Abstract
Background
Atopic dermatitis (AD) is a common inflammatory skin disease that compromises the skin's barrier function and capacity to retain moisture. Cnidii Fructus (CF), the dried fruits of Cnidium monnieri, has long been used to treat atopic dermatitis (AD) in China. However, the anti-AD compounds and mechanisms of CF are not fully understood. In this study, we evaluated the active compounds and molecular targets of CF in treating AD.
Methods
The Traditional Chinese Medicine Systems Pharmacology database was used to acquire information regarding the compounds that occur in the herb. Targets of these compounds were predicted using the SwissTargetPrediction website tool. AD-related genes were collected from the GeneCards database. Gene ontology (GO) enrichment analysis and KEGG pathway analysis of proteins that are targeted by active compounds of CF and encoded by AD-related genes were performed using Database for Annotation, Visualization, and Integrated Discovery Bioinformatics Resources. A “compound-target” network was constructed and analyzed using Cytoscape Software. Molecular docking was performed using BIOVIA Discovery Studio Visualizer and AutoDock Vina.
Results
We identified 19 active compounds in CF, 532 potential targets for these compounds, and 1540 genes related to AD. Results of GO enrichment indicated that CF affects biological processes and molecular functions, such as inflammatory response and steroid hormone receptor activity, which may be associated with its anti-AD effects. KEGG pathway analyses showed that PI3K-Akt signaling, calcium signaling, Rap1 signaling, and cAMP signaling pathways are the main pathways involved in the anti-AD effects of CF. Molecular docking analyses revealed that the key active compounds in CF, such as (E)-2,3-bis(2-keto-7-methoxy-chromen-8-yl)acrolein, ar-curcumene, and diosmetin, can bind the main therapeutic targets AKT1, SRC, MAPK3, EGFR, CASP3, and PTGS2.
Conclusions
Results of the present study establish a foundation for further investigation of the anti-AD compounds and mechanisms of CF and provide a basis for developing modern anti-AD agents based on compounds that occur in CF.
Keywords: Cnidium monnieri, Network pharmacology, Atopic dermatitis, Gene Ontology, KEGG pathway
Introduction
Atopic dermatitis (AD)), also known as atopic eczema, is an inflammatory dry skin disease [1, 2]. The frequency and prevalence of AD have steadily grown over the last several decades [1, 3, 4]. AD affects people of all ages but is most often diagnosed during infancy and early childhood. It may persist until maturity and can emerge during adulthood. According to Global Burden of Disease, AD has a prevalence of 15–20% in children and up to 10% in adults, making it the 15th most prevalent nonfatal skin disease. Both males and females are afflicted, and the incidence varies according to race and ethnic group. In the United States, for example, the frequency is much greater among black children (19.3%) than among white children (16.1%) [5, 6]. Around 20% of the population in Hong Kong experiences AD at some point in their lives. Approximately 30% of children in Hong Kong are affected [7–9]. The increased occurrence has been provisionally related to environmental variables such as exposure to air pollution and home hygiene products in high-income and industrialized nations [1]. AD patients often experience itching; their skin can appear dry, cracked and red, and is often thickened. On the cellular level, AD is typically accompanied by keratinocyte apoptosis [10, 11].
AD is thought to be caused by a disruption of the epidermal barrier that allows allergens to penetrate the epidermis and activate dendritic and innate lymphoid cells, which then attract and activate Th2 cells [12]. These activated and dysregulated Th2 cells produce inflammatory cytokines (IL-4, IL-13, and IL-31) in the skin, activating Janus kinase (Jak) pathways. Active Jak pathways activate plasma cells and B lymphocytes, which generate antigen-specific IgE, aggravating the inflammatory response further [13–15].
AD has no definitive cure, and current treatment consists primarily of topical anti-inflammatory agents such as corticosteroids and calcineurin inhibitors. Corticosteroids, powerful anti-inflammatory medicines, have been demonstrated to be beneficial for both acute and chronic AD [11, 16]; however, continuous utilization of topical corticosteroids may result in adverse side effects such as permanent skin thinning and systemic inhibition of adrenal function [11, 17]. Topical calcineurin inhibitors, such as tacrolimus and pimecrolimus, have been shown to ameliorate the symptoms by inhibiting the transcription of important AD-related cytokines (IL-2, IL-4, and IL-5). The US Food and Drug Administration, however, issued an advisory indicating a possible link between calcineurin inhibitors and cancer [18–20]. Traditional Chinese medicine (TCM) has been shown to provide safe, effective alternative immunotherapies for AD [11].
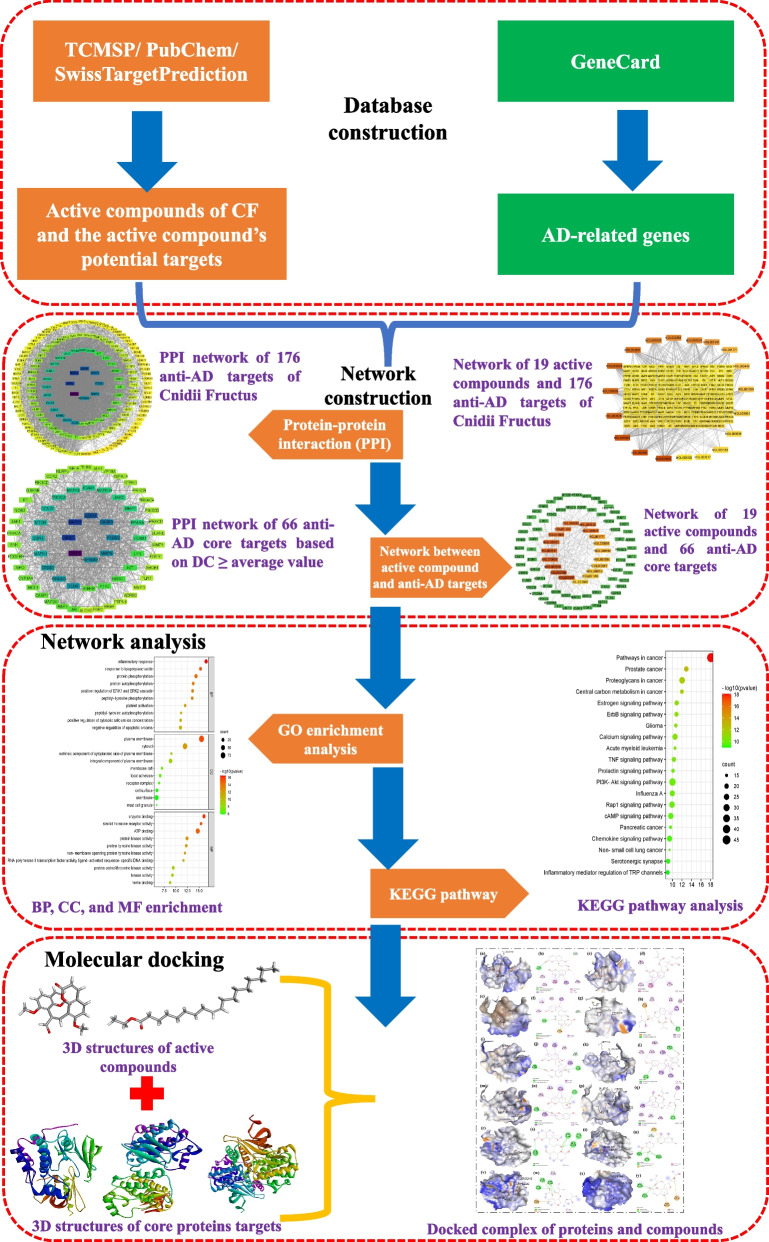
Cnidii Fructus (She Chuang Zi in Chinese; common name, Monnier's snow parsley; henceforth referred to here as CF) is the dried fruit of Cnidium monnieri (L.) Cuss. The use of CF in China can be traced back to Shennong's Classic of Materia Medica (Shennong Bencao Jing) written in the Eastern Han Dynasty (25–220 AD), i.e., close to 2000 years ago. CF is traditionally used for treating female genitals, kidney deficiency, male impotence, and skin-related diseases [21]. Water decoctions and tinctures of CF alone or in combination with other Chinese medicinal herbs are commonly used to treat intractable skin pruritus, superficial fungal diseases, and atopic dermatitis in current TCM clinical practice [22]. More than 400 chemical constituents have been identified in CF. These compounds are mainly categorized as glucides, glycosides, terpenoids, monoterpenoid glucosides, chromones, liposoluble compounds, volatile oils, and coumarins [23, 24]. Pharmacological studies demonstrated that extracts and components of CF have antibacterial, antifungal, anti-osteoporotic, anti-tumor, antiallergic, antipruritic, anti-inflammatory, anti-itching, and anti-dermatitic effects [22, 24]. Total coumarins isolated from CF have recently been reported to have anti-AD effects in a rat model [25]. However, the anti-AD compounds and mechanisms of CF in treating AD have not been fully elucidated. Network pharmacology and molecular docking are now commonly used to identify active pharmaceutical ingredients and understand the overall mechanisms of action of multicomponent herbal drugs [26]. In the present study, we used network pharmacology and molecular docking approaches to predict biologically active phytomolecules, as well as molecular targets and pathways, involved in the anti-AD effects of CF (Fig. 1).
