Abstract
Background
Fluid resuscitation is necessary to correct the sepsis-induced hypoperfusion, which is contradictory to the treatment of heart failure. This study explored the association between fluid balance (FB) of the first 24 h after ICU admission and mortality in critically ill patients with heart failure and sepsis.
Methods
Data were extracted from the Medical Information Mart for Intensive Care database. The locally weighted scatterplot smoothing (Lowess) method was used to demonstrate the relationship between FB and in-hospital mortality. Groups were divided into high FB (≥ 55.85 ml/kg) and low FB (< 55.85 ml/kg) according to the cut-off value of FB using Receiver operating characteristic analysis and Youden index method. The primary outcome was in-hospital mortality. Subgroup analyses, multivariable logistic regression analyses, and Kaplan-Meier curves were used to detect the association and survival difference between groups. Inverse probability treatment weighting (IPTW) and propensity score matching (PSM) were performed to minimize the bias of confounding factors and facilitate the comparability between groups.
Results
A total of 936 patients were included. The Lowess curve showed an approximate positive linear relationship for FB and in-hospital mortality. In the multivariable logistic regression adjusted model, high FB showed strong associations with in-hospital mortality (OR 2.53, 95% CI 1.60–3.99, p < 0.001) as compared to the low FB group. In IPTW and PSM models, high FB consistently showed higher in-hospital mortality (IPTW model: OR 1.94, 95% CI 1.52–2.49, p < 0.001; PSM model: OR 2.93, 95% CI 1.75–4.90, p < 0.001) and 30-day mortality (IPTW model: OR 1.65, 95% CI 1.29–2.10, p < 0.001; PSM model: OR 2.50, 95% CI 1.51–4.15, p < 0.001), compared with the low FB group.
Conclusion
For critically ill patients with heart failure and sepsis, high FB within the first 24 h after ICU admission could serve as an independent risk factor for in-hospital mortality and 30-day mortality. The avoidance of fluid overload exerts important effects on reducing mortality in such patients.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12871-022-01865-5.
Keywords: Critically ill patients, Heart failure, Sepsis, Fluid balance, In-hospital mortality
Background
Heart failure, as an increasing global prevalent disease, is featured as cardiovascular dysfunction with high morbidity and mortality [1]. More than 64 million people worldwide suffer from heart failure, which seriously affects their quality of life, especially for the elderly [2]. Among these patients, chronic heart failure is more common than new-onset heart failure. Infection is a common precipitating factor to induce acute decompensation in chronic heart failure. The OFICA study published by Logeart et al. demonstrated over a quarter of acute heart failure patients were induced by infection [3]. Furthermore, an Israeli study showed 38% of patients with heart failure were hospitalized because of infection-related factors [4]. Sepsis is regarded as a serious and life-threatening disease featured with multiple organ dysfunction due to patients’ dysregulation to infection. Thus, heart failure with sepsis has a complicated pathophysiological mechanism, with high mortality and a high probability of being admitted into the intensive care unit (ICU). The treatment for these patients is full of challenge since the therapeutic strategies for sepsis and heart failure are contradictory. Fluid resuscitation, as an important treatment for early management, is necessary to resolve the tissue and organ hypoperfusion induced by sepsis according to the Surviving Sepsis Campaign guidelines [5, 6]. However, excessive fluid intake can worsen the congestive symptom and increase the risk of poor prognosis for heart failure patients. Current strategies are empirical, and no relevant guidelines individually provide specific approaches according to various haemodynamic states [7]. There still remained unclear on patients’ management for fluid balance status. Therefore, this study mainly discussed the association between fluid balance (FB) of the first 24 h after ICU admission and mortality in critically ill patients with heart failure and sepsis.
Materials and methods
Data source
All the data were extracted from Medical Information Mart for Intensive Care III (MIMIC III version 1.4) database, a free-available database containing more than 40,000 patients in the intensive care unit (ICU) of the Beth Israel Deaconess Medical Center [8]. All the information in this database was anonymized to protect patients’ privacy so the ethical approval statement and informed consent were not required. One author (certification number 38,653,219 for author Zhang) gained access to the database and extracted the data using PostgreSQL tools version 10.
Study population and outcome
Sepsis patients were retrieved in terms of sepsis-3 criteria: (1) patients were confirmed with infection by positive results of microbial culture; (2) Sequential Organ Failure Assessment (SOFA) score ≥ 2 [9]. Heart failure patients were identified using the International Classification of Diseases (ICD) 9 code, including 398.91, 402.01, 402.11, 402.91, 404.01, 404.03, 404.11, 404.13, 404.91, 404.93, 428.XX. We classified heart failure as heart failure with reduced ejection fraction (LVEF ≤ 40%), heart failure with mildly-reduced ejection fraction (LVEF 40 − 50%), and heart failure with preserved ejection fraction (LVEF ≥ 50%) according to left ventricular ejection fraction (LVEF) [10]. For this study, only the first ICU admission was included in this study if patients were admitted in ICU more than once. Patients younger than 18 years or without sufficient data to calculate fluid balance were excluded. In addition, patients who spent less than 24 h in ICU, or underwent renal replacement therapy or cardiac surgery were excluded.
The outcomes were also extracted, including in-hospital mortality, 30-day mortality, as well as length of stay (LOS) in ICU and hospital. In-hospital mortality was defined as the primary outcome. The secondary outcomes were 30-day mortality, as well as LOS in ICU and hospital.
