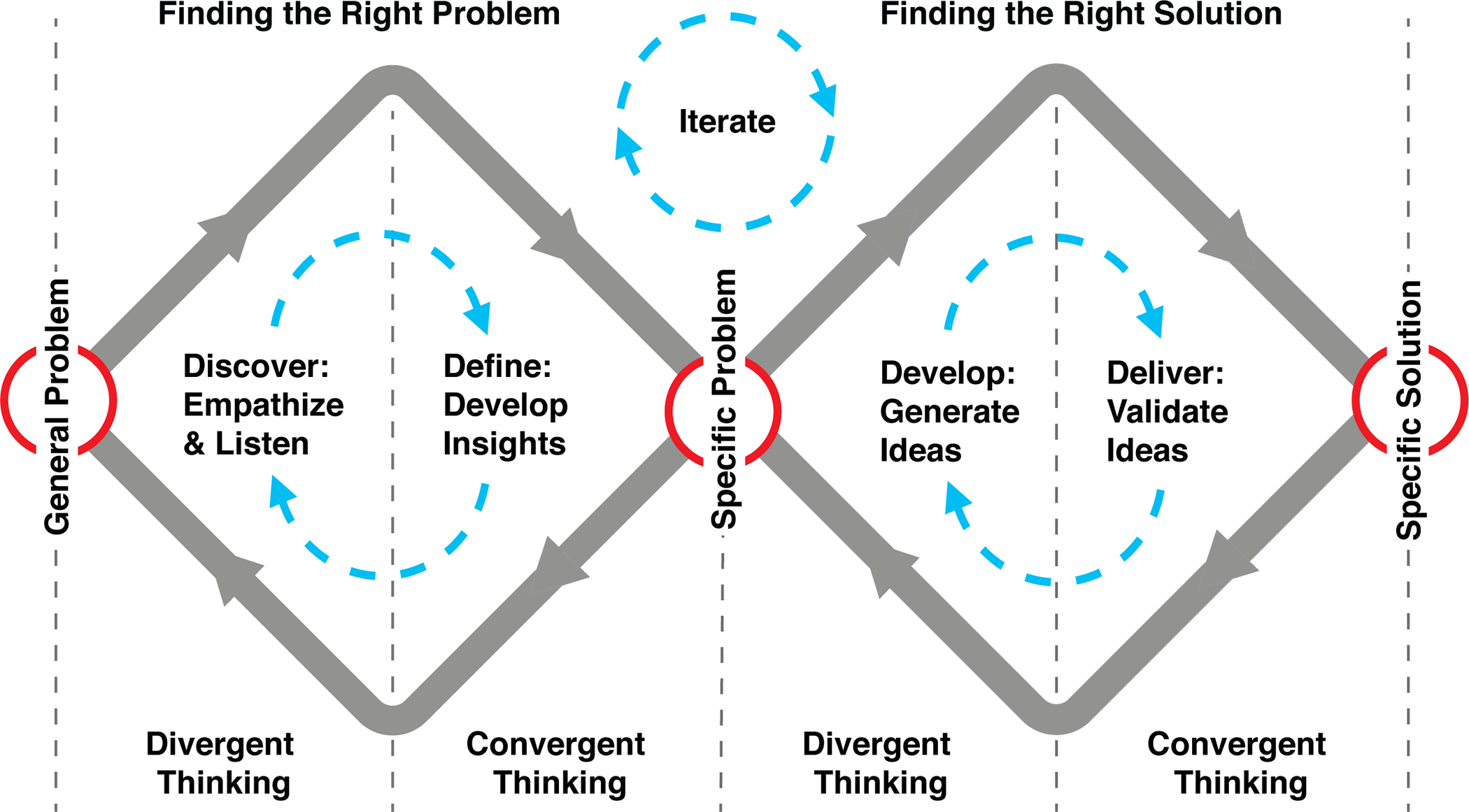
The DT model used in the dementia caregiver interventions study. The adapted version comprises the Double Diamond DT model introduced by the Design Council and the DT model introduced by the D. School.
We followed the four DT steps to provide tangible training to researchers by applying the method in exploring the problem/solution space with caregivers. For all workshops, we prepared slides (with a strong emphasis on visualization) to 1) introduce the concepts (e.g., DT process, divergent/convergent thinking); 2) facilitate the conversations, and 3) provide real-time documentation of the discussions/insightful thoughts.
Workshop 1
In the first workshop, we described the aim of the workshop series, provided an overview of the DT process, and introduced the IMCC program to the researchers. We then initiated the first stage of the DT process (Discover) by a focus group, asking the caregivers to think as broadly as possible about their caregiving challenges and needs not being met by IMCC or elsewhere, using divergent thinking as a means of empathizing with caregivers. We asked broad, open-ended questions including:
What are your primary everyday care challenges?
