This cross-sectional study compares the number of men and women surgeons who received research funding from the National Institutes of Health from 2010 to 2020 and the total grant funding they received.
Key Points
Question
What is the current status of National Institutes of Health (NIH) research funding for women surgeon-scientists?
Findings
In this cross-sectional study, the number of women surgeon-scientists who received NIH research funds and the amounts awarded to them increased from 2010 to 2020. However, in 2020, disparities remained in the proportion of women in the surgical workforce (27%) compared with those who received research funding from the NIH (25%) and the total grant amounts (22%) awarded to them.
Meaning
Results of this study suggest that more academic opportunities need to be created for women surgeon-scientists to narrow the existing gap in research funding between men and women.
Abstract
Importance
Women have made substantial advancements in academic surgery, but research funding disparities continue to hamper their progress, and current literature on the status of National Institutes of Health (NIH) funding awarded to women surgeon-scientists appears to be conflicting.
Objective
To examine gender-based differences in NIH funding awarded to surgeon-scientists by comparing total grant amounts awarded and the distribution of grants by gender and research type.
Design, Setting, and Participants
This cross-sectional study was performed using a previously created database of NIH-funded surgeons from 2010 to 2020. Active physician data from the Association of American Medical Colleges were used to calculate total surgeon populations. This study was performed at the NIH using the NIH internal data platform, iSearch Grants. A total of 715 men and women surgeon-scientists funded by the NIH in 2010 and 1031 funded in 2020 were included in the analysis.
Main Outcomes and Measures
The main outcome was the number of women among the total number of surgeons who received NIH grants and the total grant amounts awarded to them. Bivariate χ2 analyses were performed using population totals and substantiated by z tests of population proportions.
Results
This study included 715 physicians (n = 579 men [81.0%]) in 2010 and 1031 physicians (n = 769 men [74.6%]) in 2020. In 2020, women comprised 27.4% of the surgical workforce and 25.4% of surgeons with research funding in the US, but they received only 21.7% of total NIH research funding awarded to all surgeons. The number of funded women surgeon-scientists, however, significantly increased from 2010 to 2020 (262 [25.4%] in 2020 vs 136 [19.0%] in 2010; P < .001) as did their funding ($189.7 million [21.7%] in 2020 vs $75.9 million [12.3%] in 2010; P < .001). Furthermore, the proportion of US women surgeons overall with NIH funding significantly increased in 2020 vs 2010 (0.7% vs 0.5%; P < .001). Basic science, clinical outcomes, and clinical trial R01 grants also increased among women surgeon-scientists. Women and men K grant holders had a similar mean (SD) number of R01 application attempts before success (2.7 [3.01] vs 2.3 [3.15]; P = .60) and similar K-to-R award conversion rates (23.5% vs 26.7%; P = .55).
Conclusions and Relevance
This cross-sectional study found an increasing number of women surgeon-scientists receiving NIH funding in 2020 vs 2010 as well as increases in the median grant amounts awarded. Although these results are promising, a discrepancy remains in the proportion of women in the surgical workforce compared with those funded by the NIH and the total grant amounts awarded to them.
Introduction
Funding disparities among different groups have garnered attention in recent years. However, current literature on the representation of women among funded surgeon-scientists in the US is conflicting, with disparate claims indicating either a persistently wide gender-based gap in funding or parity for men and women.1,2,3
Several studies have reported gender-based disparities in research funding throughout academic medicine. Some studies found that women were evaluated less favorably as principal investigators (PIs) than men and, as first-time PIs, received less National Institutes of Health (NIH) funding per grant.4,5 Similar findings have been reported for surgical specialties.6,7,8 For instance, Eloy et al7 reported that men PIs in otolaryngology received higher mean NIH funding compared with women ($498 593 vs $359 276).
In contrast, a study analyzing the patterns of NIH funding in general surgery using the NIH Research Portfolio Online Reporting Tools Expenditures and Results (RePORTER) found no significant difference in the number of grants awarded to men vs women.9 Another study reported an overrepresentation of women among surgeon-scientists with R01 funding in 2018.2 However, most studies use RePORTER as their primary database, which is limited to searching for investigators by department only. As such, this limitation may result in the inclusion of nonsurgeons while excluding surgeons who belong to surgical specialties not represented in the RePORTER, such as cardiothoracic or vascular surgery.10
To address these inconsistencies, we used data from a database of National Institutes of Health (NIH)–funded surgeon-scientists to analyze the representation of women among women surgeons with NIH research funding10 and compared total grant amounts awarded stratified by gender distribution of grant awards and by research type (basic science, clinical outcomes, clinical trials research). We compared the number of attempts made by men and women surgeons who held K grants (research career development awards) in obtaining their first R grants (research grants). We also examined the rate of conversion of career development K-series awards to R01 grants (research grants awarded to a named investigator in an area representing the specific interest to support a discrete, specified, circumscribed project). In addition, to identify differences in maintenance of NIH research funding, we evaluated the number of PIs who maintained continuous NIH funding from 2010 to 2020.
