Abstract
Femoral neck fracture in the absence of trauma is a rare, but known complication after hardware removal. This complication may be due to the boney defect created by the hardware removal itself, or the increase in femoral neck strain that occurs after removal of the hardware. Previous biomechanical studies have suggested that filling the defect with calcium phosphate cement after removal of hardware may prevent the development of a femoral neck fracture. However, there are no reports on the use of calcium phosphate cement after removal of hardware in the clinical setting. The purpose of this case discussion is to present the first reported case, to our knowledge, of the use of calcium phosphate cement augmentation of the boney defect after lag screw removal, and the subsequent failure resulting in atraumatic femoral neck fracture.
Keywords: Trauma, Orthopedics, Removal of hardware, Pain
Introduction
Standard treatment of peritrochanteric fractures consists of lag screw placement through either a nail or side-plate with purchase gained into femoral head [1], [2]. In some instances, removal of hardware (ROH) is performed due to the pain associated with the retained implants [1], [2], [3], [4]. Femoral neck fractures after ROH in the absence of trauma has a reported incidence between 9 and 35 % [5], [6], [7], [8], [9]. Previous biomechanical studies have demonstrated that the mean force to cause fracture after ROH is lower, which may be associated with the boney defects caused by removing the implants [4]. A recent study by Strauss et al. found that calcium phosphate cement augmentation can increase the mean load to failure, which may prevent the occurrence of a femoral neck fracture after ROH [2]. However, to the author's knowledge, despite being suggested by several investigators, there are no reports about the use of calcium phosphate cement in patients for this purpose [2], [10]. This case report represents the first published case of clinical use of calcium phosphate as a void filler after ROH in the femoral neck and its subsequent failure.
Case report
A 40-year-old male (BMI of 24.7 kg/m2) presented to a clinic in 2021 at a level 1 trauma center with a chief complaint of point tenderness directly over the greater trochanter. The patient has a history of type-1 diabetes controlled with insulin, and a 20 pack-year history of cigarette use. He denied alcohol or illicit drugs. Three years prior to his initial presentation, the patient was treated at an outside hospital for a left intertrochanteric fracture treated with a cephallomedullary nail. X-rays of the left hip demonstrated a well healed fracture in anatomic alignment, but with lateral prominence of the lag screw (Fig. 1). After failing conservative therapies, which included physical therapy, anti-inflammatories, and a home exercise program, the patient elected to undergo removal of the lag screw while retaining the intra-medullary nail. The boney defect created by its removal was filled with HydroSet (Stryker Mahwah, NJ) (Fig. 2). The patient was allowed to weight bear as tolerated postoperatively.
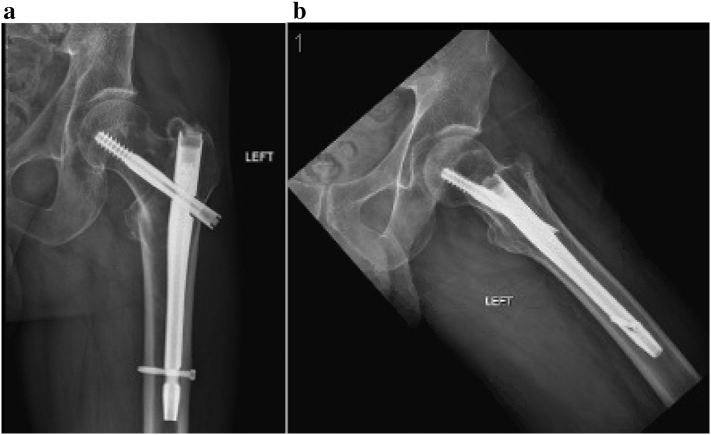
Fig. 1.
Preoperative AP (1a) and lateral (1b) x-rays of the left hip with a cephalomedullary nail demonstrating lateralization of the lag screw.
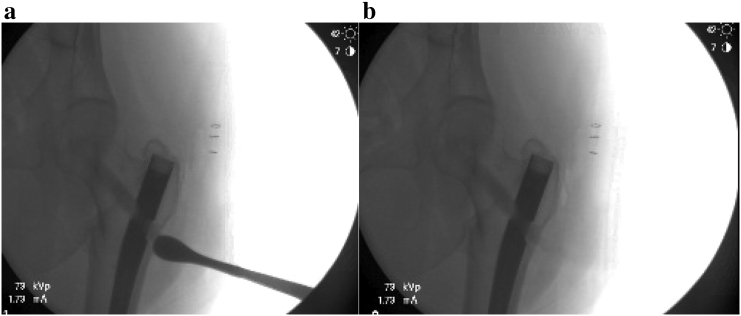
Fig. 2.
Intraoperative fluoroscopy images after removal of the lag screw and application of calcium phosphate cement.
At three weeks postop, the patient presented to the Emergency Department due to new onset left groin pain. He denied any trauma to the hip prior to the onset of symptoms. X-rays demonstrated an acute, subcapital femoral neck fracture (Fig. 3). The patient was admitted and underwent uneventful, open reduction and internal fixation with a sliding hip screw, which eventually went on to heal.
