Figure 2. Association Between Platelet Transfusion–Associated Outcomes and Platelet Count at the Time of Platelet Transfusion.
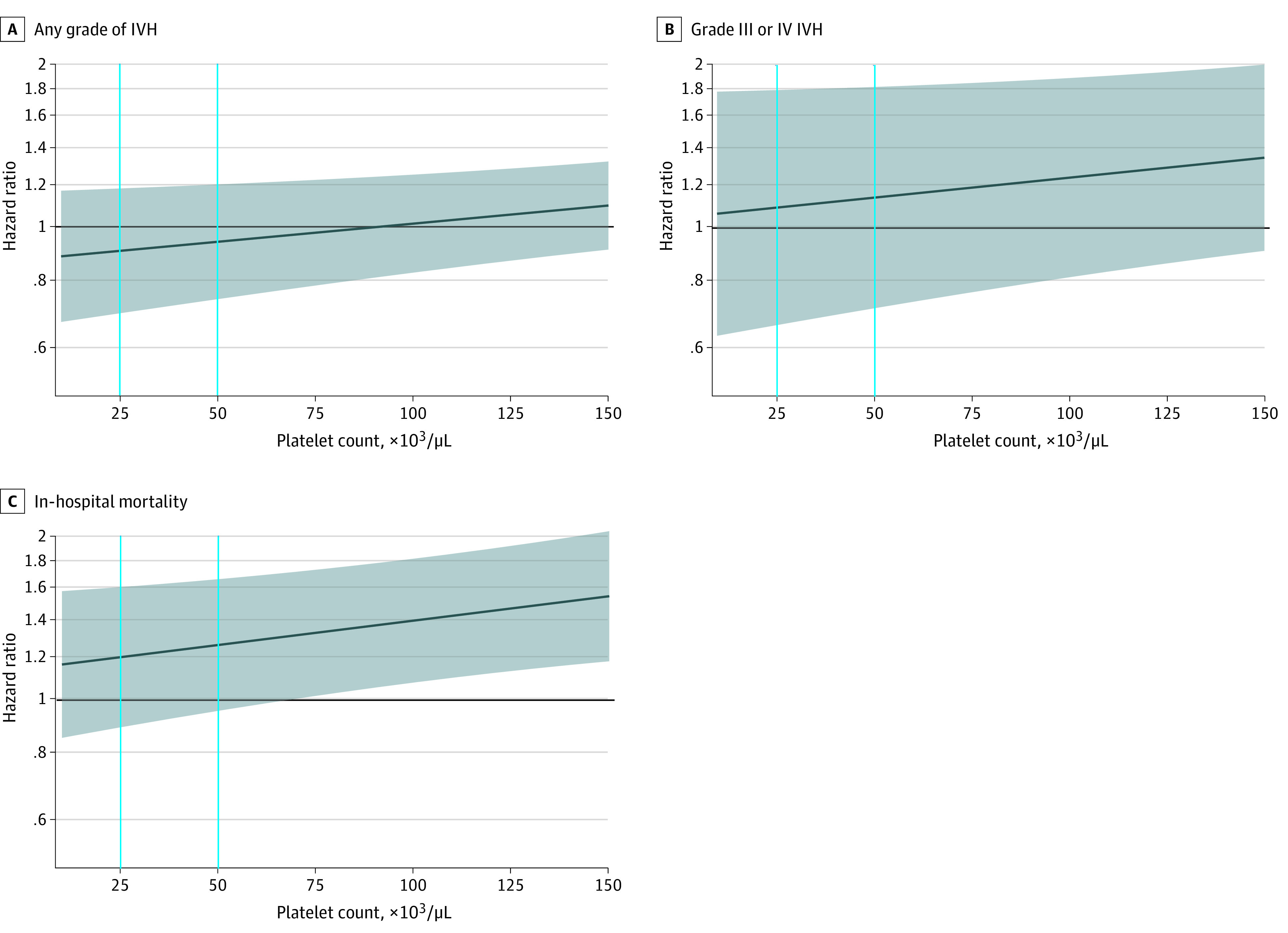
The dark blue line represents the hazard ratio, and the shaded area represents the 95% CI. The horizontal black line indicates a hazard ratio of 1.00. Vertical lines indicate platelet count values of 25 × 103 /μL and 50 × 103/μL (to convert to ×109 per liter, multiply by 1). A and B, Hazard ratios were estimated by the Fine-Gray subdistribution hazard model to account for the competing risk of death. C, The Cox proportional hazards model was used to estimate the hazard ratio. In all models, platelet count was included as a time-varying variable, which was defined as the most recent result at least 1 day prior to the outcome event. The interaction term between platelet count and platelet transfusion was included in all models, so the hazard ratio represents the risk change for every additional platelet transfusion at a certain platelet count level. The quadratic term of platelet count was added to the model of any grade IVH, and quadratic and cubic terms were added to the model of in-hospital mortality because they were statistically significant. Infant sex, birth weight strata, gestational age strata, congenital disorder, singleton, any Apgar score of 7 or lower (ie, 1-minute, 5-minute, or 10-minute Apgar), cesarean delivery, maternal preeclampsia, pregnancy-induced hypertension, antenatal steroids given, intrauterine distress, maternal high-risk pregnancy, and premature rupture of membrane were adjusted as time-constant covariates; first ventilation time after birth and the sepsis/necrotizing enterocolitis occurrence time after birth were adjusted as time-varying covariates.