Data extraction
The following data were collected at the first ICU admission as baseline characteristics: age, gender, weight, ethnicity, infection site, left ventricular ejection fraction, mean arterial pressure (MAP). Laboratory parameters included white blood cell, hemoglobin, pH, serum potassium, serum sodium, serum bicarbonate, serum chloride, serum lactate, serum creatinine, Troponin T, and N-terminal pro-B-type natriuretic peptide (NT-proBNP). Medications included angiotensin-converting enzyme inhibitor/angiotensin receptor blocker (ACEI/ARB), beta-blocker, and vasopressor. The severity of illness was evaluated by sequential organ failure assessment (SOFA) score. Comorbidities included coronary heart disease, hypertension, chronic obstructive pulmonary disease (COPD), chronic kidney disease (CKD), cirrhosis, and diabetes. Vasopressor included epinephrine, norepinephrine, vasopressin, dopamine, dobutamine, and phenylephrine. Fluid intake and output were recorded at the first 24 h after ICU admission. Fluid intake included crystalloid, colloid, and blood products. Fluid output was defined as urine output, drainage fluid from chest and cerebral tubes, and stool. We calculated the difference between fluid input and fluid output as fluid balance (FB). All the fluid volumes have been corrected for each individual’s body weight. All baseline data were included within 24 h after ICU admission.
Statistical analysis
Categorical data were recorded as number and percentage, and compared using Pearson’s chi-squared test or Fisher’s exact test. Continuous data were recorded as mean ± standard deviation (mean ± SD) or median with interquartile range (IQR), and compared using Student’s t test or Wilcoxon rank-sum test as appropriate. The missing values of all the included variables were less than 30% and filled by the multiple imputation method (details illustrated in Supplement Table S1). The locally weighted scatterplot smoothing (Lowess) method was used to demonstrate the crude relationship between FB and in-hospital mortality. Receiver operating characteristic analysis and Youden index method were used to calculate the cut-off value of FB. For a better explanation, groups were divided according to the cut-off value and analyzed by univariable and multivariable logistical regression. Subgroup analysis was performed to detect the association of FB and in-hospital mortality among various groups according to median age, gender, LVEF, median MAP, median SOFA score, median serum lactate level, median NT-proBNP level, coronary heart disease, hypertension, COPD, CKD, cirrhosis, and diabetes. Inverse probability treatment weighting (IPTW) [11] and propensity score matching (PSM) [12] were performed to minimize the bias of confounding factors and facilitate the comparability between groups. The ratio was set as 1:1 match with a caliper width of 0.05 in the PSM model. The Kaplan-Meier method with log-rank test was performed to compare the 30-day survival rates between high and low FB. The data cleaning, statistical analyses, and data visualizations were performed using Stata version 16.0, and R software version 4.0.2. P value < 0.05 with a two-sided test was regarded as statistical significance.
Results
Baseline characteristics
A total of 936 patients were included in our study, and the selection process was described in Supplement Figure S1. The mean age of included patients was 71.59 ± 14.27 years and 52.24% were male. The median (IQR) LOS in ICU and hospital were respectively 3.34 (1.93 to 7.52) and 9.63 (5.77 to 17.05) days. The in-hospital and 30-day mortality reached 16.77% and 17.74%. The Lowess curve displayed an approximate positive linear relationship for FB and in-hospital mortality (Fig. 1). For further analysis, the cut-off value (55.85 ml/kg) of FB was calculated, and groups were further divided into the high FB group (≥ 55.85 ml/kg) and the low FB group (< 55.85 ml/kg), which was presented in Table 1.
Fig. 1.
Association of fluid balance and in-hospital mortality
Table 1.