Methods
Data Sources
In this cross-sectional study, a previously created database, using the NIH internal data platform iSearch Grants, version 2.4 (NIH Office of Portfolio Analysis’s next-generation portfolio analysis platform), was queried to identify all surgeon-scientists with NIH grants active in either June 2010 or June 2020.10 The following data were extracted: PI name, grant activity code, grant number, total grant amount, and number of R01 applications for K grant holders. Information on the gender of the PI was obtained by querying faculty web pages of academic institutions. The National Institutes of Health Institutional Review Board deemed the study exempt from review and waived the requirement for informed consent because a public database was used in this study. We followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline.
By searching NIH biosketches of PIs, we ensured that we captured all NIH-funded surgeons and excluded nonsurgeons. Furthermore, we used data from the Association of American Medical Colleges (AAMC) on the total surgeon workforce to obtain an accurate representation of the proportion of funded men and women. The total number of active physicians by gender in surgical specialties was obtained using the AAMC’s Physician Specialty Data Reports for 2008 and 2018, which were used as a surrogate for 2010 and 2020, respectively, as AAMC data reports are published every 2 years but were not available for 2010.11 These data were used to calculate the percentage of funded surgeon-scientists.
Total Grant Awards for Men vs Women Surgeon-Scientists by Research Type
Total grant amounts were calculated for men vs women for June 2010 and June 2020, and the total proportions were compared. For career development awards, the number and proportion of K-series grants were stratified by gender and compared between 2010 and 2020.
The K08, K23, and R01 grants were classified as basic science, clinical outcomes, and clinical trials. The proportion of K and R grants held by men vs women and the total grant amounts awarded per category were compared. In addition, the median grant amounts awarded to each PI for K08, K23, and R01 grants in each category were compared.
Application Success Rates, Conversion Rates, and Funding Longevity
The 2010 surgeon database was queried for all PIs holding K grants. The number of applications submitted for the first R01 grant was identified for each surgeon. Conversion rates of all NIH K-series grants identified in 2010 to R01 grants were calculated and compared.
Continuity of NIH funding for men and women surgeon-scientists with R01 grants was ascertained by identifying R01 grant holders who had funding in both 2010 and 2020. The status of all PIs with R01 grants in 2010 who did not maintain funding until 2020 was verified using a web search and online faculty profiles to exclude all PIs who had retired or were deceased.
Statistical Analysis
Data were expressed as number of PIs, total grant amounts awarded, and amount per grant awarded to individual PIs. The analyses were stratified by gender, assessment year, and grant type (K or R) or type of research (basic science, clinical outcomes, clinical trials). Bivariate χ2 analyses were performed using the number of PIs, total funding, and median grant amount. Kruskal-Wallis test and analysis of variance were performed for grant amount analyses. The z tests of the proportions of PIs and total awarded grant amounts in 2020 stratified by gender were performed using the proportions from 2010 as the null hypotheses. The t test was used to compare the number of attempts to convert from a K to an R award for women vs men. A consumer price index inflation–adjusted analysis was also performed for total grant amounts and median grant amounts using the online Consumer Price Index inflation calculator provided by the US Bureau of Labor Statistics.12 Statistical analyses were performed using JMP, version 14.0.0 (SAS Institute Inc). A 2-tailed P < .05 was considered to be statistically significant.
Results
Gender-Based Patterns
In 2010, of the NIH-funded surgeon population (n = 715), 579 were men (81.0%) and 136 were women (19.0%). In 2020, of the NIH-funded surgeon population (n = 1031), 769 were men (74.6%) and 262 were women (25.4%). A significant increase was observed in the proportion of women from 2010 to 2020 (19.0% vs 25.4%; P < .001) (Table). According to AAMC data, women comprised 27.4% of the surgeon workforce in 2020.