What do you feel to be your most challenging caregiving task, and how do you handle it?
What has been your experience at the IMCC? What type of support have you received?
What is missing? What are some other ways that the clinic can support you as a caregiver?
The ensuing conversation produced four themes and 13 challenges shared by caregivers (Table 2), including providing care (e.g., keeping a person with dementia safe) and being a caregiver (e.g., resting from caregiving activities). While researchers’ role in this stage was observers of caregivers-facilitators conversations, they occasionally asked questions from caregivers to gain insight on their thinking and better understand the reason behind the proposed issues.
Table 2.
Dementia caregiving challenges developed following divergent thinking.
| Overarching Theme | Caregivers Challenges |
|---|---|
|
| |
| 1.Challenges of providing care/support to patients with dementia | 1. Challenge of keeping persons with dementia safe at home |
| 2. Lack of public education and general awareness about persons’ aggressive behaviours associated with dementia can threaten persons with dementia’s safety | |
| 3. Strong need to have access to 24-hour support line to consult about people with dementia health/behaviour issues and action plans | |
| 4. Lack of having access to universal care that provides comprehensive care | |
| 5. Importance of having access to geriatric oral health and hygiene specialized in dementia care | |
| 2. Challenges of being a caregiver and self-care | 6. Challenges of resting from caregiving continuing activities |
| 7. Need for having access to affordable daycare centers | |
| 8. Need for having a secondary caregiver to help with caregiving tasks when needed | |
| 3. Challenges of having access to critical information | 9. Need for having access to repository and archive of dementia regular information |
| 10. Need for having access to educational programs during the pre-diagnosis | |
| 11. Need for connecting with other dementia caregivers and peer support groups | |
| 4. Challenges of having a social life | 12. Difficulty avoiding conflicts in public due to inappropriate behaviours of persons with dementia |
| 13. Difficulty attending social events/activities outside the home can isolate caregivers and family members of a person with dementia | |
Workshop 2
In the second workshop, we introduced the second stage of DT (Define) and used convergent thinking and prioritization techniques to review the themes to seek to define the right problem. More specifically, the caregivers were provided with a list of criteria (e.g., the solution exists for this problem; the problem is not as critical; the problem is not caregiving related; the problem is not worth tackling) to be considered to guide them to eliminate items perceived as least critical to them. They collectively agreed on a shorter, prioritized list of needs to be addressed through caregiving interventions, which lead to identifying a specific problem statement: ‘Caregivers and persons with dementia are in a vulnerable situation during the dementia post-diagnosis period.’ We used this statement to initiate the next two solution exploration phased of DT.
Workshop 3
Due to scheduling conflicts of the clinical researchers, the third and fourth workshops occurred on the same day. We started the third workshop by introducing the next DT phase (Develop) and used divergent thinking and brainstorming techniques to facilitate ideating several solution-focused caregiving interventions. We guided the brainstorming session on potential solutions by asking questions such as ‘What type of interventions can potentially support caregivers during the post-diagnosis time?’ We used slides simultaneously to facilitate conversations and record/visualize caregivers’ shared concepts. Using divergent thinking and keeping the problem statement in mind, caregivers jointly generated 14 interventions they felt would resolve their problem after the dementia diagnosis stage that could be included in the IMCC program. Caregivers broadly explored the solution space to support clinical, social, and individual aspects of caregiving. For example, they suggested developing an online repository of caregiving resources, creating peer-mentor programs/social media groups, and Tele-Savvy interventions to support individualized care (Table 3).
Table 3.
Intervention concepts examples developed by caregivers following divergent thinking.
| Problem statement | Proposed Interventions |
|---|---|
|
| |
| ‘Caregivers and persons with dementia are in a vulnerable situation during the dementia post-diagnosis period.’ | Universal care: One-stop shop to have a primary care |
| Resetting caregivers/family life: Identify what elements are essential to the quality of life of a family | |
| Individualized support: Provide personalized solution for each family | |
| Q: What type of interventions can potentially support caregivers during this critical time? | Create a balance between personalize mentors and automated resources (e.g., a website with all dementia-related resources) |
| Peer-mentors: Support groups in social media to answer caregivers’ questions and connect caregivers | |
Workshop 4
We started the fourth workshop by introducing the last phase of DT (Deliver) to validate the caregiving conceptual solutions. We used convergent thinking and prioritization techniques to narrow down the 14 intervention concepts. To minimize any potential bias in evaluating the proposed interventions, we invited three new caregivers to assess the 14 concepts. We provided several criteria to facilitate the convergence process, including the novelty, thoughtfulness, relevance of each intervention concept to caregiving. Together, caregivers converged their ideas to one and agreed that the most critical need IMCC could address would be to ‘provide a comprehensive orientation program to new caregivers.’ Throughout the workshops, caregivers were the primary participants/respondents to share their ideas about their experiences. While clinical researchers were careful about inappropriate interruptions to caregivers’ opinions, in workshops 3 and 4, we observed cases where they joined the brainstorming sessions to add their expert input, share insights to enrich the conversations, and discuss the feasibility of the proposed solutions.