Baseline characteristics between high and low FB groups
| Variables | Total (n = 936) | High FB (n = 349) | Low FB (n = 587) | p |
|---|---|---|---|---|
| Age (years) | 71.59 ± 14.27 | 73.37 ± 14.65 | 70.54 ± 13.94 | 0.003 |
| Gender, male, n (%) | 489 (52.24) | 173 (49.57) | 316 (53.83) | 0.207 |
| Weight (kg) | 81.03 ± 24.03 | 75.02 ± 19.93 | 84.60 ± 25.52 | < 0.001 |
| Ethnicity, n (%) | 0.112 | |||
| White | 696 (74.36) | 270 (77.36) | 426 (72.57) | |
| Black | 103 (11.00) | 29 (8.31) | 74 (12.61) | |
| Other | 137 (14.64) | 50 (14.33) | 87 (14.82) | |
| Infection site, n (%) | 0.617 | |||
| Blood | 652 (69.66) | 243 (69.63) | 409 (69.68) | |
| Urine | 187 (19.98) | 66 (18.91) | 121 (20.61) | |
| Other | 97 (10.36) | 40 (11.46) | 57 (9.71) | |
| LVEF, n (%) | 0.556 | |||
| ≤ 40% | 260 (27.78) | 90 (25.79) | 170 (28.96) | |
| 40–50% | 78 (8.33) | 31 (8.88) | 47 (8.01) | |
| ≥ 50% | 598 (63.89) | 228 (65.33) | 370 (63.03) | |
| MAP (mm Hg) | 77.30 ± 17.94 | 75.47 ± 17.38 | 78.39 ± 18.19 | 0.016 |
| Laboratory test | ||||
| White blood cell (109/L) | 10.3 (7.1, 15.55) | 11.2 (7, 16.7) | 10.1 (7.2, 14.8) | 0.046 |
| Hemoglobin (g/dL) | 11.46 ± 2.01 | 11.48 ± 2.04 | 11.45 ± 1.99 | 0.831 |
| pH | 7.36 ± 0.10 | 7.35 ± 0.11 | 7.37 ± 0.10 | 0.005 |
| Serum potassium (mmol/L) | 4.38 ± 0.87 | 4.38 ± 0.92 | 4.39 ± 0.85 | 0.867 |
| Serum sodium (mmol/L) | 137.77 ± 5.05 | 137.79 ± 5.58 | 137.76 ± 4.70 | 0.913 |
| Serum bicarbonate (mmol/L) | 24.35 ± 5.20 | 23.07 ± 5.10 | 25.11 ± 5.12 | < 0.001 |
| Serum chloride (mmol/L) | 101.65 ± 6.29 | 102.56 ± 6.73 | 101.10 ± 5.95 | < 0.001 |
| Serum lactate (mmol/L) | 1.9 (1.3, 2.8) | 2.1 (1.4, 3.2) | 1.8 (1.3, 2.5) | < 0.001 |
| Serum creatinine (mg/dL) | 1.3 (0.9, 2.1) | 1.3 (0.9, 2.1) | 1.3 (0.9, 2) | 0.608 |
| Troponin T (ng/mL) | 0.04 (0.02, 0.11) | 0.04 (0.02, 0.08) | 0.04 (0.02, 0.12) | 0.983 |
| NT-proBNP (pg/mL) | 5076 (1939, 12919.5) | 5627 (2044, 11642) | 4671 (1870, 13556) | 0.439 |
| Drug, n (%) | ||||
| ACEI/ARB | 112 (11.97) | 13 (3.72) | 99 (16.87) | < 0.001 |
| Beta-blocker | 387 (41.35) | 117 (33.52) | 270 (46.00) | < 0.001 |
| Vasopressor | 368 (39.32) | 217 (62.18) | 151 (25.72) | < 0.001 |
| SOFA | 5 (3, 8) | 7 (4, 10) | 5 (3, 7) | < 0.001 |
| Comorbidities, n (%) | ||||
| Coronary heart disease | 437 (46.69) | 140 (40.11) | 297 (50.60) | 0.002 |
| Hypertension | 484 (51.71) | 181 (51.86) | 303 (51.62) | 0.942 |
| COPD | 71 (7.59) | 13 (3.72) | 58 (9.88) | 0.001 |
| CKD | 336 (35.90) | 112 (32.09) | 224 (38.16) | 0.061 |
| Cirrhosis | 70 (7.48) | 31 (8.88) | 39 (6.64) | 0.208 |
| Diabetes | 443 (47.33) | 133 (38.11) | 310 (52.81) | < 0.001 |
| Fluid balance status | ||||
| Fluid intake (ml/kg/24 h) | 61.14 (30.00, 109.78) | 127.60 (97.41, 174.30) | 36.36 (20.54, 56.19) | < 0.001 |
| Fluid output (ml/kg/24 h) | 21.81 (12.07, 37.70) | 19.79 (11.11, 37.17) | 23.31 (12.66, 38.17) | 0.076 |
| Fluid balance (ml/kg/24 h) | 36.90 (5.09, 81.19) | 98.28 (73.08, 142.88) | 13.93 (-5.11, 32.33) | < 0.001 |
| Clinical Outcomes | ||||
| In-hospital mortality, n (%) | 157 (16.77) | 97 (27.79) | 60 (10.22) | < 0.001 |
| 30-day mortality, n (%) | 166 (17.74) | 99 (28.37) | 67 (11.41) | < 0.001 |
| ICU LOS (days) | 3.34 (1.93, 7.52) | 4.85 (2.62, 9.08) | 2.82 (1.82, 5.91) | < 0.001 |
| Hospital LOS (days) | 9.63 (5.77, 17.05) | 11.35 (7.32, 21.11) | 8.52 (4.97, 14.94) | < 0.001 |
Abbreviations: ACEI, angiotensin-converting enzyme inhibitor; ARB, angiotensin receptor blocker; CKD, chronic kidney disease; COPD, chronic obstructive pulmonary disease; FB, fluid balance; ICU, intensive care unit; LOS, length of stay; LVEF, left ventricular ejection fraction; MAP, mean arterial pressure; NT-proBNP, N-terminal pro-B-type natriuretic peptide; SOFA, sequential organ failure assessment
Association between fluid balance and in-hospital mortality
After groups were divided according to the cut-off value, the difference of FB between groups was mainly associated with fluid intake (p < 0.001) instead of fluid output (p = 0.076) (Table 1). Patients with high FB showed higher in-hospital mortality (27.79% vs. 10.22%, p < 0.001) and 30-day mortality (28.37% vs. 11.41%, p < 0.001), as well as longer LOS in ICU (4.85 [2.62, 9.08] vs. 2.82 [1.82, 5.91], p < 0.001) and hospital (11.35 [7.32, 21.11] vs. 8.52 [4.97, 14.94], p < 0.001), as compared to the lower FB group (Table 1).The crude model demonstrated that in-hospital mortality (OR 3.38, 95% CI 2.37–4.82, p < 0.001) and 30-day mortality (OR 3.07, 95% CI 2.18–4.34, p < 0.001) were significantly higher for patients with high FB (Table 2). Subgroup analyses revealed that high FB had higher risks of in-hospital mortality in most of the subgroups except for patients with COPD or cirrhosis (Fig. 2). In the adjusted model, which further adjusted for all included covariates, high FB was regarded as an independent risk factor for in-hospital mortality (OR 2.53, 95% CI 1.60–3.99, p < 0.001) and 30-day mortality (OR 2.08, 95% CI 1.34–3.23, p = 0.001) compared with low FB (Table 2). FB also showed strong and consistent associations with in-hospital mortality (crude model: OR 1.67, 95% CI 1.39–1.99 per SD increase, p < 0.001; adjusted model: OR 1.32, 95% CI 1.04 to 1.69 per SD increase, p = 0.024) and 30-day mortality (crude model: OR 1.67, 95% CI 1.40–1.99 per SD increase, p < 0.001; adjusted model: OR 1.28, 95% CI 1.01–1.63 per SD increase, p = 0.041) when analyzed as a continuous variable (Table 2).