Table. National Institutes of Health–Funded Surgeon Portfolio Stratified by Gender, 2010 vs 2020.
| 2010 | 2020 | P value | |
|---|---|---|---|
| All surgeons | |||
| Total amount awarded in millions, $ | 614.7 | 872.4 | NA |
| No. of funded surgeons | 715 | 1031 | |
| Proportion of funded surgeonsa | 0.5 | 0.7 | |
| Men | |||
| Total amount awarded in millions (%), $ | 538.8 (87.7) | 682.7 (78.3) | <.001 |
| No. of funded surgeons (%) | 579 (81.0) | 769 (74.6) | |
| Proportion of funded surgeonsa | 0.5 | 0.7 | |
| Women | |||
| Total amount awarded in millions (%), $ | 75.9 (12.3) | 189.7 (21.7) | <.001 |
| No. of funded surgeons (%) | 136 (19.0) | 262 (25.4) | |
| Proportion of funded surgeonsa | 0.5 | 0.7 | |
Abbreviation: NA, not applicable.
Based on 2008 and 2018 Association of American Medical Colleges active physician data. The proportion of funded surgeons was taken from the total number of surgeons in the US in each category.
In the US, 136 women surgeon-scientists (0.5%) had NIH funding in 2010. In 2020, the proportion of women surgeon-scientists with funding increased to 0.7% (P < .001) (Table). A similar pattern was observed in men from 2010 (0.5%) to 2020 (0.7%; P < .001); however, the total number of men surgeon-scientists in the US declined from 114 765 in 2010 to 105 073 in 2020.
Total Grant Amounts and Career Development Awards
In 2010, women held $75.9 million (12.3%) of the $614.7 million total grant amounts awarded to surgeon-scientists, whereas men held $538.8 million (87.7%) (Table). In 2020, total grant amounts held by both women ($189.7 million [21.7%]) and men ($682.7 million [78.3%]) increased to $872.4 million; the increases for both men and women were statistically significant (P < .001). The total grant amounts in 2010 were adjusted for inflation ($89.6 million held by women; $635.8 million held by men), and the increase from 2010 to 2020 remained statistically significant after adjustment for inflation (P < .001).
In 2010, 90 surgeon-scientists held K awards: 29 were held by women (32.2%) and 61 by men (67.8%). In 2020, the number of surgeon-scientists increased to 172: 58 women (33.7%) and 114 men (66.3%; P = .67). This increase was not found to be statistically significant because the gender distribution remained stable over time.
Research Types
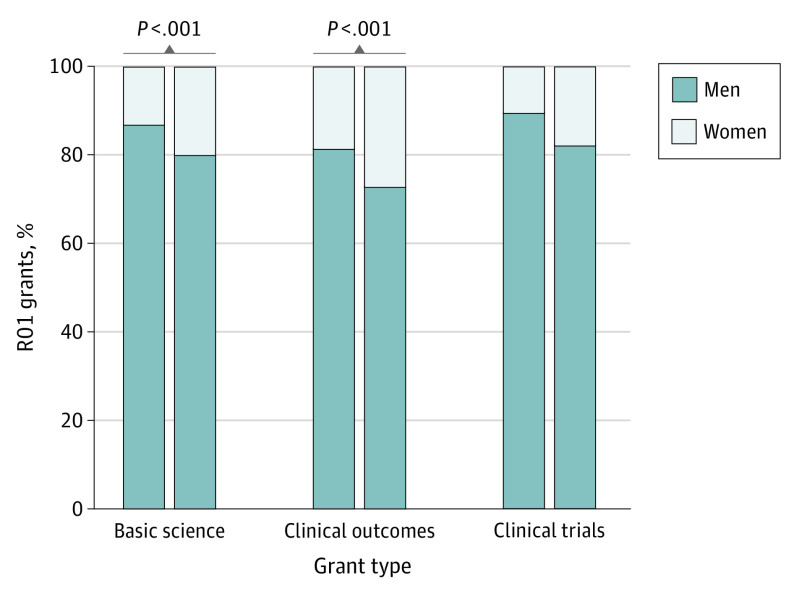
From 2010 to 2020, the proportion of R01 grants held by women in basic science, clinical outcomes, and clinical trials categories increased compared with men (Figure 1). The number of basic science grants increased from 370 to 466: 13.2% held by women in 2010 and 20.2% in 2020 (P < .001). The number of clinical outcomes grants increased from 78 to 126: 19.2% held by women in 2010 and 27.0% in 2020 (P < .001). The number of clinical trial grants also increased from 19 to 50, with 10.5% of these grants held by women in 2010 vs 18.0% in 2020 (P = .08); this increase was not statistically significant.
Figure 1. R01 Grants by Research Type and Principal Investigator Gender, 2010 vs 2020.
P values were calculated for the increase from 2010 to 2020.