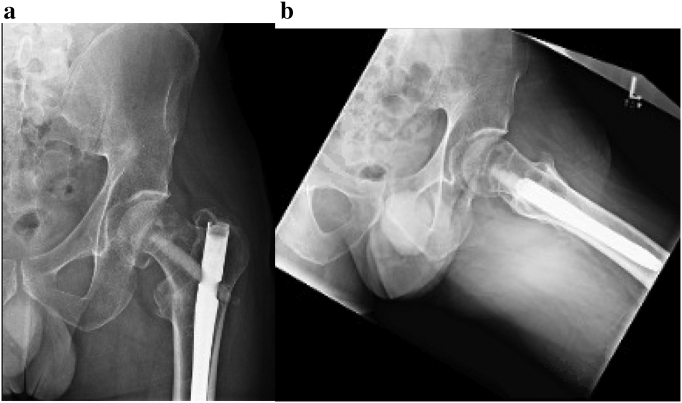
Fig. 3.
Three weeks postoperative AP (3a) and lateral (3b) x-rays of the right hip demonstrating a subcapital femoral neck fracture.
Discussion
Femoral neck fractures in the absence of trauma after removal of a cephallomedullary nail or sliding hip compression screw is a rare complication that has been documented in the orthopaedic literature [5], [6], [7], [8], [9]. This complication may be associated with the boney defect created by ROH, which can weaken the bone [3]. A previous biomedical study by Kukla et al. demonstrated that the mean load to failure was 35 % lower in cadaveric bones after ROH in comparison to cadaveric bones with retained implants [3], [4]. Other studies have suggested that the complication of a postoperative femoral neck fracture may be associated with the increase in strain in the femoral neck caused by the removal of the lag screw [3], [11]. Due to these findings, prior authors have often discouraged removal of hardware or have suggested the alternative of replacing the lag screw with one that is shorter [4], [5], [8]. However, there is currently no data in regards to outcomes after replacing the initial lag screw with a shorter screw.
There is some data to suggest that using of calcium phosphate cement augmentation may prevent a femoral neck fracture after ROH due to its ability to increase compressive strength [2], [10]. Strauss et al. demonstrated that the mean load to failure in cadaveric bones after ROH was 3994 N in comparison to 4819 N if the bone was treated with calcium phosphate cement after ROH [2]. However, there is currently no clinical data in the orthopaedic literature regarding the use of calcium phosphate cement augmentation after ROH. To the author's knowledge, this is the first case report that documents the clinical use of calcium phosphate cement augmentation after removal of a lag screw, as well as the subsequent failure.
In the case of our patient, calcium phosphate cement was injected into the boney defect after removal of the proximal lag screw. Despite the compressive strength properties of calcium phosphate cement, a subcapital femoral neck fracture occurred three weeks postoperatively in the absence of trauma. Previous investigations demonstrate calcium phosphate cement achieves most of its mechanical strength properties within 24 h, with its ultimate strength being greater than that of bone [2], [12]. This property of the cement allows for early weight bearing in the setting of osteoporotic fractures [10]. Prior studies have also observed that the primary stressors on the proximal femur are compressive in nature, which, unlike shear and tension, are well-neutralized by calcium phosphate cement [12], [13]. Based on these findings, calcium phosphate augmentation should theoretically reduce the risk of femoral neck fractures after ROH.
However, in their review of femoral neck fractures after hardware removal Barquet et al. found that pre-existing osteoporosis, local osteopenia from stress shielding, and reduction of strength from hardware removal were the three factors most associated with failure [14]. While calcium phosphate restores much of the biomechanical properties to the femoral neck after lag screw removal, it does little to augment weakness attributable to stress shielding from the implant. Biomechanical studies show that the lag screw can decrease strain in the superior neck by up to 88 % and change the type of strain from tensile to compression [15]. Simply removing the screw reverted the strains back to near normal.
In the present case, it is likely that these factors played a significant role in the femoral neck fracture despite filling the void with calcium phosphate cement. However, at age 40, he represents the youngest patient by 10 years reported with this complication, indicating patient factors also contributed. For instance, heavy tobacco use and diabetes are linked to increase risk of hip fracture [16].
Conclusion
Because of the well-described complication of femoral neck fracture, we join other authors in discouraging ROH to address symptomatic lag screws even if filling the void with calcium phosphate cement [2], [10]. This is especially true in patients harboring independent risk factors for hip fracture. Cement does little to protect the superior neck, which having previously been subject to the effects of stress-shielding would begin to bear a near normal strain, increasing the risk of fracture. Instead, replacement with a shorter screw is recommended.
Declaration of competing interest
The authors have nothing to disclose.