Data Collection and Analysis Methods
Our primary goal in conducting the DT workshops was to train researchers with DT skills in the context of dementia caregiving. Our primary research question explored: ‘How would Design Thinking benefit researchers in developing caregiving research initiatives/interventions?’ We sought to answer this question by examining whether the DT workshops improved clinical researchers’ skills in problem-solving and human centredness (Aflatoony et al. 2018).
We asked participating researchers to complete pre-and post- DT workshop questionnaires to assess their understanding of DT, in this case in the context of dementia caregiving. Several pre- and post- surveys questions were identical to help us compare researchers’ knowledge before and after attending the workshops, their understanding of DT in the caregiving context, their plans to use DT principles in developing caregiving interventions, their insights about caregiving challenges, and the issues they sought to address through their intervention design/research to support caregiving mastery. Some of the survey questions were open-ended, and some were structured (closed type), which enabled us to collect both qualitative and quantitative data (please see Appendix A).
We distributed the surveys using Qualtrics and left the survey open for one week after completing the workshops. Seventeen researchers completed the pre-survey, and, despite sending them reminders, only eleven completed the post-survey in total. To analyse the qualitative data, we used open coding and the affinity diagram method, an inductive process to analyse the survey data for recurring patterns and emerging themes (Holtzblatt and Beyer 2017). We categorized the data into three common themes as described in the next section. The numeric/quantitative data were calculated using a formula in the Excel Sheet and cross-referenced with analysed data in Qualtrics.
Results
Overall, our findings indicated that the application of DT supported researchers’ understanding of the caregiving context, including caregivers’ challenges/needs (defining the right problem) and the researchers’ exploration of the type of interventions that potentially support caregiving mastery (defining the right solutions). Researchers were empathetic towards caregivers’ challenges, valued the shared information, and reflected on the issues by citing concrete examples from the workshop in the post-survey. Quantitative data analysis demonstrated an improvement in participants’ understanding of DT in developing caregiving interventions and their plans to engage caregivers in designing the interventions. We further describe these findings below.
The Overall Perception and Recognition of Design Thinking
Researchers’ understanding of the use of DT in developing caregiving interventions improved considerably after attending the workshop. As Table 4 illustrates, there was a nearly three-fold increase in researchers ‘Very Well’ or ‘Moderately Well’ indications of their familiarity and understanding of DT principles post-workshop. Likewise, as illustrated in Table 5, researchers reported a marked increase in their likelihood of employing DT principles in the design of caregiver interventions.
Table 4.
Participants’ degrees of understanding of Design Thinking in developing caregiving interventions in pre- and post-survey.
| Pre-Survey | Count | Post-Survey | Count | |
|---|---|---|---|---|
|
| ||||
| Extremely well | 0% | 0 | 0% | 0 |
| Very well | 11.76% | 2 | 18% | 2 |
| Moderately well | 11.76% | 2 | 54% | 6 |
| Slightly well | 29.41% | 5 | 27% | 3 |
| Not well at all | 47.06% | 8 | 0.00% | 0 |
| Mean | 4.12 | 3.09 | ||
| SD | 1.02 | 0.67 | ||
Table 5.
Participants plan to engage caregivers in designing the interventions in pre- and post-survey.
| Pre-Survey | Count | Post-Survey | Count | |
|---|---|---|---|---|
|
| ||||
| Not at all/rarely use it in a project | 58.82% | 10 | 9.09% | 1 |
| Occasionally in a project | 11.76% | 2 | 18.18% | 2 |
| Early in a project | 5.88% | 1 | 54.55% | 6 |
| Throughout the entire project | 23.53% | 4 | 18.18% | 2 |
| Mean | 1.94 | 3 | ||
| SD | 1.26 | 1.13 | ||
Perception of Caregiving Challenges
The challenges of finding resources, especially at the point of diagnosis, were raised by the caregivers and endorsed by the researchers. Importantly, researchers recognized the interconnectedness and complexity of caregivers’ challenges. For example, one researcher mentioned the difficulty of: ‘… reconciling the tension between wanting to protect the person from harm and honouring preferences and promoting quality of life.’ Challenges such as this were brought up by caregivers and were discussed in depth during the workshops.