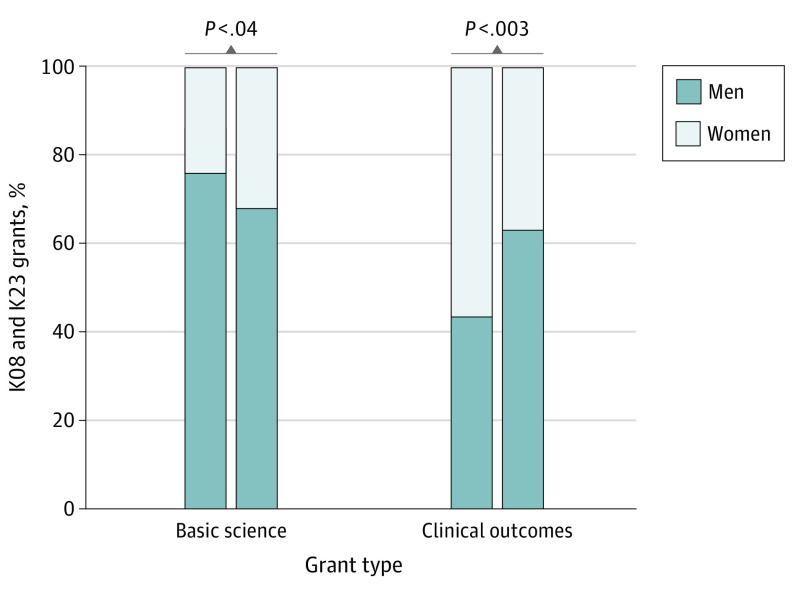
Analysis of K08 and K23 research grants revealed that the proportion of basic science grants held by women increased from 2010 to 2020 compared with men, whereas the proportion of clinical outcomes grants held by women decreased (Figure 2). The total number of basic science grants increased from 67 to 115. Women held 23.9% of the grants (16 of 67) in 2010 and 32.2% (37 of 115) in 2020, with a corresponding decrease from 76.1% (51 of 67) in 2010 to 67.8% (78 of 115) in 2020 for men (P = .04). The total number of clinical outcomes grants increased from 23 in 2010 to 57 in 2020. Women held 56.5% of clinical outcomes grants (13 of 23) in 2010 and just 36.8% (21 of 57) in 2020, with a corresponding increase from 43.5% (10 of 23) in 2010 to 63.2% (36 of 57) in 2020 for men (P = .003).
Figure 2. K08 and K23 Grants by Research Type and Principal Investigator Gender, 2010 vs 2020.
P values were calculated for the increase from 2010 to 2020.
Gender-Based Differences in Median Grant Amounts Awarded to PIs Based on Research Type
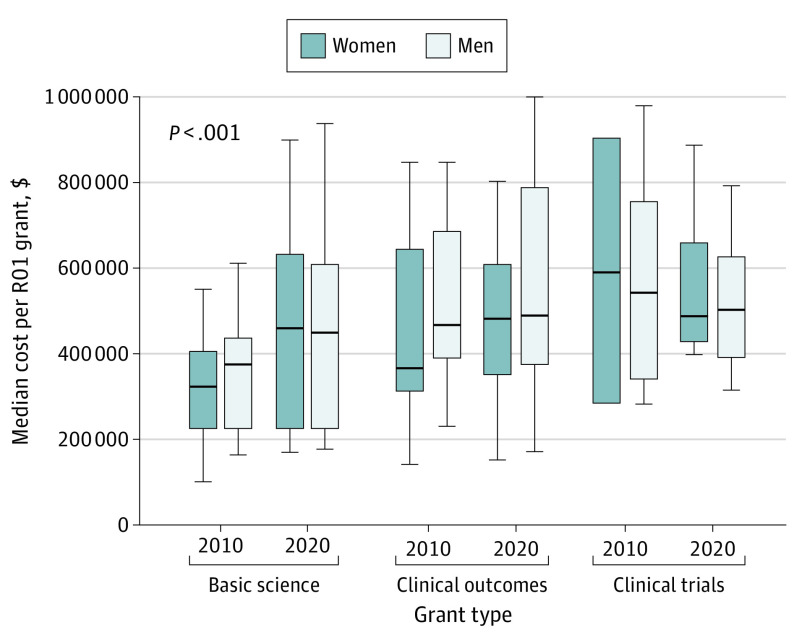
Analysis of the median total grant cost awarded to PIs for R01 basic science, clinical outcomes, and clinical trial research grants (Figure 3) found that in 2010, women were awarded a median (IQR) $318 258 ($275 058-$403 750) per basic science grant, whereas men were awarded $369 702 ($312 562-$431 493) per grant. The median (IQR) total grant amount increased for both women and men in 2020 (women, $456 543 [$366 517-$631 185]; men, $446 886 [$365 663-$604 548]; P < .001). There was no statistically significant difference between men and women in the median total grant amount awarded in clinical outcomes and clinical trials categories over time (Figure 3). The results were the same when adjusted for inflation.
