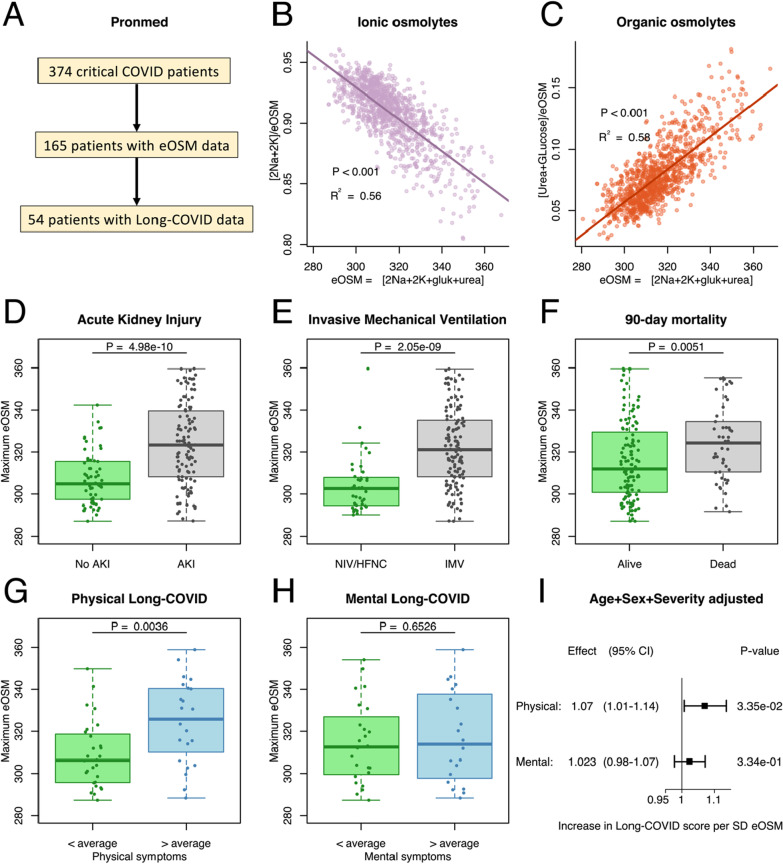
Fig. 2.
A The present study was based on a discovery analysis of the prospective observational cohort Pronmed with critically ill COVID-19 patients from the ICU at Uppsala University Hospital (A). Out of a total of 374 included patients, 165 had plasma urea analyzed at some point during their ICU stay and could be used to analyze the aestivation response through estimated osmolality (eOSM). Out of these 54 participated in the 3–6 month follow-up and provided data on remaining symptoms. B, C Aestivation response showing the fraction of the estimated total osmolality (eOSM = 2*Na + 2*K + Glucose + Urea) for the ionic osmolytes sodium and potassium (B), and the organic osmolytes glucose and urea (C), showing a shift to organic osmolytes with increasing eOSM. Pearson regression line with p value and R2 for the correlation. D, E, F Maximum dehydration measured as eOSM was higher in critically ill COVID-19 patients with important outcomes such as acute kidney injury (AKI, D), need for invasive mechanical ventilation (IMV, E), and 90-day mortality (F). Student’s T-test was used to test for chance difference. G, H, I Interestingly, maximal dehydration was higher in patients who reported more than average remaining physical (G) symptoms after 3–6 months, but not mental symptoms (H). Student’s T-test was used to test for chance difference. The analysis adjusted for sex, age and disease severity using SAPS-3 shows a substantial effect of eOSM on physical long-COVID but not on mental long-COVID (I)