Table 2.
Association of FB and mortality in various models
| Crude Model | Adjusted Model | IPTW Model | PSM Model | |||||
|---|---|---|---|---|---|---|---|---|
| OR (95% CI) | p | OR (95% CI) | p | OR (95% CI) | p | OR (95% CI) | p | |
| Categorical FB | ||||||||
| In-hospital mortality | ||||||||
| Low FB | 1.0 (Reference) | - | 1.0 (Reference) | - | 1.0 (Reference) | - | 1.0 (Reference) | - |
| High FB | 3.38 (2.37, 4.82) | < 0.001 | 2.53 (1.60, 3.99) | < 0.001 | 1.94 (1.52, 2.49) | < 0.001 | 2.93 (1.75, 4.90) | < 0.001 |
| 30-day mortality | ||||||||
| Low FB | 1.0 (Reference) | - | 1.0 (Reference) | - | 1.0 (Reference) | - | 1.0 (Reference) | - |
| High FB | 3.07 (2.18, 4.34) | < 0.001 | 2.08 (1.34, 3.23) | 0.001 | 1.65 (1.29, 2.10) | < 0.001 | 2.50 (1.51, 4.15) | < 0.001 |
| Continuous FB | ||||||||
| In-hospital mortality | 1.67 (1.39, 1.99) | < 0.001 | 1.32 (1.04, 1.69) | 0.024 | 1.66 (1.39, 1.99) | < 0.001 | 1.45 (1.13, 1.88) | 0.004 |
| 30-day mortality | 1.67 (1.40, 1.99) | < 0.001 | 1.28 (1.01, 1.63) | 0.041 | 1.67 (1.40, 1.99) | < 0.001 | 1.35 (1.04, 1.74) | 0.022 |
Note: Crude model: No covariates were adjusted. Adjusted Model: adjusted for age, gender, ethnicity, weight, infection site, LVEF, MAP, laboratory test, drug, SOFA, and comorbidities
Abbreviations: CI, confidence interval; FB, fluid balance; LVEF, left ventricular ejection fraction; IPTW, inverse probability of treatment weighting; MAP, mean arterial pressure; OR, odds ratio; PSM, propensity score-matching; SOFA, sequential organ failure assessment
Fig. 2.
Forrest plots for the association of high FB and clinical outcomes in subgroups. Abbreviations: CI, confidence interval; CKD, chronic kidney disease; COPD, chronic obstructive pulmonary disease; FB, fluid balance; LVEF, left ventricular ejection fraction; MAP, mean arterial pressure; NT-proBNP, N-terminal pro-B-type natriuretic peptide; OR, odds ratio; SOFA, sequential organ failure assessment
IPTW and PSM analyses
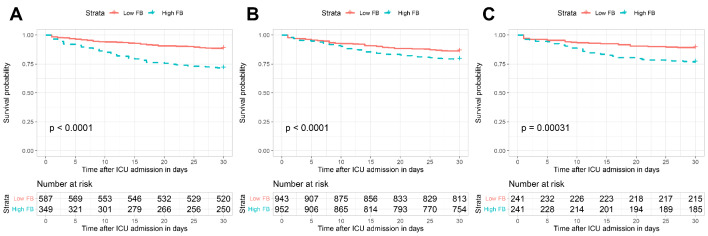
In the IPTW model, baseline characteristics between groups were well balanced. After PSM, 241 patients were well matched by a 1:1 ratio for each group. No significant differences were found in the baseline characteristics between the matched groups (Supplement Table S2). Regression analyses verified stronger monotonic associations of FB with in-hospital mortality (IPTW model: OR 1.66, 95% CI 1.39–1.99 per SD increase, p < 0.001; PSM model: OR 1.45, 95% CI 1.13–1.88 per SD increase, p = 0.004) and 30-day mortality (IPTW model: OR 1.67, 95% CI 1.40–1.99 per SD increase, p < 0.001; PSM model: OR 1.35, 95% CI 1.04–1.74 per SD increase, p = 0.022) (Table 2). In IPTW and PSM models, high FB consistently showed higher in-hospital mortality (IPTW model: OR 1.94, 95% CI 1.52–2.49, p < 0.001; PSM model: OR 2.93, 95% CI 1.75–4.90, p < 0.001) and 30-day mortality (IPTW model: OR 1.65, 95% CI 1.29–2.10, p < 0.001; PSM model: OR 2.50, 95% CI 1.51–4.15, p < 0.001), compared with the low FB group (Table 2). As depicted in the Kaplan-Meier survival curves, patients with low FB show better 30-day survival than those with high FB in the crude model (Fig. 3A), the IPTW model (Fig. 3B), and the PSM model (Fig. 3C).