Figure 3. Median Amount per R01 Grant by Research Type and Principal Investigator Gender, 2010 vs 2020.
The P value was calculated for the increase from 2010 to 2020.
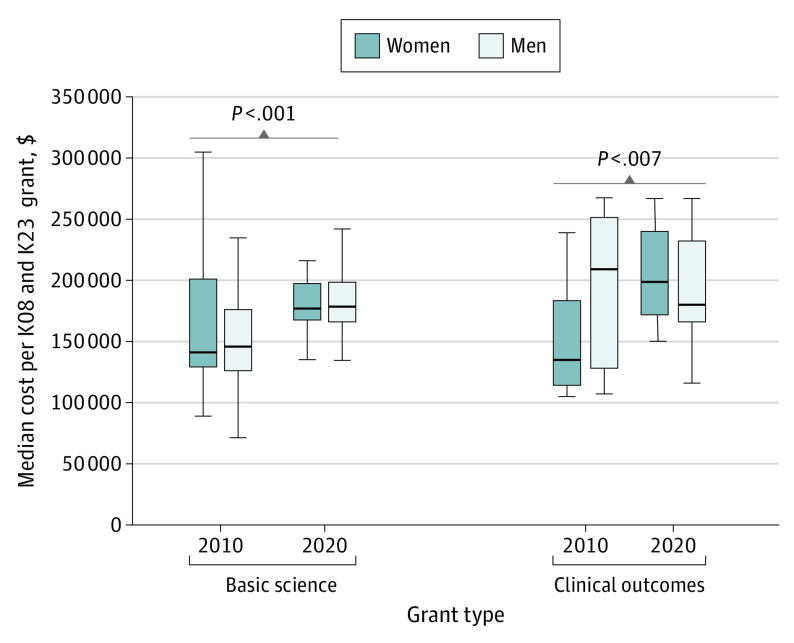
Similarly, the median total cost per grant for men and women calculated for all K08 and K23 grants (Figure 4) revealed that, for basic science grants in 2010, women were awarded a median (IQR) of $141 824 ($129 588-$201 119) per grant, whereas men were awarded $146 367 ($126 546-$176 094). The median (IQR) total grant amount awarded in 2020 increased to $176 472 ($167 481-$197 726) for women and $177 952 ($165 909-$198 426) for men (P < .001). For clinical outcomes grants, in 2010, women were awarded a median (IQR) of $135 626 ($115 369-$183 870) per grant, whereas men were awarded $209 656 ($129 108-$251 010) per grant. The median (IQR) total grant amount awarded to women significantly increased in 2020 to $199 098 ($171 341-$240 336), whereas the median (IQR) total grant amount awarded to men decreased to $180 133 ($166 028-$231 995) (P = .007). When adjusted for inflation, the median grant costs for basic science and clinical outcomes K grants were not statistically significant.
Figure 4. Median Amount per K08 and K23 Grant by Research Type and Principal Investigator Gender, 2010 vs 2020.
P values were calculated for the increase from 2010 to 2020.
Application Success Rates, K-Series Conversion Rates, and NIH Funding Longevity
Between 2010 and 2020, a mean (SD) of 2.7 (3.01) application attempts were made by women with K grants before successfully obtaining an R01 grant, whereas men had a mean (SD) of 2.3 (3.15) attempts (P = .60). There was no statistically significant difference in the K-to-R grant conversion rate between 2010 and 2020; for women the rate was 23.5%, whereas for men it was 26.7% (P = .55).
In 2010, 374 surgeon-scientists held R01 grants, of whom 57 were women (15.2%) and 317 were men (84.8%). During the next decade, 18 men surgeon-scientists retired or died and were excluded from the analysis. Between 2010 and 2020, 29 of 57 women (50.9%) and 188 of 299 men (62.9%) maintained funding (P = .10).
Discussion
As previously reported by our group, throughout the last decade, the population of surgeons with NIH funding has increased.10 The present study indicates that this increase was seen for both men and women. When analyzed in the context of the overall surgeon workforce based on AAMC data, the percentage of NIH-funded women surgeon-scientists increased from 0.5% to 0.7% between 2010 and 2020, and the percentage of men surgeon-scientists increased from 0.5% to 0.7%. Furthermore, when looking at the gender distribution of the total NIH-funded surgeon population, we found that the proportion of NIH-funded women surgeon-scientists increased from 19.0% to 25.4% during the last decade. This increase suggests that, as more women entered the surgeon workforce, a proportionately higher number were successful in securing NIH funding.