Additionally, in the pre-survey responses, the clinical researchers’ reflections on caregiving problems were quite broad and suffered from a lack of specificity. For example, one researcher suggested that caregivers ‘cannot take care of themselves; they are exhausted; they do not have enough support to do what they need to do.’ Others seemed uncertain about the challenges. For example, one researcher stated: ‘the demands of caregiving may prevent participation in usual social circles and activities’ or ‘[they are] overwhelmed, so may not feel they have the time to evaluate options.’
Post-survey responses showed that researchers had gained a substantially better understanding of caregivers’ needs through the empathizing component of DT. They pointed to social and cultural caregiving challenges that ‘do not support continued engagement and quality of life for PwD [people with dementia]/families].’ They identified caregivers’ added psychological challenges and emotional pressures, including ‘dealing with the loss of the individual even though they are still present.’ Additionally, researchers identified ‘scattered resources’ as a significant challenge that caregivers brought up several times, as well as frustrations related to ‘overwhelming volume of resources,’ ‘fragmented care system,’ and ‘lack of individualization of resources.’
Insights on Caregiver-Specific Interventions
We asked the researchers about their plans for developing interventions to address caregiving challenges and what changes they made to the plan after attending the workshops. Most indicated an intent to alter or improve their research plan, particularly by integrating a more human (caregiver)-centred approach to their intervention processes: ‘After attending the design thinking workshops and webinars, I did change my research plan to incorporate provider training and to coordinate with existing caregiving support groups.’ Researchers provided much more comprehensive answers in the post-survey. For example, in the pre-survey a participant shared her project plan as ‘Motivating care providers to perform daily oral hygiene.’ In the post-survey, after reflecting on her approach, she expressed: ‘The scope of my problem has changed beyond teaching oral hygiene to caregivers - and is now inclusive of anticipatory guidance re: oral health problems, provider education, and insurance resources. … I realize how important it is for me to think about an intervention that will not add to their burden by working with providers and existing caregiving support groups.’
Researchers’ post-survey responses emphasized creative thinking, empathizing with caregivers, and recognizing the need for a more comprehensive intervention to meet complex, intertwined problems. Some planned to: ‘Incorporate questions from the webinar into the interviews with caregivers’ to closely engage them in developing caregiving-related interventions. Most spoke to the need for embracing caregiver-centred research activities and involving caregivers frequently in research: ‘Creation of an advisory board inclusive of caregivers that will be integral from the very beginning to the end’ and ‘I include CGs in all stages of intervention development; especially during phase 1A/1B development.’
Perspectives on Human (Caregiver)-Centred Approach
The researchers collectively reflected positively on the caregiver-centred approach as the main benefit of the DT workshops, how it helped them in current/future caregiving research projects/intervention development. The workshops introduced participants to the application of the human-centred process (DT) in developing caregiving interventions, using tangible examples: ‘Before the webinar, I only knew in ‘theory,’ what design thinking was; now I have an example of the process.’ Alternatively, ’Nice examples of incorporating CG [Caregiver] input into design!’ Participants acknowledged the importance of incorporating caregivers’ input throughout the intervention development processes: ‘The main benefit of the workshop series was the ability to hear from caregivers themselves. Tremendously helpful!’ They recognized the necessity of involving the caregivers in interventions development: ‘I think I am encouraged to bring in caregiver voices earlier’ or ‘identifying the need to bring caregivers more fully into the design process.’
Additionally, researchers recognized the need for divergent and convergent thinking in collecting, prioritizing, and organizing data/thoughts, leading to novel insights: ‘Great model of using/organizing lots of input and creativity […] New thoughts around how to research cultural aspects of caregiving.’ The DT workshop also acted as a piece of confirmatory evidence for those who were aware of the significance of involving caregivers in intervention development: ‘I am working with a colleague, and we are planning the inclusion of caregivers in our work, so this reinforces that plan.’ Also, some asked whether DT can be used in ‘Adaptation of currently existing caregiver interventions.’ However, some researchers were concerned about ‘How to talk about research and its importance with caregivers; caregiver preferences for data collection, recruitment, and dissemination.’
Discussion and Contributions
This article details the processes of incorporating DT in training medical researchers to recognize the dementia caregiving problem and solution spaces in greater depth through empathy, a caregiver-centred approach to research. Our findings revealed the benefit of DT to support researchers in having clear perceptions of caregiving problem space and speculating future caregiving-specific interventions that can augment caregiving mastery. The quantitative and qualitative results indicate researchers’ improved understanding of DT recognition in the caregiving context and developed clear insights on caregiving challenges and caregiving-specific interventions.