Fig. 1.
Flowchart of this study
Materials and methods
Collection of active compounds of CF
Traditional Chinese Medicine Systems Pharmacology Database and Analysis Platform (TCMSP Version 2.3, https://old.tcmsp-e.com/tcmsp.php, accessed on December 10, 2021) was used to obtain the active phytomolecules of CF [27]. The TCMSP database includes information about the absorption, distribution, metabolism, and excretion (ADME) characteristics of each compound. Oral bioavailability “OB” is a term that refers to "the rate and degree to which an active component or active moiety is absorbed from a therapeutic product that becomes accessible at the targeted site". Drug Likeness “DL” is a qualitative paradigm for drug design that incorporates the ADME qualities of ingredients and established medications. The therapeutic compounds of CF that satisfy the requirements of both OB ≥ 30% and DL ≥ 0.18 [27–30] were collected for subsequent target prediction.
Target prediction of active compounds of CF
The potential targets of the active compounds of CF (with a probability score > 0) were predicted using the SwissTargetPrediction website tool (http://www.swisstargetprediction.ch/, accessed on December 10, 2021) [31].
Screening of disease-related genes
The AD-related genes were collected from GeneCards®: The Human Gene Database (https://www.genecards.org/, accessed on December 10, 2021) by searching using the keywords “atopic dermatitis”, “atopic dermatitis inhibiting” and “anti-atopic dermatitis” [32].
Identification of potential anti-AD targets of CF
Proteins that are compound targets and are encoded by AD-related genes were identified using the Venny 2.1 online software (https://bioinfogp.cnb.csic.es/tools/venny/, accessed on December 11, 2021). The common molecules were considered to be potential anti-AD targets of CF.
Protein–protein interaction analysis
The protein–protein interaction (PPI) between the potential anti-AD targets of CF was then analyzed by using the STRING database (https://string-db.org/, version 11.5, accessed on December 12, 2021) [33]. The confidence score was set to be > 0.4, and species was limited to “Homo sapiens”. The results of the PPI analysis were further visualized using Cytoscape Software (version 3.9.0, Boston, MA, the USA, accessed on December 14, 2021) [34].
Compound-target network construction
To analyze the interaction between active compounds and the anti-AD targets of CF, compound-target networks were constructed using Cytoscape Software (version 3.9.0, Boston, MA, USA, accessed on December 14, 2021) [34].
Enrichment analysis
Gene ontology (GO) functional enrichment analysis and Kyoto Encyclopedia of Genes and Genomes (KEGG) pathway enrichment analysis were carried out using the DAVID database for annotation, visualization, and integrated discovery (Version 6.8; https://david.ncifcrf.gov/, accessed on December 16, 2021) [35–37]. The GO terms were categorized into three types: cellular component (CC), biological process (BP), and molecular function (MF). By uploading the data to the Bioinformatics platform (http://www.bioinformatics.com.cn/), bubble plots of bioprocesses and pathways were drawn. Classical hypergeometric test was used to determine statistical significance. The adjusted p-value < 0.05 was utilized as the significance threshold in our investigation after utilizing the Benjamini–Hochberg method to control the false discovery rate (FDR) for multiple hypothesis testing [11].
Molecular docking
Two-dimensional (2D) structures of active compounds of CF were acquired in Spatial Data File (SDF) format from the NCBI PubChem (https://pubchem.ncbi.nlm.nih.gov/) online database. Their three-dimensional (3D) structures were constructed using BIOVIA Discovery Studio Visualizer 2021 and were saved in PDB format. Protein crystal structures of the potential targets (AKT1, MAPK3, SRC, EGFR, CASP3 and PTGS2) were obtained in PDB format from the Protein Data Bank (https://www.rcsb.org/) [38]. PDB IDs of the six potential targets are 3O96, 6GES, 2BDF, 5Y9T, 1NME and 5IKT, respectievly. BIOVIA Discovery Studio Visualizer 2021 Software was used for the extraction of the ligands and water molecules from the crystal structure complex. It was further employed for designing the grid and the preparation of proteins [39, 40]. The proteins in PDB format were uploaded to AutoDock Vina (version 1.2.0.), and the Kollman charges and Gasteiger partial charges were added to the receptor proteins. The key active compounds in PDB format were then uploaded to AutoDock Vina (version 1.2.0.). Both proteins and key active compounds were converted into pdbqt format using AutoDock Vina (version 1.2.0.). Finally, both proteins and key active compounds in pdbqt format were used for scriptwriting for molecular docking using AutoDock Vina (version 1.2.0.); from this, docked complex results were obtained [41]. The docked complex results were further visualized to estimate the binding ability of the molecules and targets using BIOVIA Discovery Studio Visualizer 2021 software [39]. A binding energy < 0 indicates that a ligand may spontaneously bind to the receptor. It is commonly recognized that the lower the energy score of the ligand and receptor binding configuration, the more probable the binding will occur [41].
Results
Active compounds of CF
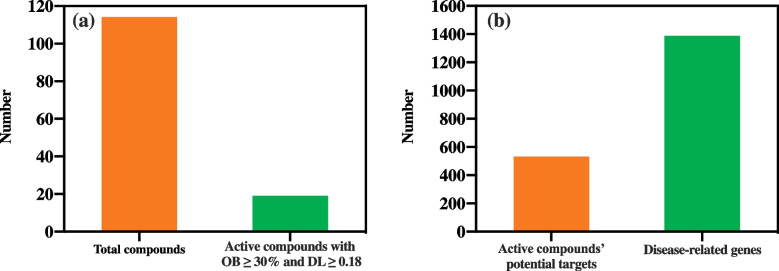
A total of 114 compounds of CF were extracted from the TCMSP. Further active compound screening was carried out based on OB ≥ 30% and DL ≥ 0.18; from this, 19 active compounds were obtained (Fig. 2a) as listed in Table 1.
Fig. 2.
a Total numbers of compounds and active compounds present in CF. b Total number of active compounds’ potential targets and disease-related genes
Table 1.