Fig. 3.
The 30-day cumulative survival probability for each group. (A) Original cohort, (B) After IPTW, (C) After PSM. Abbreviations: FB, fluid balance; IPTW, inverse probability of treatment weighting; PSM, propensity score-matching
Discussion
Currently, few studies have discussed the relationship between FB and mortality in critically ill patients with heart failure and sepsis. To our knowledge, the cut-off value of FB is the first to be reported in this study for critically ill patients with heart failure and sepsis. In this study, fluid intake, fluid output, and FB have been corrected for each patient’s body weight, which is an improvement over many studies that just calculated absolute volumes of fluid resuscitation. We found that high FB was an independent risk factor for in-hospital mortality and 30-day mortality, as well as associated with longer LOS in ICU and hospital. The conclusions are consistent and robust by subgroup, multivariable logistic regression, IPTW, and PSM analyses, which can provide a reliable assessment for the impact of FB on prognosis in such patients in a real clinical setting.
Our results show the benefits of low FB and verify the detrimental impacts of fluid overload. The potential mechanism may be that high FB accelerates the multiple organ disorder [13]. First, cardiotoxicity and glycocalyx damage induced by fluid overload has been confirmed in animal models [14, 15]. Large volume intake is a contributor to myocardial injury because of myocardial edema and oxidative stress. The FEAST trial showed cardiovascular collapse generated refractory shock, contributing most to the excessive mortality [16]. Second, for patients with high FB, increased atrial and venous pressure can facilitate the fluid transfer to the interstitial space and aggravate tissue edema, which results in tissue distortion and microcirculation disorder, and thus leads to cell metabolism disturbance [13, 17]. Third, increased venous pressure can minimize renal perfusion, which is harmful to kidney function [17]. Fourth, aggressive fluid intake is proved to promote intra-abdominal hypertension, which is closely related to respiratory dysfunction, reduced hepatic perfusion, bowel malabsorption and obstruction, and even death [18, 19]. On the other hand, although no statistical differences were found in the subgroup of patients with COPD or cirrhosis, the small sample size of each stratification limits its results. Besides, FB status also depends on the previous extent of fluid accumulation, although patients who can achieve low or negative FB may indicate their better organ function [20]. Further studies are needed to investigate the specific mechanism.
Early and immediate fluid resuscitation has been recommended in the updated Surviving Sepsis Campaign guidelines because fluid intake can reverse hypotension and correct tachycardia in patients with sepsis [5, 13]. However, this guideline also acknowledged that this recommendation is based on low-quality evidence [21]. Several studies reported the relationship between FB and mortality in sepsis by setting various thresholds of volume and time points. A multicentric Scandinavian study showed no statistical difference between FB and mortality [22]. Moreover, a meta-analysis published by Meyhoff et al. did not find the protective effects of restrictive fluid intake as well [23]. On the contrary, there is still evidence of harmful effects of fluid resuscitation [24, 25]. Fluid intake of more than 5 L on the 1st day of hospital admission increased the risk of excess deaths [26]. Similarly, FB over 3 L between the 24th and the 48th hour after diagnosis increased the risk of mortality in severe sepsis [27]. Consecutive positive FB within 3 days had a higher risk of in-hospital mortality [28]. However, the time point of FB varies among current studies and no unified criteria have been achieved. Conclusions regarding the relationship between early FB status and mortality are conflicting in current studies [24, 29]. It has also been suggested that early fluid accumulation (within 24 h after ICU admission) was not associated with increased mortality in septic patients [24, 29], and even Brotfain et al. highlighted the beneficial effects of early fluid resuscitation [30]. This might indicate that septic patients have a certain tolerance for the adverse effects of fluid overload, and furthermore, early fluid resuscitation is still recommended by the guidelines [31]. Besides, the volume of fluid intake and output may be recorded inaccurately during clinical practice due that partial fluid losses are difficult to measure. Many studies only calculated the absolute volumes of fluid intake, instead of the relative volumes adjusted by individuals’ weight. Additionally, fluid responsiveness and levels of haemodynamic disturbance are hard to be defined and stratified in various groups [32]. Therefore, with respect to fluid resuscitation for sepsis, the evidence of most trials was not strong enough to make a clear consensus.
As is well-known, limiting fluid intake and increasing fluid output is the principle of heart failure treatment, which is paradoxical with medical treatment for sepsis [7]. Koell et al. noted that fluid overload was associated with adverse prognosis in patients with heart failure and preserved ejection fraction [33]. Fluid accumulation and redistribution result in the expansion of interstitial and intravascular space in organs. Right heart hemodynamic data lack reliability for precise fluid management because of its provided limited information, although commonly utilized for the evaluation of fluid balance status in ICU [6, 34]. Regarding studies on heart failure with sepsis, it has been reported that almost 25% of heart failure patients died of sepsis [35]. The survivors accepted more fluid intake within the first 6 h for patients with heart failure with reduced ejection fraction and septic shock [36].