While the collaborative and participatory nature of DT has some overlaps with participatory approaches to design, the framework’s creative problem-solving qualities support developing innovative interventions. The Double Diamond framework’s convergent and divergent thinking modes/associated techniques amplify identifying critical problems and unique solutions to the issues. Such an outcome can only be achieved by following the proposed phases of Discover, Define, Develop, and Deliver closely. Additionally, the empathizing strategies in DT encourage/advance researchers’ skills to investigate and discover less-obvious and unspoken challenges, enabling them to practice human-centredness capacities/skills. In the following sections, we further discuss these qualities and benefits as they contribute to caregiving research and beyond in recognizing urgent matters, revealing implicit needs, and producing original research initiatives in healthcare.
Recognition of and Responsiveness to Urgent Matters in Healthcare
Studies in DT emphasized the rapid nature of the DT method as a catalyst in seeking resolutions to rapidly raising situations in healthcare (Thakur et al. 2021). The process allows recognition of early solutions as a means to support ‘exploring and defining problems and solutions together’ (Cross 2001). The rapid-iterative DT strategies provide a holistic view of complex situations, resulting in innovative solutions to healthcare problems (Abookire et al. 2020). In our study, divergent thinking strategies allowed caregivers to share many insights about their everyday challenges (e.g., avoid conflicts in public). Some issues were unexpected for participating researchers and opened opportunities for richer conversations and further examination of the topic. Additionally, the convergent thinking mode facilitated discovering urgent matters among others, identifying critical caregiving situations, and prioritizing interventions that required the research community’s close attention.
Divergently exploring the solution space provided new insights on the co-development of novel intervention directions that each can be developed as a new research program. As Ward (2015, p. 229) described: ‘Designers materialize thought in order to push the boundaries of knowledge.’ Such an approach reveals new avenues for innovation in healthcare beyond quality improvement initiatives and ‘helps to envision new possibilities to enable people to improve health’ (Noël and Frascara 2016). The convergent thinking mode supported prioritizing and getting potential interventions right, based on enriched co-conversations and co-investigation of issues (Sanders and Stappers 2008). The DT method created awareness among the researchers about realistic caregiving situations and reinforced the value and necessity of involving caregivers throughout the intervention development processes. Researchers acknowledged receiving thoughtful insights and knowledge from caregivers, associated with their close involvement in caregiving activities and reflection on their experiences. The method served as proof of evidence against inaccurate or ill-defined problems associated with limited understanding of situations or unproven assumptions (Cross 2017). Several researchers expressed the need to revise their research plans, define problem statements more precisely, and invite caregivers to assist earlier with the project as caregiving experts.
Revealing Implicit Needs through Exchange of Knowledge
In clinical practice, creating a shared understanding of a situation by frontline staff is necessary (Lin et al. 2015). In traditional clinical research, not much emphasis has been made on developing a shared understanding of a situation through exchanging knowledge among patients and researchers. It is common to refer to existing data and second-hand resources. We observed several instances of explicit knowledge transformation among participants during the workshops that created momentum for richer conversations. In the empathize phase, the caregivers exchanged the challenges of caregiving by sharing their everyday experiences. This shared knowledge is tacit, rooted in implicit caregiving needs and developed through ‘learning by doing’ caregiving activities. Thus, it is hard to find from second-hand data resources and can only be achieved through externalizing first-hand experiences (Thoring and Mueller 2011). In another example, in the define phase, the insights created a shared understanding of the situation or supported ‘mutual learning’ by incorporating collective rational and more intuitive decision-making through convergent thinking (Aflatoony and Lee 2020). This process enabled identifying a unique ‘problem statement’ that acted as a common ground for exploring the solution. The ideation techniques acted as innovation catalysts, where divergent insights and knowledge representations arose to explore and define the right solution. New ideas have been created collectively through internalizing explicit knowledge and externalizing tacit knowledge (Thoring and Mueller 2011). Such an enriched knowledge exchange enabled revealing implicit caregiving needs, which can be resolved through ‘interdisciplinary collaborations that integrate design and health in a problem-based learning context’ (Noël and Frascara 2016).
Producing Original Health Care Research and Contributions
In scholarly research, conducting original research and making a novel contribution to the knowledge of the field is critical but challenging, especially for novice researchers (Lovitts 2005). Producing quality original research requires creative intelligence associated with solving a well-defined problem and managing ambiguous research processes. Such an approach can eventually contribute to establishing a significant piece that transforms the knowledge of the domain (Lovitts 2005). DT can be used as a catalyst in producing novel contributions to advanced/scholarly research by supporting researchers’ creative problem-solving skills. Studies showed that training clinical researchers with DT can resolve complex structural health care issues (Van De Grift and Kroeze 2016), and inspiring innovative public health interventions (Abookire et al. 2020). Additionally, since most healthcare conditions are multilayered and intertwined with physiological, psychological, social, and cultural needs of patients/care providers, the DT iterative process of co-developing interventions provides a clear insight into the likelihood of research project success before initiating them. The iterative process of moving through concept generation, prototyping, and testing with users prompts a ‘fail early and often’ approach for reaching a solution confidently (Thoring and Müller 2011). Such a process can potentially eliminate or reduce any failure/negative outcomes later on when providing patient care. Additionally, the DT outcome can be recorded systematically and demonstrated as pilot data for future research initiatives.