Active compounds of CF
| Serial No | Compound ID | Compound name | OB | DL | |
|---|---|---|---|---|---|
| Common name | Standard name | ||||
| 1 | MOL001510 | Campesterol | 24-epicampesterol | 37.58 | 0.71 |
| 2 | MOL001771 | Poriferast-5-en-3beta-ol | Poriferast-5-en-3beta-ol | 36.91 | 0.75 |
| 3 | MOL001941 | Imperatorin | Ammidin | 34.55 | 0.22 |
| 4 | MOL002881 | Diosmetin | Diosmetin | 31.14 | 0.27 |
| 5 | MOL002883 | Ethyl oleate | Ethyl oleate (NF) | 32.40 | 0.19 |
| 6 | MOL000358 | Beta-sitosterol | Beta-sitosterol | 36.91 | 0.75 |
| 7 | MOL003584 | Xanthoxyletin | Xanthoxylin N | 35.51 | 0.21 |
| 8 | MOL003588 | Alloimperatorin | Prangenidin | 36.31 | 0.22 |
| 9 | MOL003591 | Ar-curcumene | Ar-curcumene | 52.34 | 0.65 |
| 10 | MOL003600 | Cnidimol B | Cnidimol B | 68.66 | 0.26 |
| 11 | MOL003604 | Cnidimol F | Cnidimol F | 54.43 | 0.28 |
| 12 | MOL003605 | Cnidimonal | (E)-2,3-bis(2-keto-7-methoxy-chromen-8-yl)acrolein | 56.38 | 0.71 |
| 13 | MOL003606 | Cniforin A | Cniforin A | 55.89 | 0.47 |
| 14 | MOL003607 | Cniforin B | Cniforin B | 36.70 | 0.60 |
| 15 | MOL003608 | Columbianetin acetate | O-acetylcolumbianetin | 60.04 | 0.26 |
| 16 | MOL003617 | Isogosferol | Isogosferol | 30.07 | 0.25 |
| 17 | MOL003624 | O-isovalerylcolum bianetin | O-isovalerylcolum bianetin | 64.03 | 0.36 |
| 18 | MOL003626 | Ostruthin | Ostruthin | 30.65 | 0.23 |
| 19 | MOL000449 | Stigmasterol | Stigmasterol | 43.83 | 0.76 |
OB Oral bioavailability, DL Drug-likeness
Targets of CF’s active compounds
To obtain direct targets of the 19 active compounds of CF, ligand-based target prediction was performed using the SwissTargetPredictaion website tool. A total of 1387 potential targets (probability score > 0) were obtained. After eliminating redundancy, 532 predicted potential targets were selected for further analysis (Fig. 2b).
Disease-related genes
A total of 1540 AD-related genes were obtained by searching in the GeneCards database using the keywords “atopic dermatitis”, “atopic dermatitis inhibiting”, and “anti-atopic dermatitis” (Fig. 2b).
Intersection of AD-related gene products and compound targets in Venn diagram
Intersection of AD-related gene products and compound targets were identified using the Venny 2.1.0 online system. The results are presented in Fig. 3. A total of 176 compound targets that map with disease-gene products were considered to be potential anti-AD targets of CF.
Fig. 3.
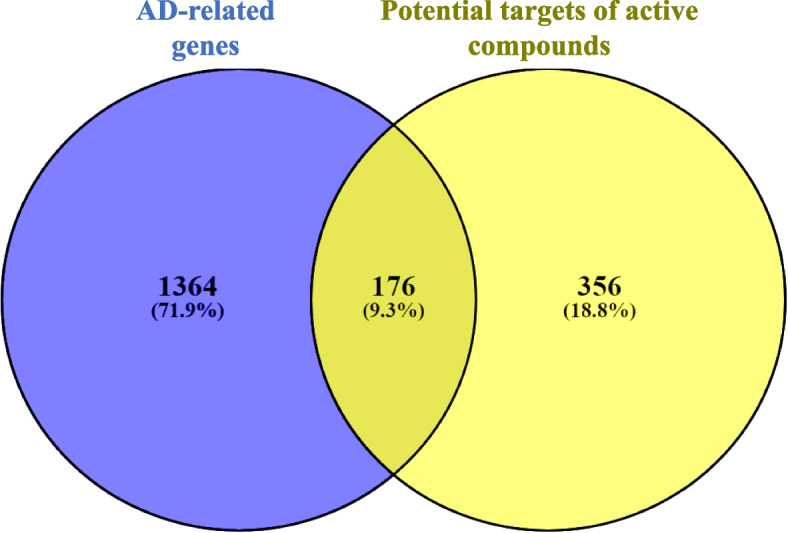
Venn diagram depicting the intersection of AD-related gene products and proteins targeted by CF’s active compounds
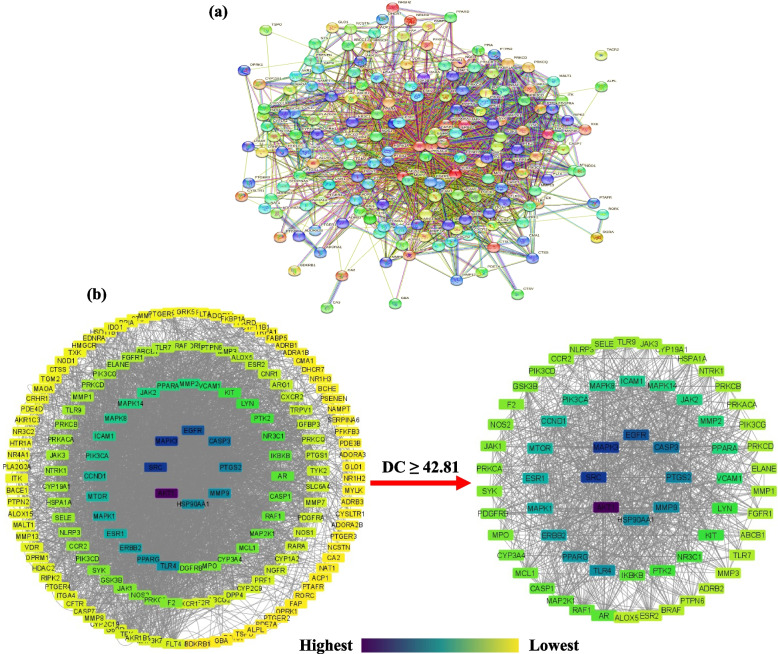
Analysis of protein–protein interaction (PPI)
The PPI network of the 176 potential anti-AD targets of CF was constructed by importing them into STRING Database 11.5 (Fig. 4a). The network contained 176 nodes and 1873 edges. Average node degree, average local clustering coefficient, and average PPI enrichment p-values were 21.3, 0.485, < 0.00001, respectively.
Fig. 4.
a PPI interaction network of 176 potential anti-AD targets of CF constructed using STRING Database 11.5. b PPI interaction network of the 176 potential anti-AD targets of CF and the 66 anti-AD core targets constructed using Cytoscape Software 3.9.0. DC denotes degree centrality. Node color represents degree of interaction from yellow (lowest) to purple (highest)
The PPI analysis results were further exported as a simple textual data format (.tsv) file and then imported to Cytoscape software 3.9.0 to obtain the PPI network. The results demonstrated that the network involved 175 nodes and 3748 edges, in which the average shortest path length value between all node pairs in the network was 2.148 with a network radius value of 3. Figure 4b depicts the network with the nodes as colored circles and the color of each node representing its degree, from yellow (lowest) to purple (highest). The 66 nodes that satisfied the criteria of degree centrality (DC) ≥ average value of (42.81) were further extracted and considered as anti-AD core targets (Fig. 4b). Ranked by DC, the 66 anti-AD core targets are presented in the form of a bar graph in Fig. 5. The top 6 anti-AD core targets, namely AKT1, MAPK3, SRC, EGFR, CASP3, and PTGS2, were selected for molecular docking that will be described in Network of active compounds and anti-AD targets of CF section.
Fig. 5.