We found that the total amount of NIH funding held by women increased during the last decade (12.3% to 21.7%). Although this finding is encouraging, women continue to hold a smaller amount of funding (21.7%) in 2020 than expected based on their proportion of women surgeon-scientists (25.4%). This amount is consistent with data reported by several other studies that indicate a gender disparity exists in the amount of NIH funding awarded to women in various surgical specialties.6,7,13
Another noteworthy reflection of the status of NIH funding for women is the pattern in number of K grants awarded from 2010 to 2020. K awards are early-career mentored grants, often considered a stepping stone toward obtaining the coveted R grant and professor status. Although the total number of K grants awarded to surgeon-scientists increased, the proportion of grants held by men and women remained unchanged, with women holding 32.2% in 2010 and 33.7% in 2020. This proportion is higher than the 25.2% reported in a recently published study.14 Given that women comprise approximately 27% of the active surgeon workforce in 2020, this finding is promising.
Recently, there has been concern about the future of surgeon-scientists, especially those conducting basic science research, with surgeon-scientists being labeled a “dying breed” because of increasing clinical demands and hospitals’ need for revenue generation, NIH salary caps, and insufficient protected research time.15,16,17 However, the present study found encouraging patterns for NIH-funded basic surgeon-scientists, especially women. The total number of K grants awarded to surgeon-scientists in basic science increased from 67 in 2010 to 115 in 2020, and the number of R01 grants increased from 370 in 2010 to 466 in 2020. Furthermore, the proportion of basic science K grants held by women in 2010 vs 2020 significantly increased (23.9% to 32.2%). Similarly, for R01 basic science grants, the proportion of grants held by women also increased (13.2% to 20.2%). In addition, the median total grant cost awarded to both men and women for K and R01 grants in basic science significantly increased, with women being on par with men in 2020 (Figure 3 and Figure 4). These data suggest that the basic scientist pipeline for women surgeons is, indeed, robust.
Clinical outcomes research is increasingly becoming part of the modern surgeon-scientist’s armamentarium.18 Although the total number of K grants awarded to surgeons conducting clinical outcomes research did increase, the proportion of women holding these grants significantly decreased from 2010 to 2020 (56.5% to 36.8%). This decrease likely represents an artifact as women holding clinical outcomes grants were relatively overrepresented in 2010. The median total grant cost awarded to women during the study period increased from $135 626 to $199 098, whereas the median grant cost awarded to men decreased from $209 656 to $180 133. Despite these variations, overall patterns in median grant costs for both R and K grants in all categories suggest a narrowing of the gap between men and women in 2020 compared with 2010.
One aspect likely associated with the underrepresentation of women surgeon-scientists is the gender-based disparity in attaining independent funding by K award recipients. Jagsi et al19 reported that among K08 and K23 award recipients, women (36.2%) were less likely than men (45.6%) to receive an R01 grant. Although the K-to-R grant conversion rate for men and women surgeon-scientists was lower at 26.7% and 23.5%, respectively, we did not observe any statistically significant differences between the 2 sexes. Our findings corroborate a recently published study reporting an overall 10-year K-to-R grant conversion rate of 26.1% for surgeon-scientists with no sex-based differences.14
We analyzed the number of attempts needed for both men and women who held K awards to obtain an R01 grant, finding no statistically significant difference (women: mean, 2.7 attempts vs men: mean, 2.3 attempts). Warner et al20 reported comparable results in the rates of receipt of the first R01 awards by junior faculty. We also assessed maintenance of R01 grants among women and men surgeon-scientists. Between 2010 and 2020, more women (49.1%) lost funding compared with men (37.1%); however, this difference was not found to be statistically significant. These results are similar to those published by Hechtman et al,21 which indicate no significant differences in NIH funding longevity by gender between 1991 and 2010.
Limitations
This study has limitations. Gender was presumed based on pronouns obtained through a thorough review of biosketches and faculty online profiles; however, the authors are aware that using dichotomous genders has inherent limitations and may have led to some incorrect classifications and exclusion of nonbinary individuals. Another limitation is that we could only include NIH-funded surgeon-scientists; hence, surgeons who obtain funding from affiliated specialty societies, industry, or private foundations were not captured in our study. Moreover, the lack of detection of statistical significance in K-to-R grant conversion rates, number of R01 grant application attempts, and NIH funding longevity may be attributable to our study being underpowered.