References
- 1.Hoffmann M.F., Khoriaty J.D., Sietsema D.L., Jones C.B. Outcome of intramedullary nailing treatment for intertrochanteric femoral fractures. J. Orthop. Surg. Res. 2019 Nov 12;14(1):360. doi: 10.1186/s13018-019-1431-3. Epub 2019/11/14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Strauss E.J., Pahk B., Kummer F.J., Egol K. Calcium phosphate cement augmentation of the femoral neck defect created after dynamic hip screw removal. J. Orthop. Trauma. 2007 May;21(5):295–300. doi: 10.1097/BOT.0b013e3180616ba5. Epub 2007/05/09. [DOI] [PubMed] [Google Scholar]
- 3.Barquet A., Giannoudis P.V., Gelink A. Femoral neck fractures after removal of hardware in healed trochanteric fractures. Injury. 2017 Dec;48(12):2619–2624. doi: 10.1016/j.injury.2017.11.031. Epub 2017/12/11. [DOI] [PubMed] [Google Scholar]
- 4.Kukla C., Pichl W., Prokesch R., Jacyniak W., Heinze G., Gatterer R., et al. Femoral neck fracture after removal of the standard gamma interlocking nail: a cadaveric study to determine factors influencing the biomechanical properties of the proximal femur. J. Biomech. 2001 Dec;34(12):1519–1526. doi: 10.1016/s0021-9290(01)00157-9. Epub 2001/11/22. [DOI] [PubMed] [Google Scholar]
- 5.Driessen M.L.S., Goessens M. Complications of implant removal after healed hip fractures. Arch. Orthop. Trauma Surg. 2020 Nov;140(11):1745–1749. doi: 10.1007/s00402-020-03435-1. Epub 2020/04/08. [DOI] [PubMed] [Google Scholar]
- 6.Shaer J.A., Hileman B.M., Newcomer J.E., Hanes M.C. Femoral neck fracture following hardware removal. Orthopedics. 2012 Jan 16;35(1):e83–e87. doi: 10.3928/01477447-20111122-34. Epub 2012/01/11. [DOI] [PubMed] [Google Scholar]
- 7.Huang C.K., Hong C.K., Su W.R., Huang Y.H., Chao L.Y. A rare complication of ipsilateral femoral neck fracture after removal of the long gamma nail in a healed intertrochanteric fracture. Ci Ji Yi Xue Za Zhi. 2020 Jan-Mar;32(1):88–90. doi: 10.4103/tcmj.tcmj_188_18. Epub 2020/02/29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yoon P.W., Kwon J.E., Yoo J.J., Kim H.J., Yoon K.S. Femoral neck fracture after removal of the compression hip screw from healed intertrochanteric fractures. J. Orthop. Trauma. 2013 Dec;27(12):696–701. doi: 10.1097/BOT.0b013e31829906a0. Epub 2013/05/15. [DOI] [PubMed] [Google Scholar]
- 9.Kyu-Hyun Yang Y.-W.C., Won Jung-Hoon, Yoo Je-Hyun. Subcapital femoral neck fracture after removal of gamma/proximal femoral nails: report of two cases. Injury Extra. 2005;36:245–248. [Google Scholar]
- 10.Larsson S., Bauer T.W. Use of injectable calcium phosphate cement for fracture fixation: a review. Clin. Orthop. Relat. Res. 2002 Feb;395:23–32. doi: 10.1097/00003086-200202000-00004. Epub 2002/04/09. [DOI] [PubMed] [Google Scholar]
- 11.Mahaisavariya B., Sitthiseripratip K., Suwanprateeb J. Finite element study of the proximal femur with retained trochanteric gamma nail and after removal of nail. Injury. 2006 Aug;37(8):778–785. doi: 10.1016/j.injury.2006.01.019. Epub 2006/02/28. [DOI] [PubMed] [Google Scholar]
- 12.Larsson S. Calcium phosphates: what is the evidence? J. Orthop. Trauma. 2010 Mar;24(Suppl 1):S41–S45. doi: 10.1097/BOT.0b013e3181cec472. Epub 2010/03/10. [DOI] [PubMed] [Google Scholar]
- 13.Rudman K.E., Aspden R.M., Meakin J.R. Compression or tension? The stress distribution in the proximal femur. Biomed Eng. Online. 2006 Feb 20;5:12. doi: 10.1186/1475-925X-5-12. Epub 2006/03/01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Barquet A., Gelink A., Giannoudis P.V. Proximal femoral fractures and vascular injuries in adults: incidence, aetiology and outcomes. Injury. 2015 Dec;46(12):2297–2313. doi: 10.1016/j.injury.2015.10.021. Epub 2015/11/03. [DOI] [PubMed] [Google Scholar]
- 15.Eberle S., Wutte C., Bauer C., von Oldenburg G., Augat P. Should extramedullary fixations for hip fractures be removed after bone union? Clin. Biomech. (Bristol, Avon) 2011 May;26(4):410–414. doi: 10.1016/j.clinbiomech.2010.12.002. Epub 2011/01/18. [DOI] [PubMed] [Google Scholar]
- 16.Kanis J.A., Johansson H., Oden A., McCloskey E.V. Assessment of fracture risk. Eur. J. Radiol. 2009 Sep;71(3):392–397. doi: 10.1016/j.ejrad.2008.04.061. Epub 2009/09/01. [DOI] [PubMed] [Google Scholar]