We anticipate that DT can be incorporated into training researchers as a complementary approach to conventional intervention development research methods. For example, DT can be used explicitly in the early phases of research initiatives for need assessment purposes, in cases that problems are ill-identified due to limited understanding of situations (Cross 2017), or attempts to problem-solve have failed to investigate the users’ needs succinctly and generate critical insights through qualitative evaluation of generated concepts (Roberts et al. 2016). In our study, the lack of knowledge in dementia caregiving made a case for rapidly incorporating DT to explore caregivers’ initial needs and conceptualization of solutions. We argue for the benefit of DT for clinical researchers as a rapid tool to support pilot studies/proof of concept interventions, which can be supported later through advanced clinical research methods with a larger sample size to produce generalizable outcomes.
Study Limitations
Our study has some limitations to be considered. While the flexible nature of the method enabled us to bring together clinicians/specialists from different institutions and access researchers nationwide, we could not incorporate hands-on prototyping in action or standard ideation methods (e.g., sketching) in the Develop stage. Instead, we facilitated the discussions and visualized the information in real-time to support caregivers’ idea generation. Likewise, the last phase emphasizes evaluating conceptual ideas, so no concrete evaluation methods have been used (e.g., user study). So, the last two intervention development phases have been limited to idea generation through discussion. Additionally, even though clinical researchers were enthusiastic about/participated in the workshops and sent out reminders, not all completed the pre- and post-surveys. So, the information provided is limited to their experience and does not represent a larger clinical researcher population.
Conclusion and Future Work
In this study, we implemented a series of Design Thinking workshops within the context of dementia caregiving mastery. This initiative aimed to provide training to clinical researchers in preparing caregiver-centred research initiatives through activities that encouraged empathizing with dementia family caregivers. Our findings revealed the benefit of the workshop by providing researchers an insight into the Design Thinking concept, caregiving challenges, and speculating caregiving-specific interventions. We discussed the contribution of our study to significantly understudied/new healthcare areas by rapidly supporting the 1) Recognition of urgent matters in the field, 2) Revelation of implicit needs through the exchange of expert knowledge, and 3) Production of original knowledge contributions to the field. Our future study explores the Design Thinking application/benefit in the context of health inequity/disparity to train clinical researchers in developing research initiatives to resolve caregiving challenges of marginalized and underrepresented minority populations.
Acknowledgement
We sincerely thank all our participants, including dementia caregivers and clinical researchers, who have participated in this study. This research was supported by grant 5P30AG064200 from the National Institute on Aging at the National Institutes of Health (NIH/NIA), awarded to Hepburn and Perkins.
Appendix A: Pre/Post Webinar Survey Questions
Pre-Survey Questions:
What is your area of expertise? ---
What is your academic rank? ---
How well do you understand the use of Design Thinking in developing caregiving interventions?
- To what extent do you use Design Thinking principles in developing your care giving interventions?
- 1) Not at all 2) Occasionally 3) Early in design process 4) Throughout the entire project
- From your perspective, what are the three greatest challenges that caregivers face in providing care/support for individuals with dementia on a daily basis? Briefly describe each challenge.
- Challenge 1:
- Challenge 2:
- Challenge 3:
What is the main challenge in caregiving that you are trying to address in your intervention research?
In your opinion, what type of intervention are you thinking will address the above-mentioned challenge and/or support caregiving mastery?
What is your expectation about the webinar? How do you hope it will help your thinking in respect to the challenge and intervention?
Post-Survey Questions:
What is your area of expertise? ---
What is your academic rank? ---
How well do you understand the use of Design Thinking in developing caregiving interventions?
- Based on your participation in the workshop, to what extent do you engage caregivers in designing the interventions?
- 1) Not at all 2) Occasionally 3) Early in design process 4) Throughout the entire project
- From your perspective, what are the three greatest challenges that caregivers face in providing care/support for individuals with dementia on a daily basis? List three challenges and briefly describe each.
- Challenge 1:
- Challenge 2:
- Challenge 3:
How do you now define the main challenge in caregiving that you are trying to address in your research?
Do you plan to make any changes to your research plans/proposal (defining problem, type of intervention, etc) after attending the webinar?
How do you plan now to engage caregivers in the design of the intervention?
In what way the Webinars series helped you in current/future caregiving research projects/intervention development/grant writing?