An important limitation is that we were unable to further apply an intersectional lens to our methodologic process by including race and ethnicity data because these data are not available on iSearch Grants. Importantly, however, Ginther et al22 reported that Black applicants remain 10 percentage points less likely than White applicants to be awarded NIH research funding after controlling for the applicant’s educational background, country of origin, training, previous research awards, publication record, and employer characteristics. Black and Hispanic women face even greater disparities; Berry et al23 reported that between 1998 and 2017, only 31 (0.3%) of the 9139 NIH grants awarded to academic surgeons were awarded to Black women surgeons. Furthermore, Lewit et al8 examined the association between NIH funding for surgeon-scientists and sex and race and ethnicity and found that no Black or Hispanic women received R01 equivalent grants in 2019.
Conclusions
Findings of this cross-sectional study suggest that women surgeon-scientists have made substantial gains in obtaining NIH funding during the last decade. However, a disparity remains in total grant amounts awarded to women compared with men. Women comprise 27.4% of the surgeon workforce and 25.4% of NIH-funded surgeons; meanwhile, they hold only 21.7% of total NIH funding awarded to surgeons. Identification of factors associated with these disparities is imperative with an even greater focus needed on women belonging to underrepresented minority groups. Gender-neutral policies may appear fair on the surface but disregard pivotal differences, such as inequitable division of domestic labor or unconscious biases that women face. Policies at the institutional level are necessary, including not only creation of mentorship and sponsorship opportunities or cultural changes but also unique initiatives such as provision of onsite child care at conferences or time banking.24 Jagsi et al25 shared their experience from the establishment of the Doris Duke Charitable Foundation’s fund that supported junior physician-scientists facing substantial extraprofessional challenges, including compelling caregiving demands. Another initiative that was specifically created for women physician-scientists is the Claflin Distinguished Scholar Awards at Massachusetts General Hospital, which, based on survey results from the award recipients, laid the groundwork for attainment of funding from NIH and private foundations.26 In addition, the Association of Women Surgeons annually awards a $20 000 grant for basic science or clinical research to women surgeon-scientists. Findings of the present study emphasize the need for more academic opportunities for aspiring women surgeon-scientists and underscores the need to further narrow the gender-based gap in NIH funding.
References
- 1.Mesquita-Neto JW, Dailey W, Macedo FI, Merchant NB. Patterns of National Institutes of Health grant funding to surgical research and scholarly productivity in the United States. Ann Surg. 2020;272(4):539-546. doi: 10.1097/SLA.0000000000004206 [DOI] [PubMed] [Google Scholar]
- 2.Krebs ED, Narahari AK, Cook-Armstrong IO, et al. The changing face of academic surgery: overrepresentation of women among surgeon-scientists with R01 funding. J Am Coll Surg. 2020;231(4):427-433. doi: 10.1016/j.jamcollsurg.2020.06.013 [DOI] [PubMed] [Google Scholar]
- 3.Mesquita-Neto JW, Manoharan J, Dailey W, Macedo FI, Merchant NB. National Institutes of Health research funding to academic surgical oncologists: who are we and where do we stand? Ann Surg Oncol. 2021;28(8):4195-4202. doi: 10.1245/s10434-020-09495-2 [DOI] [PubMed] [Google Scholar]
- 4.Witteman HO, Hendricks M, Straus S, Tannenbaum C. Are gender gaps due to evaluations of the applicant or the science? a natural experiment at a national funding agency. Lancet. 2019;393(10171):531-540. doi: 10.1016/S0140-6736(18)32611-4 [DOI] [PubMed] [Google Scholar]
- 5.Oliveira DFM, Ma Y, Woodruff TK, Uzzi B. Comparison of National Institutes of Health grant amounts to first-time male and female principal investigators. JAMA. 2019;321(9):898-900. doi: 10.1001/jama.2018.21944 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Silva NA, Cerasiello SY, Herendeen JS, et al. Gender differences in NIH grant funding in neurological surgery. J Clin Neurosci. 2020;80:43-49. doi: 10.1016/j.jocn.2020.07.052 [DOI] [PubMed] [Google Scholar]
- 7.Eloy JA, Svider PF, Kovalerchik O, Baredes S, Kalyoussef E, Chandrasekhar SS. Gender differences in successful NIH grant funding in otolaryngology. Otolaryngol Head Neck Surg. 2013;149(1):77-83. doi: 10.1177/0194599813486083 [DOI] [PubMed] [Google Scholar]
- 8.Lewit RA, Black CM, Camp L, et al. Association of sex and race/ethnicity with National Institutes of Health funding of surgeon-scientists. JAMA Surg. 2021;156(2):195-197. doi: 10.1001/jamasurg.2020.5016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Berg EJ, Ashurst J. Patterns of recent National Institutes of Health (NIH) funding in general surgery: analysis using the NIH RePORTER system. Cureus. 2019;11(6):e4938. doi: 10.7759/cureus.4938 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Demblowski LA, Busse B, Santangelo G, et al. NIH funding for surgeon-scientists in the US: what is the current status? J Am Coll Surg. 2021;232(3):265-274.e2. doi: 10.1016/j.jamcollsurg.2020.12.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Association of American Medical Colleges . Physician specialty data report. Accessed April 4, 2021. https://www.aamc.org/data-reports/workforce/report/physician-specialty-data-report
- 12.US Bureau of Labor Statistics . CPI Inflation Calculator. Accessed September 29, 2021. https://www.bls.gov/data/inflation_calculator.htm.