On the basis of current researches combined with our results, early fluid resuscitation can correct hypotension and increase cardiac output, while late fluid overload by continuous volume intake is harmful. We resume that FB status should be paid attention and the strategy of limited fluid intake should be adopted as long as vital signs have been corrected and reached stability. The cut-off value of FB, instead of positive or negative FB, may provide guidance for the assessment of patients’ states and prognosis, and timely adjust the treatment strategy. The speed and amount of fluid intake should be cautiously treated in patients with heart failure and sepsis.
Limitations
Several limitations should be considered for our study. First, potential bias may not fully eliminate and undetected confounding factors might exist although subgroup analyses, as well as adjusted, IPTW, and PSM models reached consistent results. Second, fluid overload, as a haemodynamic state, cannot be prospectively randomized so it has to be replaced by FB. FB and haemodynamic status before ICU admission were not available in the database, to a certain extent, which could cause information bias. Third, only the relationship between high FB and in-hospital mortality can be inferred due to the nature of the retrospective study design. Prospective cohort studies are needed to further detect whether a causal association of high FB and mortality exists. In addition, some variables were not included due to excessive missing values. In this study, the relatively small percentage of missing data might also have potential impacts on our results. Multicentric cohort studies are needed to further validate the results due to the single-center study design.
Conclusion
In conclusion, for critically ill patients with heart failure and sepsis, high FB within the first 24 h after ICU admission could serve as an independent risk factor for in-hospital mortality and 30-day mortality. The avoidance of fluid overload exerts important effects on reducing mortality in such patients. Future studies are needed to further establish the optimal strategy on fluid status management for patients with heart failure and sepsis.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
None.
Abbreviations and acronyms
- ACEI
Angiotensin-converting enzyme inhibitor.
- ARB
Angiotensin receptor blocker.
- CI
Confidence interval.
- COPD
Chronic obstructive pulmonary disease.
- CKD
Chronic kidney disease.
- FB
Fluid balance.
- ICU
Intensive care unit.
- IPTW
Inverse probability of treatment weighting.
- IQR
Interquartile range.
- LOS
Length of stay.
- LVEF
Left ventricular ejection fraction.
- MAP
Mean arterial pressure.
- MIMIC
Medical Information Mart for Intensive Care.
- NT-proBNP
N-terminal pro-B-type natriuretic peptide.
- OR
Odds ratio.
- PSM
Propensity score matching.
- SD
Standard deviation.
- SOFA
Sequential organ failure assessment.
Authors’ contribution
BZ, SG, and ZL accomplished the study design. BZ extracted the data and performed the quality assessment. BZ, SG, and NW contributed to the statistical analysis. ZF, NW, and ZL were responsible for data validation. BZ, SG, ZF, NW, and ZL wrote and revised the manuscript. All authors have full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the analysis.
Funding
This work was supported by the Natural Science Foundation of Tianjin City [18JCZDJC36200 and 21JCYBJC00900].
Data availability
The datasets generated and/or analyzed during the current study are available in the PhysioBank repository (mimic.physionet.org).
Declarations
Ethics approval and consent to participate
The establishment of MIMIC III database was approved by the institutional review boards of Beth Israel Deaconess Medical Center and Massachusetts Institute of Technology Affiliates. This is an open and free database, and researchers must complete an online course at the National Institutes of Health, known as Protecting Human Research Participants, before they can apply for permission to access it. The Protecting Human Research Participants’ exam was passed to gain access to the MIMIC III database and consent was obtained for the original data collection and analysis (certification number 38653219). All the information in this database was anonymized to protect patients’ privacy, so the ethical approval statement and the informed consent were waived. The authors confirm that all methods were performed in accordance with the relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Bufan Zhang and Shaohua Guo contributed equally to this work.
Contributor Information
Naishi Wu, Email: wunaishi@tmu.edu.cn.
Zhigang Liu, Email: liuzgtedaich@163.com.
