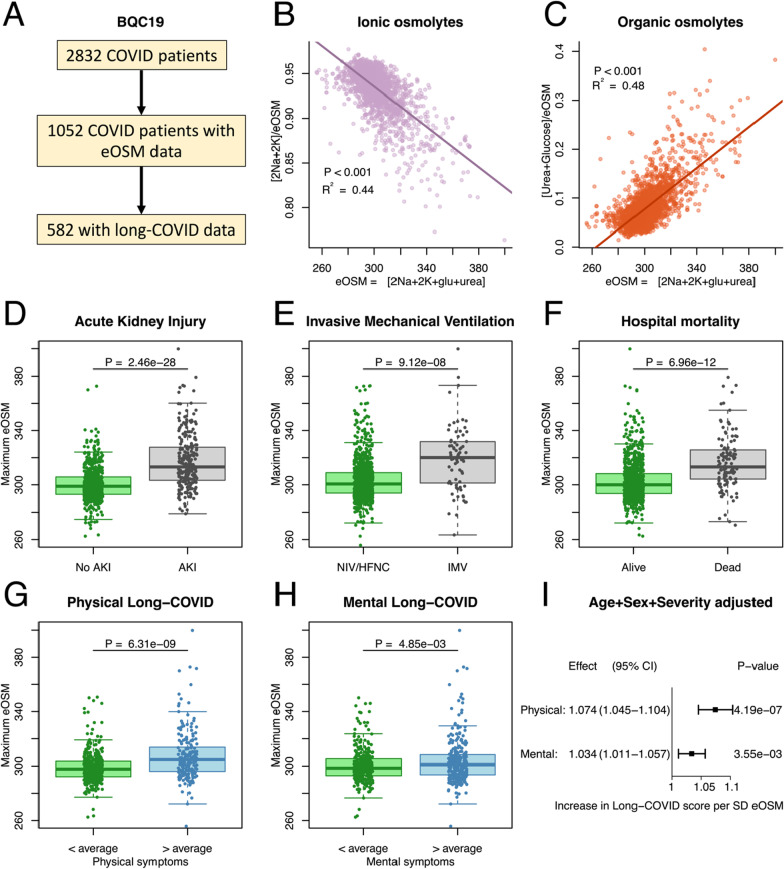
Fig. 3.
A To validate the findings the same analysis was performed in the Biobanque Québécoise de la COVID-19 (BQC19) (A). Out of a total of 3768 included patients, 1637 had plasma urea analyzed at some point during their ICU stay and could be used to analyze the aestivation response through estimated osmolality (eOSM). Out of these 872 patients filled out questionnaires on remaining symptoms. B, C The validation cohort recapitulates the aestivation response for the ionic osmolytes (B), and the organic osmolytes (C). Pearson regression line with p value and R2 for the correlation. D,E,F: As in the Pronmed cohort maximum dehydration was higher in more severely ill COVID-19 patients for the outcomes acute kidney injury (AKI, D), need for invasive mechanical ventilation (IMV, E), and hospital mortality (F). Student’s T-test was used to test for chance difference. G, H, I Finally, the association of maximal dehydration with physical symptoms after 3–6 months was reproduced (G). In addition, an association was seen for mental long-COVID in the BQC19 cohort (H). Student’s T-test was used to test for chance difference. The analysis adjusted for sex, age and disease severity using ICU-admission reproduces the substantially greater effect eOSM has on physical long-COVID than on mental long-COVID, although both show significant effect (I)