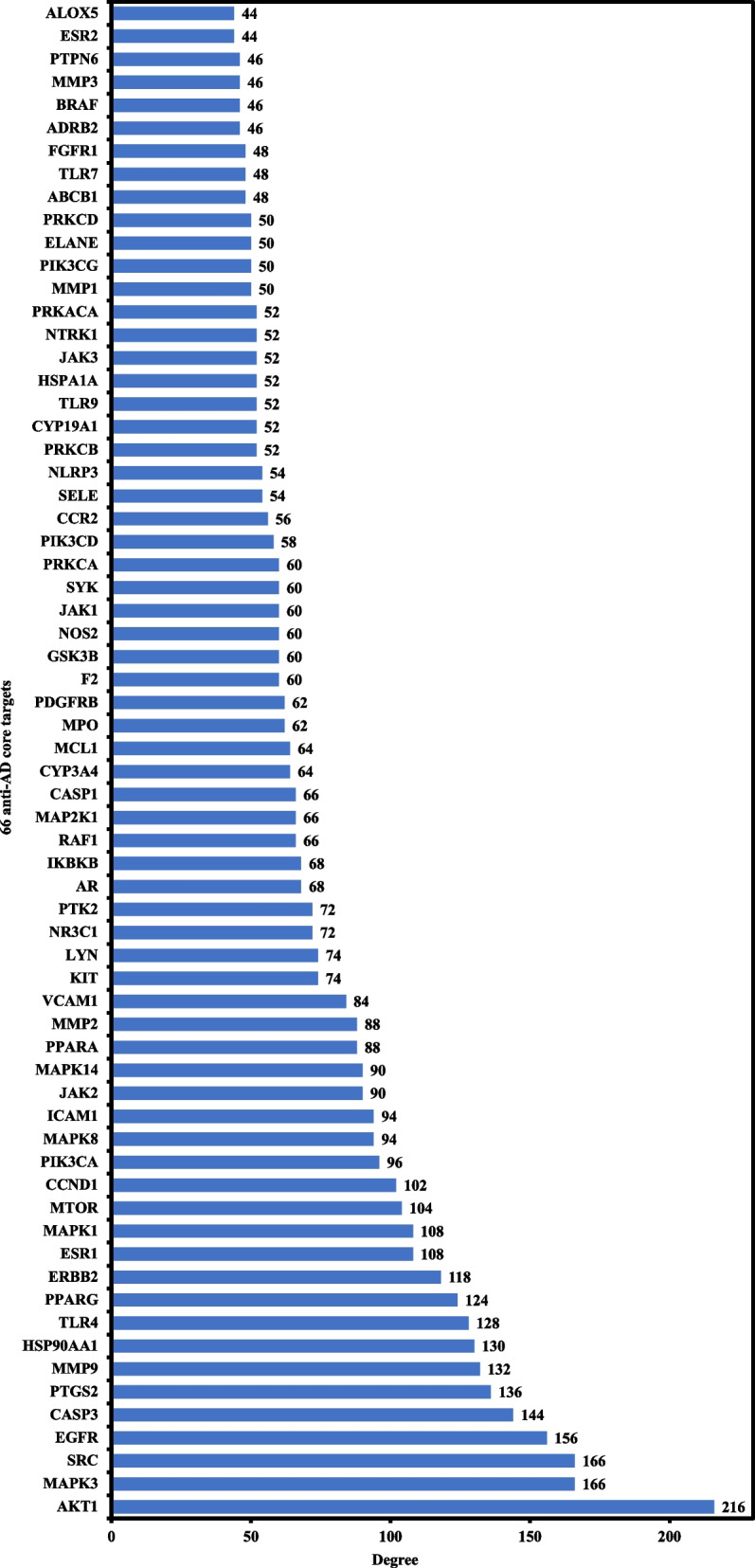
Bar graph of CF’s anti-AD core targets with DC ≥ 42.81
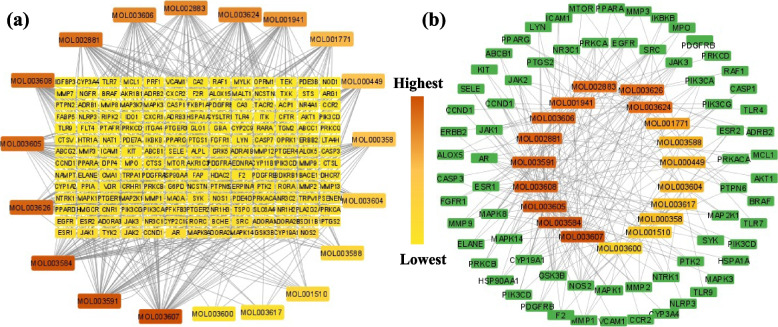
Network of active compounds and anti-AD targets of CF
A network displaying the 19 active compounds (determined as described in Active compounds of CF section) acting on the 176 anti-AD targets of CF (determined as described in Analysis of protein-protein interaction (PPI) section) was constructed using Cytoscape Software 3.9.0 (Fig. 6a). Results showed that the network has 201 nodes and 524 edges. Each edge denotes the connection of an active compound to an anti-AD target of CF. The color of each node of compounds shows the degree from lowest (yellow) to highest (red orange). The node degree represents the number of edges connected to this node in the network [42].
Fig. 6.
a Network of 19 active compounds and the anti-AD targets of CF. b Hub network of 66 anti-AD core targets and the 19 active compounds. Node colour represents degree (number of connections), from lowest (yellow) to highest (red orange)
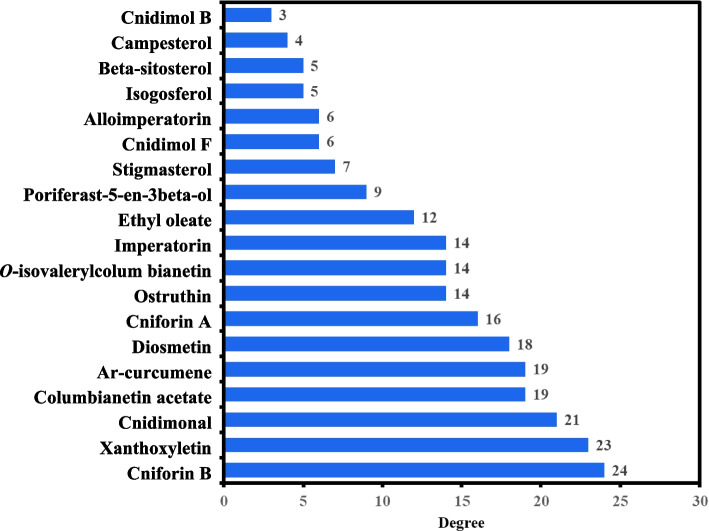
One more hub network was constructed between the 66 anti-AD core targets (Analysis of protein-protein interaction (PPI) section) and the 19 active compounds, as shown in Fig. 6b. The 66 anti-AD core targets were acted on by all the 19 active compounds. The 19 active compounds with respect to their degrees in the hub network are presented in the form of a bar graph in Fig. 7. Ranked by DC ≥ average value of 12.578, the top 10 active compounds (key active compounds; each has more than 13 targets) are cniforin B, xanthoxyletin, cnidimonal, columbianetin acetate, ar-curcumene, diosmetin, cniforin A, ostruthin, O-isovalerylcolum bianetin, and imperatorin (Fig. 7). The network shows that a single compound can interact with multiple targets, and that multiple compounds can interact with a single target. These findings confirm the complexity of the interactions between multiple targets and multiple active compounds in CF.
Fig. 7.