References
- 1.Gupta AK, Tomasoni D, Sidhu K, Metra M, Ezekowitz JA. Evidence-Based Management of Acute Heart Failure. Can J Cardiol. 2021;37(4):621–31. doi: 10.1016/j.cjca.2021.01.002. [DOI] [PubMed] [Google Scholar]
- 2.Groenewegen A, Rutten FH, Mosterd A, Hoes AW. Epidemiology of heart failure. Eur J Heart Fail. 2020;22(8):1342–56. doi: 10.1002/ejhf.1858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Logeart D, Isnard R, Resche-Rigon M, Seronde MF, de Groote P, Jondeau G, Galinier M, Mulak G, Donal E, Delahaye F, et al. Current aspects of the spectrum of acute heart failure syndromes in a real-life setting: the OFICA study. Eur J Heart Fail. 2013;15(4):465–76. doi: 10.1093/eurjhf/hfs189. [DOI] [PubMed] [Google Scholar]
- 4.Alon D, Stein GY, Korenfeld R, Fuchs S. Predictors and outcomes of infection-related hospital admissions of heart failure patients. PLoS ONE. 2013;8(8):e72476. doi: 10.1371/journal.pone.0072476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Levy MM, Evans LE, Rhodes A. The Surviving Sepsis Campaign Bundle: 2018 Update. Crit Care Med. 2018;46(6):997–1000. doi: 10.1097/CCM.0000000000003119. [DOI] [PubMed] [Google Scholar]
- 6.Rhodes A, Evans LE, Alhazzani W, Levy MM, Antonelli M, Ferrer R, Kumar A, Sevransky JE, Sprung CL, Nunnally ME, et al. Surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock: 2016. Intensive Care Med. 2017;43(3):304–77. doi: 10.1007/s00134-017-4683-6. [DOI] [PubMed] [Google Scholar]
- 7.Arfaras-Melainis A, Polyzogopoulou E, Triposkiadis F, Xanthopoulos A, Ikonomidis I, Mebazaa A, Parissis J. Heart failure and sepsis: practical recommendations for the optimal management. Heart Fail Rev. 2020;25(2):183–94. doi: 10.1007/s10741-019-09816-y. [DOI] [PubMed] [Google Scholar]
- 8.Johnson AE, Pollard TJ, Shen L, Lehman LW, Feng M, Ghassemi M, Moody B, Szolovits P, Celi LA, Mark RG. MIMIC-III, a freely accessible critical care database. Sci Data. 2016;3:160035. doi: 10.1038/sdata.2016.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, Bellomo R, Bernard GR, Chiche JD, Coopersmith CM, et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3) JAMA. 2016;315(8):801–10. doi: 10.1001/jama.2016.0287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McDonagh TA, Metra M, Adamo M, Gardner RS, Baumbach A, Bohm M, Burri H, Butler J, Celutkiene J, Chioncel O, et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2021;42(36):3599–726. doi: 10.1093/eurheartj/ehab368. [DOI] [PubMed] [Google Scholar]
- 11.Chesnaye NC, Stel VS, Tripepi G, Dekker FW, Fu EL, Zoccali C, Jager KJ. An introduction to inverse probability of treatment weighting in observational research. Clin Kidney J. 2022;15(1):14–20. doi: 10.1093/ckj/sfab158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Deb S, Austin PC, Tu JV, Ko DT, Mazer CD, Kiss A, Fremes SE. A Review of Propensity-Score Methods and Their Use in Cardiovascular Research. Can J Cardiol. 2016;32(2):259–65. doi: 10.1016/j.cjca.2015.05.015. [DOI] [PubMed] [Google Scholar]
- 13.Marik PE, Byrne L, van Haren F. Fluid resuscitation in sepsis: the great 30 mL per kg hoax. J Thorac Dis. 2020;12(Suppl 1):37–47. doi: 10.21037/jtd.2019.12.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Byrne L, Obonyo NG, Diab SD, Dunster KR, Passmore MR, Boon AC, Hoe LS, Pedersen S, Fauzi MH, Pimenta LP, et al. Unintended Consequences: Fluid Resuscitation Worsens Shock in an Ovine Model of Endotoxemia. Am J Respir Crit Care Med. 2018;198(8):1043–54. doi: 10.1164/rccm.201801-0064OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Byrne L, Obonyo NG, Diab S, Dunster K, Passmore M, Boon AC, Hoe LS, Hay K, Van Haren F, Tung JP, et al. An Ovine Model of Hyperdynamic Endotoxemia and Vital Organ Metabolism. Shock. 2018;49(1):99–107. doi: 10.1097/SHK.0000000000000904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Maitland K, George EC, Evans JA, Kiguli S, Olupot-Olupot P, Akech SO, Opoka RO, Engoru C, Nyeko R, Mtove G, et al. Exploring mechanisms of excess mortality with early fluid resuscitation: insights from the FEAST trial. BMC Med. 2013;11:68. doi: 10.1186/1741-7015-11-68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Prowle JR, Kirwan CJ, Bellomo R. Fluid management for the prevention and attenuation of acute kidney injury. Nat Rev Nephrol. 2014;10(1):37–47. doi: 10.1038/nrneph.2013.232. [DOI] [PubMed] [Google Scholar]
- 18.Kirkpatrick AW, Roberts DJ, De Waele J, Jaeschke R, Malbrain ML, De Keulenaer B, Duchesne J, Bjorck M, Leppaniemi A, Ejike JC, et al. Intra-abdominal hypertension and the abdominal compartment syndrome: updated consensus definitions and clinical practice guidelines from the World Society of the Abdominal Compartment Syndrome. Intensive Care Med. 2013;39(7):1190–206. doi: 10.1007/s00134-013-2906-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dalfino L, Tullo L, Donadio I, Malcangi V, Brienza N. Intra-abdominal hypertension and acute renal failure in critically ill patients. Intensive Care Med. 2008;34(4):707–13. doi: 10.1007/s00134-007-0969-4. [DOI] [PubMed] [Google Scholar]