- 13.Svider PF, D’Aguillo CM, White PE, et al. Gender differences in successful National Institutes of Health funding in ophthalmology. J Surg Educ. 2014;71(5):680-688. doi: 10.1016/j.jsurg.2014.01.020 [DOI] [PubMed] [Google Scholar]
- 14.Mesquita-Neto JW, Dailey W, Weaver D, Datta J, Macedo FI, Merchant NB. National Institutes of Health career development (K) awards to young surgeons: an academic milestone or one-hit wonder? Ann Surg. 2021;274(4):549-555. doi: 10.1097/SLA.0000000000005066 [DOI] [PubMed] [Google Scholar]
- 15.Woldu SL, Raj GV. Surgery: the surgeon-scientist—a dying breed? Nat Rev Urol. 2016;13(12):698-699. doi: 10.1038/nrurol.2016.236 [DOI] [PubMed] [Google Scholar]
- 16.Cheema AN. The surgeon-scientist: in need of resuscitation. Acad Med. 2018;93(12):1753. doi: 10.1097/ACM.0000000000002452 [DOI] [PubMed] [Google Scholar]
- 17.Kibbe MR, Velazquez OC. The extinction of the surgeon scientist. Ann Surg. 2017;265(6):1060-1061. [DOI] [PubMed] [Google Scholar]
- 18.DiBrito SR, Holscher CM, Haugen CE, et al. The modern surgeon scientist. Ann Surg. 2018;268(6):e88-e89. doi: 10.1097/SLA.0000000000002756 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jagsi R, Motomura AR, Griffith KA, Rangarajan S, Ubel PA. Sex differences in attainment of independent funding by career development awardees. Ann Intern Med. 2009;151(11):804-811. doi: 10.7326/0003-4819-151-11-200912010-00009 [DOI] [PubMed] [Google Scholar]
- 20.Warner ET, Carapinha R, Weber GM, Hill EV, Reede JY. Gender differences in receipt of National Institutes of Health R01 grants among junior faculty at an academic medical center: the role of connectivity, rank, and research productivity. J Womens Health (Larchmt). 2017;26(10):1086-1093. doi: 10.1089/jwh.2016.6102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hechtman LA, Moore NP, Schulkey CE, et al. NIH funding longevity by gender. Proc Natl Acad Sci U S A. 2018;115(31):7943-7948. doi: 10.1073/pnas.1800615115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ginther DK, Schaffer WT, Schnell J, et al. Race, ethnicity, and NIH research awards. Science. 2011;333(6045):1015-1019. doi: 10.1126/science.1196783 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Berry C, Khabele D, Johnson-Mann C, et al. A call to action: Black/African American women surgeon scientists, where are they? Ann Surg. 2020;272(1):24-29. doi: 10.1097/SLA.0000000000003786 [DOI] [PubMed] [Google Scholar]
- 24.Fassiotto M, Simard C, Sandborg C, Valantine H, Raymond J. An integrated career coaching and time-banking system promoting flexibility, wellness, and success: a pilot program at Stanford University School of Medicine. Acad Med. 2018;93(6):881-887. doi: 10.1097/ACM.0000000000002121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jagsi R, Jones RD, Griffith KA, et al. An innovative program to support gender equity and success in academic medicine: early experiences from the Doris Duke Charitable Foundation’s Fund to Retain Clinical Scientists. Ann Intern Med. 2018;169(2):128-130. doi: 10.7326/M17-2676 [DOI] [PubMed] [Google Scholar]
- 26.Jagsi R, Butterton JR, Starr R, Tarbell NJ. A targeted intervention for the career development of women in academic medicine. Arch Intern Med. 2007;167(4):343-345. doi: 10.1001/archinte.167.4.343 [DOI] [PubMed] [Google Scholar]