Bar graph of degree values of CF’s active compounds
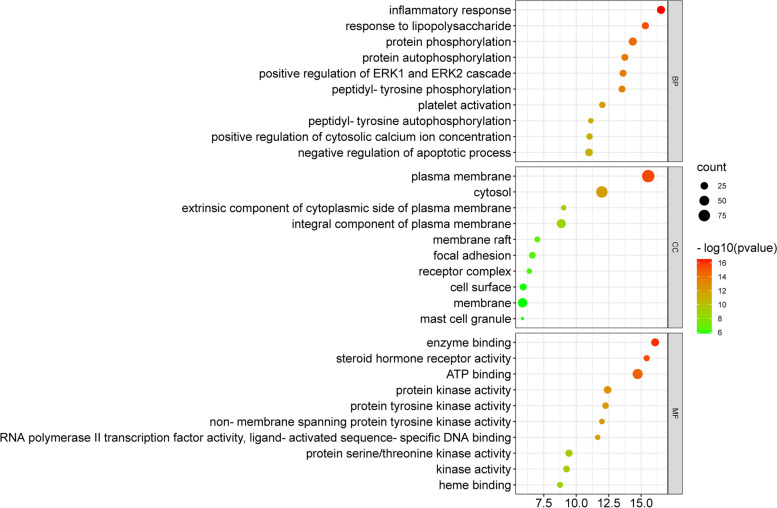
GO enrichment analysis
GO enrichment analysis was carried out to analyze the 176 anti-AD targets of CF. The respective top 10 enriched terms of BP, CC, and MF of the 176 targets are presented in Fig. 8. The results of GO enrichment analysis demonstrated that anti-AD targets of CF are involved in multiple biological processes, such as inflammatory response, response to lipopolysaccharides, protein phosphorylation, positive regulation of ERK1 and ERK2 cascades, and negative regulation of the apoptotic process. In the cellular component category, anti-AD targets of CF are mainly plasma membrane proteins, cytosol proteins and integral components of the plasma membrane. GO enrichment analysis results showed that the enriched molecular function ontologies are dominated by ATP binding, enzyme binding, proteins kinase activity, and protein serine/threonine kinase activity.
Fig. 8.
GO enrichment analysis for the 176 anti-AD targets of CF. X-axis presents the number of targets; Y-axis exhibits biological process (BP), cellular components (CC), and molecular function (MF)
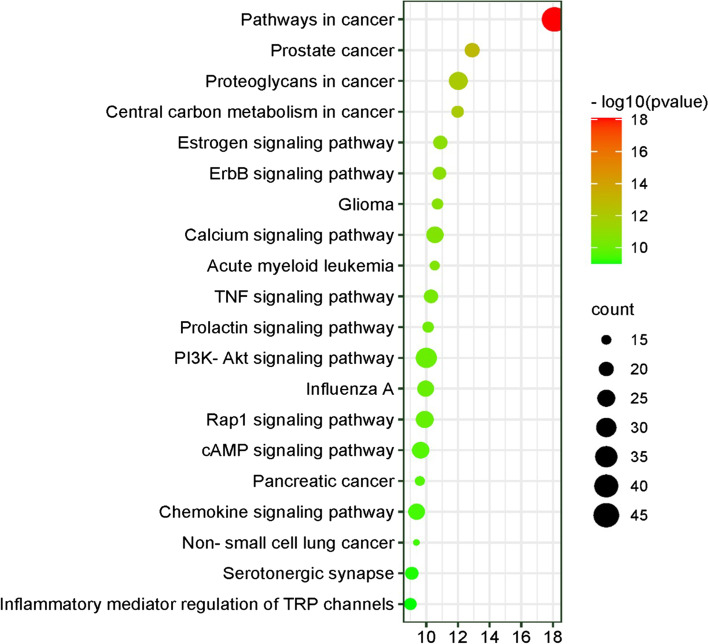
KEGG pathway analysis
KEGG pathway analysis was carried out to deduce the molecular mechanisms by which CF treats AD. A total of 96 pathways, each with a p-value < 0.05, were identified after uploading 176 anti-AD targets of CF to the DAVID platform. The top 20 significant KEGG pathways are presented in Fig. 9. Findings of the KEGG pathway enrichment revealed that anti-AD targets of CF appear to be mainly involved in PI3K-Akt signaling pathway, calcium signaling pathway, Rap1 signaling pathway, cAMP signaling pathway, chemokine signaling pathway, TNF signaling pathway, and inflammatory mediator regulation of TRP channels. These pathways appear likely to play roles in the molecular mechanisms of CF in treating AD.
Fig. 9.
KEGG pathway enrichment analysis for the 176 anti-AD targets of CF. X-axis displays the number of genes; Y-axis displays the various KEGG pathways. Bubble size indicates the number of genes participating in each KEGG pathway
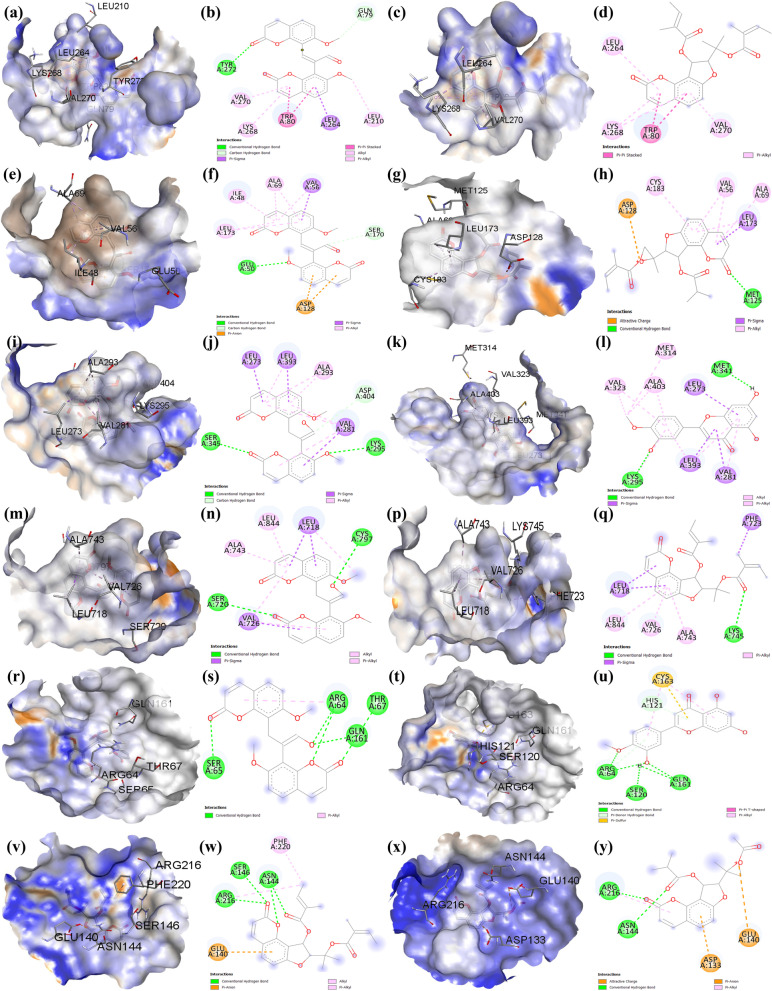
Molecular docking
Molecular docking of the key active compounds of CF with CF’s anti-AD core targets (AKT1, MAPK3, SRC, EGFR, CASP3 and PTGS2) was conducted. Results are presented in Table 2 and Fig. 10 (a-y).
Table 2.
Molecular docking of the key active compounds of CF with CF’s anti-AD core targets
| Molecule ID | Compound name | Binding energy (kcal/mol) | |||||
|---|---|---|---|---|---|---|---|
| AKT1 | MAPK3 | SRC | EGFR | CASP3 | PTGS2 | ||
| MOL003608 | Columbianetin acetate | -9.7 | -7.3 | -8.3 | -6.9 | -5.2 | -4.7 |
| MOL002881 | Diosmetin | -9.4 | -7.8 | -8.7 | -7.3 | -6.2 | -4.9 |
| MOL003584 | Xanthoxyletin | -9.8 | -7.4 | -8.3 | -6.9 | -5.3 | -4.4 |
| MOL003591 | Ar-curcumene | -10.5 | -7.8 | -8.4 | -8.3 | -6.1 | -5.1 |
| MOL003626 | Ostruthin | -9.5 | -7.6 | -7.8 | -6.7 | -5.1 | -4.1 |
| MOL003606 | Cniforin A | -9.7 | -7.6 | -8.4 | -7.2 | -5.2 | -5.0 |
| MOL003624 | O-isovalerylcolum Bianetin | -9.9 | -7.2 | -8.5 | -7.5 | -5.4 | -4.5 |
| MOL003607 | Cniforin B | -9.7 | -7.9 | -8.6 | -7.3 | -5.7 | -4.9 |
| MOL001941 | Imperatorin | -9.0 | -7.2 | -8.1 | -6.4 | -6.0 | -4.2 |
| MOL003605 | Cnidimonal | -10.8 | -8.1 | -8.7 | -8.1 | -6.2 | -5.0 |
Fig. 10.
