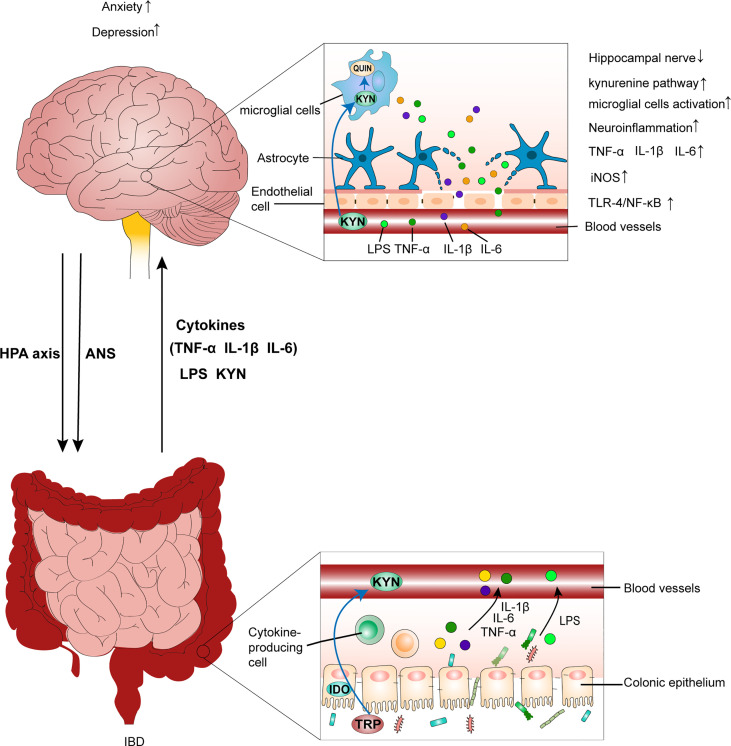
Figure 2.
IBD leads to anxiety- and depression-like behavioral comorbidities by inducing neuroinflammation. Chronic psychological stress, such as anxiety and depression, aggravates colitis by activating the HPA axis and disrupting the ANS. This is accompanied by an increase in the production of LPS, pro-inflammatory cytokines (TNF-α, IL-1β, and IL-6), and gut leak. Additionally, peripheral inflammation causes a decrease in tight junction protein expression between endothelial cells in the BBB. Then, the disruption of BBB integrity predisposes the translocation of circulating inflammatory mediators into brain tissues, which leads to the inflammatory response in the CNS by increasing IL-1β, IL-6, and TNF-α levels, activating the TLR4/NF-κB inflammatory pathway, as well as increasing iNOS and nitrite levels in brain tissues. Further, circulating inflammatory mediators reaching the brain affect neuroglial networks and activate microglial cells, which further exacerbate the inflammatory response in the CNS. Additionally, activated microglial cells can promote neurodegeneration of the hippocampal nerve, which also contributes to mood disorders. Furthermore, overactivation of the kynurenine pathway generates excess QUIN in the brain, which impairs neurons and neuroglial cells, resulting in inflammation–mediated depression. IBD, inflammatory bowel disease; HPA axis, hypothalamic-pituitary-adrenal axis; ANS, autonomic nervous system; LPS, lipopolysaccharide; BBB, blood–brain barrier; CNS, central nervous system; TRP, tryptophan; KYN, kynurenine; QUIN, neurotoxic quinolinic acid.