References
- Abookire S, Plover C, Frasso R, & Ku B (2020). Health Design Thinking: An Innovative Approach in Public Health to Defining Problems and Finding Solutions. Frontiers in Public Health, 8(August), 1–6. 10.3389/fpubh.2020.00459 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aflatoony L, & Lee S (2020). AT Makers: A Multidisciplinary Approach to Co-Designing Assistive Technologies by Co-Optimizing Expert Knowledge. ACM International Conference Proceeding Series, 2, 128–132. 10.1145/3384772.3385158 [DOI] [Google Scholar]
- Aflatoony L, Wakkary R, & Neustaedter C (2018). Becoming a Design Thinker: Assessing the Learning Process of Students in a Secondary Level Design Thinking Course. International Journal of Art and Design Education, 37(3), 438–453. 10.1111/jade.12139 [DOI] [Google Scholar]
- Altman M, Huang TTK, & Breland JY (2018). Design thinking in health care. Preventing Chronic Disease, 15(9), 1–13. 10.5888/pcd15.180128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beaird G, Geist M, & Lewis EJ (2018). Design thinking: Opportunities for application in nursing education. Nurse Education Today, 64(October 2017), 115–118. 10.1016/j.nedt.2018.02.007 [DOI] [PubMed] [Google Scholar]
- Clevenger CK, Cellar J, Kovaleva M, Medders L, & Hepburn K (2018). Integrated Memory Care Clinic: Design, Implementation, and Initial Results. Journal of the American Geriatrics Society, 66(12), 2401–2407. 10.1111/jgs.15528 [DOI] [PubMed] [Google Scholar]
- Cravens AE, Cornelius M, Ulibarri N, Royalty A, & Nabergoj AS (2014). Reflecting, Iterating, and Tolerating Ambiguity: Highlighting the Creative Process of Scientific and Scholarly Research for Doctoral Education. International Journal of Doctoral Studies, 9, 229–247. 10.28945/2058 [DOI] [Google Scholar]
- Cross N (2001). Design Cognition: Results from Protocol and other Empirical Studies of Design Activity. In Design Knowing and Learning: Cognition in Design Education (pp. 79–103). Elsevier Science. 10.1016/B978-008043868-9/50005-X [DOI] [Google Scholar]
- Cross N (2017). Design Ability. Design Thinking. 10.5040/9781474293884.ch-001 [DOI] [Google Scholar]
- Deitte LA, & Omary RA (2019). The Power of Design Thinking in Medical Education. Academic Radiology, 26(10), 1417–1420. 10.1016/j.acra.2019.02.012 [DOI] [PubMed] [Google Scholar]
- Ferreira FK, Song EH, Gomes H, Garcia EB, & Ferreira LM (2015). New mindset in scientific method in the health field: Design thinking. Clinics, 70(12), 770–772. 10.6061/clinics/2015(12)01 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gottlieb M, Wagner E, Wagner A, & Chan T (2017). Applying Design Thinking Principles to Curricular Development in Medical Education. AEM Education and Training, 1(1), 21–26. 10.1002/aet2.10003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henderson VA, Barr KLC, An LC, Guajardo C, Newhouse W, Mase R, & Heisler M (2013). Community-based participatory research and user-centered design in a diabetes medication information and decision tool. Progress in Community Health Partnerships: Research, Education, and Action, 7(2), 171–184. 10.1353/cpr.2013.0024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holtzblatt K, & Beyer H (2017). The Afnity Diagram. In Contextual Design 10.1016/b978-0-12-800894-2.00006-5 [DOI] [Google Scholar]
- Jonas L, & Stolterman E (2004). Thoughtful Interaction Design: A Design Perspective on Information Technology. The MIT Press. [Google Scholar]
- Lin M, Heisler S, Fahey L, McGinnis J, & Whiffen TL (2015). Nurse knowledge exchangeplus: Human-centered implementation for spread and sustainability. Joint Commission Journal on Quality and Patient Safety, 41(7), 303–312. 10.1016/s1553-7250(15)41040-2 [DOI] [PubMed] [Google Scholar]
- Lovitts BE (2005). Being a good course-taker is not enough: A theoretical perspective on the transition to independent research. Studies in Higher Education, 30(2), 137–154. 10.1080/03075070500043093 [DOI] [Google Scholar]
- Luna DR, Rizzato Lede DA, Otero CM, Risk MR, & González Bernaldo de Quirós F (2017). User-centered design improves the usability of drug-drug interaction alerts: Experimental comparison of interfaces. Journal of Biomedical Informatics, 66, 204–213. 10.1016/j.jbi.2017.01.009 [DOI] [PubMed] [Google Scholar]