Three D and two D molecular docking results. a & b Cnidimonal and (c & d) ar-curcumene bind AKT1. e & f Cnidimonal and (g & h) cniforin B bind MAPK3. i & j)Cnidimonal and (k & l) diosmetin bind SRC. m & n Cnidimonal and (p & q) ar-curcumene bind EGFR. r & s Cnidimonal and (t & u) diosmetin bind CASP3. v & w Ar-curcumene and (x & y) cniforin A bind PTGS2
Binding affinity between a compound and a protein is represented by bingding energy score. The lower the energy, the better the ligand-receptor protein binding is [11]. Docking results demonstrate that each of the key active compounds of CF binds AKT1, MAPK3, SRC, EGFR, CASP3, and PTGS2. These results suggest that the key active compounds of CF directly act on the anti-AD core targets AKT1, SRC, MAPK3, EGFR, CASP3, and PTGS2. The molecular docking findings were consistent with the network pharmacology screening, confirming the trustworthiness of network pharmacology in this study.
Discussion
The present study explored the active compounds and molecular mechanisms of CF in treating AD. AD is the most common inflammatory skin condition, and multiple signaling pathways potentially contribute to the disease's aetiology simultaneously.
Out of a total of 114 compounds, 19 active compounds with OB ≥ 30% and DL ≥ 0.18 were selected (Table 1) for intensive investigation. Most of the active compounds were found to be multitargeting. The network results demonstrate that ten compounds act on more than 13 anti-AD core targets; these are cniforin B, ar-curcumene, xanthoxyletin, ostruthin, cnidimonal, columbianetin acetate, diosmetin, cniforin A, O-isovalerylcolum bianetin, and imperatorin (Fig. 7). The ten compounds were regarded as key anti-AD compounds of CF. These compounds have satisfactory OB values, thus they are supposed to be orally effective. For treating AD, CF is traditionally used orally and/or topically [21, 22]. Whether the key active compounds of CF can be developed into oral and/or topical anti-AD medications warrants further studies.
The PPI analysis revealed that numerous genes are involved in CF’s effects in treating AD, including AKT1, MAPK3, SRC, EGFR, CASP3, and PTGS2. Reports have demonstrated that inhibiting AKT1 in the skin results in a shift in protease expression, a drop in filaggrin expression, and ultimately, the disintegration of the barrier function of the skin [11, 43]. IL-17 induces the activation of MAPKs that are implicated in the pathophysiology of inflammatory skin disorders [44, 45]. SRC plays a vital role in the activation and proliferation of T cells, leading to severe and chronic AD [46]. Chronic inflammatory skin diseases such as AD have also been associated with the upregulation of EGFR and its ligand expression. Recent research has shown that EGFR-targeted therapy protects against AD by reducing keratinocytes' IL-6 production in response to allergens [47, 48]. CASP3 is regarded as the principal executor and is involved not only in apoptosis pathways but also in inflammation, embryonic and hematopoietic stem cell differentiation. CASP3 plays an important role in keratinocyte apoptosis, which has been implicated as a fundamental cause of spongiosis in AD [49]. COX activity helps to maintain body homeostasis, and inducible COX-2 (PTGS2), in particular, seems to be involved in a number of pathological disorders, including inflammation and pain [50].
GO enrichment analysis demonstrated that compounds in CF may affect a variety of biological processes, including inflammatory response, response to lipopolysaccharides, protein phosphorylation, positive regulation of the ERK1 and ERK2 cascade, and negative regulation of the apoptotic process, all of which may be associated with its anti-AD effects (Fig. 8). Although apoptosis is necessary for cell renewal, excessive chemokines and cytokines produced by skin infection in patients with AD often result in considerable keratinocyte death [43]. Active compounds of CF have been shown to decrease apoptosis in AD, hence promoting keratinocyte regeneration [11, 47].
The KEGG pathway analysis results demonstrated that anti-AD key active compounds of CF act on several signaling pathways, including PI3K-Akt signaling pathway, calcium signaling pathway, Rap1 signaling pathway, cAMP signaling pathway, chemokine signaling pathway, TNF signaling pathway, and inflammatory mediator regulation of TRP channels (Fig. 9). PI3K-Akt signaling pathway dysregulation in the skin leads to a variety of clinical diseases characterized by uncontrolled cell proliferation, such as skin cancer, psoriasis, and AD [51]. Thus, suppressing the PI3K-Akt pathway may be a therapeutic option for AD. The dysregulation of the calcium signaling pathway has been reported to occur when AD is induced, as this pathway controls keratinocyte differentiation and skin barrier formation [52]. Regulating calcium can be another potential strategy in treating AD. TRP channels are regulated by inflammatory mediators and are implicated in the activation-induced release of pro-inflammatory cytokines from keratinocytes; hence, their inhibition may also be advantageous in treating AD [53]. Given that the role of TNF in the etiology of AD is well established [54], targeting TNF is a viable therapeutic strategy for AD. Molecular docking results further confirmed that key active compounds of CF had a regulatory impact on AD-related molecules, such as AKT1, SRC, MAPK3, EGFR, CASP3, and PTGS2.
Conclusions
The present study explored the compounds and molecular mechanisms active in the therapeutic application of CF to treat AD. In this research, 10 key active compounds of CF and 66 anti-AD core targets were identified. Our study revealed that the underlying mechanisms of anti-AD effects of CF are likely to involve inhibition of the inflammatory response, response to lipopolysaccharides, protein phosphorylation, negative regulation of apoptotic processes, and positive regulation of the ERK1 and ERK2 cascades. Further, we found that four key signaling pathways are likely to be involved: PI3K-Akt signaling pathway, calcium signaling pathway, Rap1 signaling pathway, and cAMP signaling pathway. Our results justify the conclusion that the anti-AD effects of CF might be due to the direct or indirect synergistic effects of multi-target and multi-pathway efforts. Molecular docking results showed that key active compounds of CF can potentially bind to AKT1, SRC, MAPK3, EGFR, CASP3, and PTGS2. Results of the present study establish a foundation for further investigation of the anti-AD compounds and mechanisms of CF and provide a basis for developing modern anti-AD agents based on compounds that occur in CF.
Acknowledgements
The authors are highly grateful to the School of Chinese Medicine, Hong Kong Baptist University, and the grants for supporting this research work.
Authors’ contributions
Conceptualization, ZL.Y.; XQ. F. and Y.W.; methodology, S.A.K.; XQ. F. and A.S.L.; software, S.A.K.; A.S.L. and XQ. F.; validation S.A.K. and ZL.Y.; formal analysis, S.A.K.; A.S.L. and Y.W.; investigation, S.A.K.; resources, XQ. F. and ZL.Y.; data curation, S.A.K.; A.S.L.; XQ. F. and ZL.Y.; writing—original draft preparation, S.A.K.; Y.W.; A.S.L.; XQ. F. and ZL.Y.; writing—review and editing, S.A.K.; Y.W.; A.S.L.; XQ. F. and ZL.Y.; visualization, S.A.K.; Y.W. and A.S.L.; supervision, XQ. F. and ZL.Y.; project administration, ZL.Y.; revision, Y.W.; XQ. F.; ZL.Y. and S.A.K.; funding acquisition, XQ. F. and ZL.Y. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by grants NSFC 81874358 and 82174029, 2021A1515010658, 2020A1515010579, and JCYJ20200109150719846.