- 20.Shen Y, Huang X, Zhang W. Association between fluid intake and mortality in critically ill patients with negative fluid balance: a retrospective cohort study. Crit Care. 2017;21(1):104. doi: 10.1186/s13054-017-1692-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lonsdale DO, Shah RV, Lipman J. Infection, Sepsis and the Inflammatory Response: Mechanisms and Therapy. Front Med (Lausanne) 2020;7:588863. doi: 10.3389/fmed.2020.588863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cronhjort M, Hjortrup PB, Holst LB, Joelsson-Alm E, Martensson J, Svensen C, Perner A. Association between fluid balance and mortality in patients with septic shock: a post hoc analysis of the TRISS trial. Acta Anaesthesiol Scand. 2016;60(7):925–33. doi: 10.1111/aas.12723. [DOI] [PubMed] [Google Scholar]
- 23.Meyhoff TS, Moller MH, Hjortrup PB, Cronhjort M, Perner A, Wetterslev J. Lower vs Higher Fluid Volumes During Initial Management of Sepsis: A Systematic Review With Meta-Analysis and Trial Sequential Analysis. Chest. 2020;157(6):1478–96. doi: 10.1016/j.chest.2019.11.050. [DOI] [PubMed] [Google Scholar]
- 24.Sakr Y, Rubatto Birri PN, Kotfis K, Nanchal R, Shah B, Kluge S, Schroeder ME, Marshall JC, Vincent JL. Intensive Care Over Nations I. Higher Fluid Balance Increases the Risk of Death From Sepsis: Results From a Large International Audit. Crit Care Med. 2017;45(3):386–94. doi: 10.1097/CCM.0000000000002189. [DOI] [PubMed] [Google Scholar]
- 25.Yue J, Zheng R, Wei H, Li J, Wu J, Wang P, Zhao H. Childhood Mortality After Fluid Bolus With Septic or Severe Infection Shock: A Systematic Review and Meta-Analysis. Shock. 2021;56(2):158–66. doi: 10.1097/SHK.0000000000001657. [DOI] [PubMed] [Google Scholar]
- 26.Marik PE, Linde-Zwirble WT, Bittner EA, Sahatjian J, Hansell D. Fluid administration in severe sepsis and septic shock, patterns and outcomes: an analysis of a large national database. Intensive Care Med. 2017;43(5):625–32. doi: 10.1007/s00134-016-4675-y. [DOI] [PubMed] [Google Scholar]
- 27.de Oliveira FS, Freitas FG, Ferreira EM, de Castro I, Bafi AT, de Azevedo LC, Machado FR. Positive fluid balance as a prognostic factor for mortality and acute kidney injury in severe sepsis and septic shock. J Crit Care. 2015;30(1):97–101. doi: 10.1016/j.jcrc.2014.09.002. [DOI] [PubMed] [Google Scholar]
- 28.Zhang L, Xu F, Li S, Zheng X, Zheng S, Liu H, Lyu J, Yin H. Influence of fluid balance on the prognosis of patients with sepsis. BMC Anesthesiol. 2021;21(1):269. doi: 10.1186/s12871-021-01489-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Smith SH, Perner A. Higher vs. lower fluid volume for septic shock: clinical characteristics and outcome in unselected patients in a prospective, multicenter cohort. Crit Care. 2012;16(3):R76. doi: 10.1186/cc11333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Brotfain E, Koyfman L, Toledano R, Borer A, Fucs L, Galante O, Frenkel A, Kutz R, Klein M. Positive fluid balance as a major predictor of clinical outcome of patients with sepsis/septic shock after ICU discharge. Am J Emerg Med. 2016;34(11):2122–6. doi: 10.1016/j.ajem.2016.07.058. [DOI] [PubMed] [Google Scholar]
- 31.Evans L, Rhodes A, Alhazzani W, Antonelli M, Coopersmith CM, French C, Machado FR, Mcintyre L, Ostermann M, Prescott HC, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock 2021. Intensive Care Med. 2021;47(11):1181–247. doi: 10.1007/s00134-021-06506-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Messmer AS, Zingg C, Muller M, Gerber JL, Schefold JC, Pfortmueller CA. Fluid Overload and Mortality in Adult Critical Care Patients-A Systematic Review and Meta-Analysis of Observational Studies. Crit Care Med. 2020;48(12):1862–70. doi: 10.1097/CCM.0000000000004617. [DOI] [PubMed] [Google Scholar]
- 33.Koell B, Zotter-Tufaro C, Duca F, Kammerlander AA, Aschauer S, Dalos D, Antlanger M, Hecking M, Saemann M, Mascherbauer J, et al. Fluid status and outcome in patients with heart failure and preserved ejection fraction. Int J Cardiol. 2017;230:476–81. doi: 10.1016/j.ijcard.2016.12.080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Miller WL. Fluid Volume Overload and Congestion in Heart Failure: Time to Reconsider Pathophysiology and How Volume Is Assessed. Circ Heart Fail. 2016;9(8):e002922. doi: 10.1161/CIRCHEARTFAILURE.115.002922. [DOI] [PubMed] [Google Scholar]
- 35.Walker AMN, Drozd M, Hall M, Patel PA, Paton M, Lowry J, Gierula J, Byrom R, Kearney L, Sapsford RJ, et al. Prevalence and Predictors of Sepsis Death in Patients With Chronic Heart Failure and Reduced Left Ventricular Ejection Fraction. J Am Heart Assoc. 2018;7(20):e009684. doi: 10.1161/JAHA.118.009684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wardi G, Wali A, Sell R, Malhotra A, Beitler J. Impact of fluid resuscitation on septic patients with systolic heart failure. Crit Care Med. 2016;44(12):446. doi: 10.1097/01.ccm.0000510156.55790.66. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets generated and/or analyzed during the current study are available in the PhysioBank repository (mimic.physionet.org).