- Lyon AR, & Koerner K (2016). User-Centered Design for Psychosocial Intervention Development and Implementation. Clinical Psychology: Science and Practice, 23(2), 180–200. 10.1111/cpsp.12154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madson MJ (2021). Making sense of design thinking: A primer for medical teachers. Medical Teacher, 0(0), 1–14. 10.1080/0142159X.2021.1874327 [DOI] [PubMed] [Google Scholar]
- McLaughlin JE, Wolcott MD, Hubbard D, Umstead K, & Rider TR (2019). A qualitative review of the design thinking framework in health professions education. BMC Medical Education, 19(1), 1–8. 10.1186/s12909-019-1528-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noël G, & Frascara J (2016). Health and Design - Fostering a culture of collaboration through education. Health Design Network, August. [Google Scholar]
- Padagas RC (2021). Design Thinking in a Professional Nursing Course – Its Effectiveness and Unearthed Lessons. Revista Romaneasca Pentru Educatie Multidimensionala, 13(2), 132–146. 10.18662/rrem/13.2/414 [DOI] [Google Scholar]
- Roberts JP, Fisher TR, Trowbridge MJ, & Bent C (2016). A design thinking framework for healthcare management and innovation. Healthcare, 4(1), 11–14. 10.1016/j.hjdsi.2015.12.002 [DOI] [PubMed] [Google Scholar]
- Rowe A, Knox M, & Harvey G (2020). Re-thinking health through design: collaborations in research, education and practice. Design for Health, 4(3), 327–344. 10.1080/24735132.2020.1841918 [DOI] [Google Scholar]
- Sandars J, & Goh P-S (2020). Design Thinking in Medical Education: The Key Features and Practical Application. Journal of Medical Education and Curricular Development, 7, 238212052092651. 10.1177/2382120520926518 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanders EB-N, & Stappers PJ (2008). Co-creation and the new landscapes of design. Co-Design, 4(1), 5–18. 10.1080/15710880701875068 [DOI] [Google Scholar]
- Searl MM, Borgi L, & Chemali Z (2010). It is time to talk about people: A human-centered healthcare system. Health Research Policy and Systems, 8, 1–7. 10.1186/1478-4505-8-35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thakur A, Soklaridis S, Crawford A, Mulsant B, & Sockalingam S (2021). Using Rapid Design Thinking to Overcome COVID-19 Challenges in Medical Education. Academic Medicine, 96(1), 56–61. 10.1097/ACM.0000000000003718 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thoring K, & Mueller R (2011). CREATING KNOWLEDGE IN DESIGN THINKING: THE RELATIONSHIP OF PROCESS STEPS AND KNOWLEDGE TYPES. In Roozenburg NFM, Chen LL, & Stappers PJ (Eds.), Proceedings of IASDR2011, the 4th Word Conference on Design Reserach. [Google Scholar]
- Thoring K, & Müller R (2011). Design Thinking; Evolutionary Methods; Creative Education. DESIRE - Procedings of the Second Conference on Creativity and Innovation in Design, 2, 137–147. [Google Scholar]
- Van De Grift TC, & Kroeze R (2016). Design thinking as a tool for interdisciplinary education in health care. Academic Medicine, 91(9), 1234–1238. 10.1097/ACM.0000000000001195 [DOI] [PubMed] [Google Scholar]
- van der Weegen S, Verwey R, Spreeuwenberg M, Tange H, van der Weijden T, & de Witte L (2013). The Development of a Mobile Monitoring and Feedback Tool to Stimulate Physical Activity of People With a Chronic Disease in Primary Care: A User-Centered Design. JMIR Mhealth and Uhealth, 1(2), e8. 10.2196/mhealth.2526 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Velardo C, Shah SA, Gibson O, Clifford G, Heneghan C, Rutter H, Farmer A, & Tarassenko L (2017). Digital health system for personalised COPD long-term management. BMC Medical Informatics and Decision Making, 17(1), 1–13. 10.1186/s12911-017-0414-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ward M (2015). Rapid prototyping politics: Design and the de-material turn. In and von A. Wolfgang Jonas K, Zerwas Sarah (Ed.), Transformation Design: Perspectives on a New Design Attitude (Issue Brown 2008, pp. 227–245). Basel: Birkhauser. 10.1515/9783035606539-017 [DOI] [Google Scholar]
- Wentzel J, Van Drie-Pierik R, Nijdam L, Geesing J, Sanderman R, & Van Gemert-Pijnen JEWC (2016). Antibiotic information application offers nurses quick support. American Journal of Infection Control, 44(6), 677–684. 10.1016/j.ajic.2015.12.038 [DOI] [PubMed] [Google Scholar]
- Wolcott MD, & McLaughlin JE (2020). Promoting creative problem-solving in schools of pharmacy with the use of design thinking. American Journal of Pharmaceutical Education, 84(10), 1271–1276. 10.5688/ajpe8065 [DOI] [PMC free article] [PubMed] [Google Scholar]