Availability of data and materials
The datasets used and analysed during the current study available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no conflict of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Ying Wu, Email: 18482546@life.hkbu.edu.hk.
Xiu-Qiong Fu, Email: makyfu@hkbu.edu.hk.
Zhi-Ling Yu, Email: zlyu@hkbu.edu.hk.
References
- 1.Ständer S. Atopic Dermatitis. N Engl J Med. 2021;384:1136–1143. doi: 10.1056/NEJMra2023911. [DOI] [PubMed] [Google Scholar]
- 2.Ring J. Terminology of Allergic Phenomena. Chem Immunol Allergy. 2014;100:46–52. doi: 10.1159/000358500. [DOI] [PubMed] [Google Scholar]
- 3.Nutten S. Atopic Dermatitis: Global Epidemiology and Risk Factors. Ann Nutr Metab. 2015;66(Suppl. 1):8–16. doi: 10.1159/000370220. [DOI] [PubMed] [Google Scholar]
- 4.Asher MI, Montefort S, Björkstén B, Lai CK, Strachan DP, Weiland SK, et al. Worldwide time trends in the prevalence of symptoms of asthma, allergic rhinoconjunctivitis, and eczema in childhood: ISAAC Phases One and Three repeat multicountry cross-sectional surveys. Lancet. 2006;368:733–743. doi: 10.1016/S0140-6736(06)69283-0. [DOI] [PubMed] [Google Scholar]
- 5.McKenzie C, Silverberg JI. The prevalence and persistence of atopic dermatitis in urban United States children. Ann Allergy, Asthma Immunol. 2019;123:173–178.e1. doi: 10.1016/j.anai.2019.05.014. [DOI] [PubMed] [Google Scholar]
- 6.Laughter MR, Maymone MBC, Mashayekhi S, Arents BWM, Karimkhani C, Langan SM, et al. The global burden of atopic dermatitis: lessons from the Global Burden of Disease Study 1990–2017*. Br J Dermatol. 2021;184:304–309. doi: 10.1111/bjd.19580. [DOI] [PubMed] [Google Scholar]
- 7.The Complete Guide to Eczema in Hong Kong | Healthy Matters. https://www.healthymatters.com.hk/eczema-in-hong-kong-causes-symptoms-treatment/. Accessed 21 Dec 2021.
- 8.“Seeing The Invisible” – Hong Kong’s first community-wide program for children and families affected by childhood eczema - All News - Media - HKU. https://www.hku.hk/press/news_detail_16241.html. Accessed 21 Dec 2021.
- 9.Cheng NS, Chau PCJ, Hon KLE, Choi KC, Kung JSC, Ng WG, et al. Measuring the quality of life of the families of children with eczema in Hong Kong. Asia Pac Allergy. 2019;9:e26. doi: 10.5415/apallergy.2019.9.e26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Boguniewicz M, Leung DYM. Atopic dermatitis: a disease of altered skin barrier and immune dysregulation. Immunol Rev. 2011;242:233–246. doi: 10.1111/j.1600-065X.2011.01027.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chu M, Tsang MSM, He R, Lam CWK, Quan ZB, Wong CK. The Active Compounds and Therapeutic Mechanisms of Pentaherbs Formula for Oral and Topical Treatment of Atopic Dermatitis Based on Network Pharmacology. Plants. 2020;9:1166. doi: 10.3390/plants9091166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Furue M, Chiba T, Tsuji G, Ulzii D, Kido-Nakahara M, Nakahara T, et al. Atopic dermatitis: immune deviation, barrier dysfunction, IgE autoreactivity and new therapies. Allergol Int. 2017;66:398–403. doi: 10.1016/j.alit.2016.12.002. [DOI] [PubMed] [Google Scholar]
- 13.Langan SM, Irvine AD, Weidinger S. Atopic dermatitis. Lancet. 2020;396:345–360. doi: 10.1016/S0140-6736(20)31286-1. [DOI] [PubMed] [Google Scholar]
- 14.Jiao D, Wong CK, Qiu HN, Dong J, Cai Z, Chu M, et al. NOD2 and TLR2 ligands trigger the activation of basophils and eosinophils by interacting with dermal fibroblasts in atopic dermatitis-like skin inflammation. Cell Mol Immunol 2016 134. 2015;13:535–50. [DOI] [PMC free article] [PubMed]
- 15.Liu FT, Goodarzi H, Chen HY. IgE, mast cells, and eosinophils in atopic dermatitis. Clin Rev Allergy Immunol. 2011;41:298–310. doi: 10.1007/s12016-011-8252-4. [DOI] [PubMed] [Google Scholar]
- 16.Alexander T, Maxim E, Cardwell LA, Chawla A, Feldman SR. Prescriptions for atopic dermatitis: oral corticosteroids remain commonplace. J Dermatolog Treat. 2017;29:238–240. doi: 10.1080/09546634.2017.1365112. [DOI] [PubMed] [Google Scholar]
- 17.Williams HC. Atopic Dermatitis. N Engl J Med. 2009;352:2314–2324. doi: 10.1056/NEJMcp042803. [DOI] [PubMed] [Google Scholar]
- 18.Ormerod AD. Topical tacrolimus and pimecrolimus and the risk of cancer: how much cause for concern? Br J Dermatol. 2005;153:701–705. doi: 10.1111/j.1365-2133.2005.06899.x. [DOI] [PubMed] [Google Scholar]
- 19.Nghiem P, Pearson G, Langley RG. Tacrolimus and pimecrolimus: From clever prokaryotes to inhibiting calcineurin and treating atopic dermatitis. J Am Acad Dermatol. 2002;46:228–241. doi: 10.1067/mjd.2002.120942. [DOI] [PubMed] [Google Scholar]
- 20.Ashcroft DM, Dimmock P, Garside R, Stein K, Williams HC. Efficacy and tolerability of topical pimecrolimus and tacrolimus in the treatment of atopic dermatitis: meta-analysis of randomised controlled trials. BMJ. 2005;330:516. doi: 10.1136/bmj.38376.439653.D3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chinese Pharmacopoeia. http://wp.chp.org.cn/front/chpint/en/. Accessed 4 Jan 2022.
- 22.Li YM, Jia M, Li HQ, Zhang ND, Wen X, Rahman K, et al. Cnidium monnieri: A Review of Traditional Uses, Phytochemical and Ethnopharmacological Properties. Am J Chin Med. 2015;43:835–877. doi: 10.1142/S0192415X15500500. [DOI] [PubMed] [Google Scholar]
- 23.Gao F, Hu Y, Ye X, Li J, Chen Z, Fan G. Optimal extraction and fingerprint analysis of Cnidii fructus by accelerated solvent extraction and high performance liquid chromatographic analysis with photodiode array and mass spectrometry detections. Food Chem. 2013;141:1962–1971. doi: 10.1016/j.foodchem.2013.05.013. [DOI] [PubMed] [Google Scholar]
- 24.Sun Y, Yang AWH, Lenon GB. Phytochemistry, Ethnopharmacology, Pharmacokinetics and Toxicology of Cnidium monnieri (L.) Cusson. Int J Mol Sci. 2020;21:1006. doi: 10.3390/ijms21031006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yu Z, Deng T, Wang P, Sun T, Xu Y. Ameliorative effects of total coumarins from the fructus of Cnidium monnieri (L.) Cuss. on 2,4-dinitrochlorobenzene-induced atopic dermatitis in rats. Phyther Res. 2021;35:3310–24. doi: 10.1002/ptr.7052. [DOI] [PubMed] [Google Scholar]
- 26.Luo TT, Lu Y, Yan SK, Xiao X, Rong X lu, Guo J. Network Pharmacology in Research of Chinese Medicine Formula: Methodology, Application and Prospective. Chinese J Integr Med 2019 261. 2019;26:72–80. [DOI] [PubMed]
- 27.Ru J, Li P, Wang J, Zhou W, Li B, Huang C, et al. TCMSP: A database of systems pharmacology for drug discovery from herbal medicines. J Cheminform. 2014;6:1–6. doi: 10.1186/1758-2946-6-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wang CR, Chen HW, Li Y, Zhou MY, Wong VKW, Jiang ZH, et al. Network Pharmacology Exploration Reveals Anti-Apoptosis as a Common Therapeutic Mechanism for Non-Alcoholic Fatty Liver Disease Treated with Blueberry Leaf Polyphenols. Nutr. 2021;13:4060. doi: 10.3390/nu13114060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ma X, Wu J, Liu C, Li J, Dong S, Zhang X, et al. Deciphering of Key Pharmacological Pathways of Poria Cocos Intervention in Breast Cancer Based on Integrated Pharmacological Method. Evid Based Complement Altern Med. 2020;2020:4931531. doi: 10.1155/2020/4931531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chen ML, Shah V, Patnaik R, Adams W, Hussain A, Conner D, et al. Bioavailability and bioequivalence: an FDA regulatory overview. Pharm Res. 2001;18(12):1645–50. doi: 10.1023/A:1013319408893. [DOI] [PubMed] [Google Scholar]
- 31.Daina A, Michielin O, Zoete V. SwissTargetPrediction: updated data and new features for efficient prediction of protein targets of small molecules. Nucleic Acids Res. 2019;47:W357–W364. doi: 10.1093/nar/gkz382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rebhan M, Chalifa-Caspi V, Prilusky J, Lancet D. GeneCards: integrating information about genes, proteins and diseases. Trends Genet. 1997;13:163. doi: 10.1016/S0168-9525(97)01103-7. [DOI] [PubMed] [Google Scholar]
- 33.von Mering C, Huynen M, Jaeggi D, Schmidt S, Bork P, Snel B. STRING: a database of predicted functional associations between proteins. Nucleic Acids Res. 2003;31:258–261. doi: 10.1093/nar/gkg034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lopes CT, Franz M, Kazi F, Donaldson SL, Morris Q, Bader GD, et al. Cytoscape Web: an interactive web-based network browser. Bioinformatics. 2010;26:2347–2348. doi: 10.1093/bioinformatics/btq430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zhang YZ, Yang JY, Wu RX, Fang C, Lu H, Li HC, et al. Network Pharmacology-Based Identification of Key Mechanisms of Xihuang Pill in the Treatment of Triple-Negative Breast Cancer Stem Cells. Front Pharmacol. 2021;12:2582. doi: 10.3389/fphar.2021.714628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kanehisa M, Goto S. KEGG: kyoto encyclopedia of genes and genomes. Nucleic Acids Res. 2000;28:27–30. doi: 10.1093/nar/28.1.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Huang DW, Sherman BT, Lempicki RA. Systematic and integrative analysis of large gene lists using DAVID bioinformatics resources. Nat Protoc 2009 41. 2008;4:44–57. [DOI] [PubMed]
- 38.Berman HM, Westbrook J, Feng Z, Gilliland G, Bhat TN, Weissig H, et al. The Protein Data Bank. Nucleic Acids Res. 2000;28:235–242. doi: 10.1093/nar/28.1.235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.BIOVIA DS. BIOVIA discovery studio visualizer. 2016. 20:779.
- 40.Grosdidier A, Zoete V, Michielin O. Fast docking using the CHARMM force field with EADock DSS. J Comput Chem. 2011;32:2149–2159. doi: 10.1002/jcc.21797. [DOI] [PubMed] [Google Scholar]
- 41.Trott O, Olson AJ. AutoDock Vina: Improving the speed and accuracy of docking with a new scoring function, efficient optimization, and multithreading. J Comput Chem. 2010;31:455–461. doi: 10.1002/jcc.21334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Liu Y, Zhang J, Liu X, Zhou W, Stalin A, Fu C, et al. Investigation on the mechanisms of guiqi huoxue capsule for treating cervical spondylosis based on network pharmacology and molecular docking. Medicine (Baltimore) 2021;100:e26643. doi: 10.1097/MD.0000000000026643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Trautmann A, Akdis M, Schmid-Grendelmeier P, Disch R, Bröcker E-B, Blaser K, et al. Targeting keratinocyte apoptosis in the treatment of atopic dermatitis and allergic contact dermatitis. J Allergy Clin Immunol. 2001;108:839–846. doi: 10.1067/mai.2001.118796. [DOI] [PubMed] [Google Scholar]
- 44.Johansen C, Kragballe K, Westergaard M, Henningsen J, Kristiansen K, Iversen L. The mitogen-activated protein kinases p38 and ERK1/2 are increased in lesional psoriatic skin. Br J Dermatol. 2005;152:37–42. doi: 10.1111/j.1365-2133.2004.06304.x. [DOI] [PubMed] [Google Scholar]
- 45.Tan Q, Yang H, Liu E, Wang H. P38/ERK MAPK signaling pathways are involved in the regulation of filaggrin and involucrin by IL-17. Mol Med Rep. 2017;16:8863. doi: 10.3892/mmr.2017.7689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Takayama T, Takaoka A, Takahashi S, Takahashi A, Umemiya H, Sato M. Effects of the novel and potent lymphocyte-specific protein tyrosine kinase inhibitor TKM0150 on mixed lymphocyte reaction and contact hypersensitivity in mice. Arzneimittel-Forschung/Drug Res. 2010;60:282–285. doi: 10.1055/s-0031-1296286. [DOI] [PubMed] [Google Scholar]
- 47.Wong WJ, Richardson T, Seykora JT, Cotsarelis G, Simon MC. Hypoxia-Inducible Factors Regulate Filaggrin Expression and Epidermal Barrier Function. J Invest Dermatol. 2015;135:454–461. doi: 10.1038/jid.2014.283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Pastore S, Mascia F, Mariani V, Girolomoni G. The Epidermal Growth Factor Receptor System in Skin Repair and Inflammation. J Invest Dermatol. 2008;128:1365–1374. doi: 10.1038/sj.jid.5701184. [DOI] [PubMed] [Google Scholar]
- 49.Simon D, Lindberg RLP, Kozlowski E, Braathen LR, Simon HU. Epidermal caspase-3 cleavage associated with interferon-γ-expressing lymphocytes in acute atopic dermatitis lesions. Exp Dermatol. 2006;15:441–446. doi: 10.1111/j.0906-6705.2006.00428.x. [DOI] [PubMed] [Google Scholar]
- 50.Sugimoto M, Arai I, Futaki N, Hashimoto Y, Honma Y, Nakaike S. COX-1 inhibition enhances scratching behaviour in NC/Nga mice with atopic dermatitis. Exp Dermatol. 2006;15:582–588. doi: 10.1111/j.1600-0625.2006.00447.x. [DOI] [PubMed] [Google Scholar]
- 51.Mercurio L, Albanesi C, Madonna S. Recent Updates on the Involvement of PI3K/AKT/mTOR Molecular Cascade in the Pathogenesis of Hyperproliferative Skin Disorders. Front Med. 2021;8:665647. doi: 10.3389/fmed.2021.665647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Lee SE, Lee SH. Skin Barrier and Calcium. Ann Dermatol. 2018;30:265–275. doi: 10.5021/ad.2018.30.3.265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Tõth BI, Oláh A, Szöllósi AG, Bírõ T. TRP channels in the skin. Br J Pharmacol. 2014;171:2568–2581. doi: 10.1111/bph.12569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Montes-Torres A, Llamas-Velasco M, Pérez-Plaza A, Solano-López G, Sánchez-Pérez J. Biological Treatments in Atopic Dermatitis. J Clin Med. 2015;4:593–613. doi: 10.3390/jcm4040593. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and analysed during the current study available from the corresponding author on reasonable request.