Abstract
Background:
A third comprehensive study of fetal alcohol spectrum disorders (FASD) in a rural, agricultural region of South Africa is described.
Methods:
Population-based, active case ascertainment methods were employed among a school-based cohort to assess child physical and neurobehavioral traits, and maternal risk factor interviews conducted to identify all children with FASD to determine FASD prevalence.
Results:
Consent was obtained for 76.7% of 1158 children attending first grade in the region’s public schools. Case control results are presented for 95 with fetal alcohol syndrome (FAS), 64 with partial fetal alcohol syndrome (PFAS), 77 with alcohol-related neurodevelopmental disorder (ARND), 2 with alcohol-related birth defects (ARBD), and 213 randomly-selected controls. Four techniques estimating FASD prevalence from in-person examinations and testing yielded a range of total FASD prevalence of 206-366 per 1,000. Final weighted, estimated prevalence of FAS was 104.5 per 1,000, PFAS was 77.7 per 1,000, ARND was 125.2 per 1,000, and total FASD prevalence was 310 per 1,000 (95% CI = 283.4 – 336.7). Expressed as a percentage, 31% had FASD. Although the rate of total FASD remained steady over nine years, the proportion of children within the FASD group has changed significantly: FAS trended downward, and ARND trended upward. A detailed evaluation is presented of the specific child physical and neurobehavioral traits integral to assessing the full continuum of FASD. The diagnosis of a child with FASD was significantly associated with maternal proximal risk factors such as: co-morbid prenatal use of alcohol and tobacco (OR=19.1); maternal drinking of two (OR=5.9), three (OR=5.9), four (OR=38.3), or more alcoholic drinks per drinking day; and drinking in the first trimester (OR=8.4), first and second trimesters (OR=17.7), or throughout pregnancy (OR=18.6). Distal maternal risk factors included: slight or small physical status (height, weight, and head circumference), lower BMI, less formal education, late recognition of pregnancy, and higher gravidity, parity, and older age during the index pregnancy.
Conclusion:
The prevalence of FASD remained a significant problem in this region, but the severity of physical traits and anomalies within the continuum of FASD is trending downwards.
Keywords: fetal alcohol spectrum disorders (FASD), prenatal alcohol use, maternal risk for FASD, prevalence, child traits of FASD, South Africa
INTRODUCTION
Prevalence Studies of Fetal Alcohol Spectrum Disorders
There have been fifteen active case ascertainment, population-based studies of fetal alcohol spectrum disorders (FASD) published in the recent past for North America (Chambers et al., 2019; May et al., 2021a, 2020a, 2020b, 2020c, 2018, 2015, 2014a; Popova et al., 2019) and Europe (May et al., 2011a, 2006; McCarthy et al., 2021; Okulicz-Kozaryn et al., 2017; Petkovic and Barisic, 2013, 2010). Most authors of these studies have cited difficulty in accessing populations to study FASD in these more-developed countries due to difficulties in obtaining approvals from local communities and institutions and skepticism about the benefits of participation in public health research. Therefore, many studies ended with a statement that findings should be considered “undercounts” (May et al., 2021b). Even though all the above studies used state-of-the-art active case ascertainment, the undercount problem revealed a need for techniques to estimate the true prevalence of FASD in populations where consent rates were low.
In the NIAAA-funded “Collaborative Initiative on FASD Prevalence” (CoFASP) in the United States (US) from 2010 to 2019, one goal was to produce a weighted estimation technique for use in active case ascertainment studies. With in-school populations, the methods adopted by CoFASP investigators employed in-person child physical/dysmorphology exams and neurobehavioral testing and maternal risk interviews. CoFASP consent rates ranged from 37% to 71% and averaged 59.9% (May, Chambers et al., 2018). Germane to this paper, the methods adopted by the CoFASP initiative were variations on case ascertainment and estimation techniques that were first employed in NIAAA-funded studies of FASD in South Africa (SA) (May et al., 2007, 2000; Viljoen et al., 2005). The SA FASD prevalence study methods evolved substantially over time, especially the: 1) diagnostic classification scheme and criteria for specific FASD diagnoses (Hoyme et al., 2016, 2005; Stratton et al., 1996), 2) a range of methods for estimating true prevalence, and 3) a weighted estimation technique derived from the proportion of FASD diagnosis in a sub-population of school children chosen randomly for the study (May et al., 2021c, 2017, 2016c, 2016a, 2013a).
The Current Study
Over the years the FASD epidemiologic study methods used in SA became well accepted for determining the prevalence of FASD and utility for advancing additional clinical and epidemiologic capabilities. The SA studies advanced the detailed description of the growth, physical dysmorphology (Hoyme et al., 2016), neurobehavioral traits of children across the continuum of FASD (Adnams et al., 2001; Kalberg et al., 2006; Kodituwakku et al., 2006), have contributed to understanding an array of maternal risk factors for FASD (May et al., 2013b, 2008).
The 2016-2017 study described in this manuscript represents the ninth cross-sectional community study of FASD conducted by the multi-disciplinary Fetal Alcohol Syndrome Epidemiology Research (FASER) team in the WCP of SA. Beginning in 1997 in another WCP town (May et al., 2000), a majority of the co-authors of this paper participated in the majority of the nine studies and in the communities reported here (May et al., 2013a). This article presents findings from the most recent cross-sectional study of a cohort of first grade children in public schools in this rural, agricultural population with the highest prevalence of FASD documented in the world (May et al., 2017, 2016a, 2013a). Detailed findings are presented from in-person, physical examinations, neurobehavioral testing and checklists completed on each child, and comprehensive maternal interviews. Furthermore, the methods for accessing, assessing, and diagnosing cases of FASD are presented, as are four techniques of prevalence estimates.
METHODS
Sampling and Recruitment: Tiers I and II
Figure 1 describes the sampling process and the number participants throughout the study. From 19 primary schools located in two rural towns and surrounding areas, written consent for children to participate was sought from parents/guardians of all 1st grade pupils (n=1158) enrolled in all public schools. Child assent forms were obtained from children seven years and older. Consent and assent were received for 888 (76.6%) of the enrolled school children. A three-tier process of screening was utilized for all child participants. In Tier I, all participants were measured for height, weight, and occipitofrontal (head) circumference (OFC). If a child were ≤25th centile on height or weight, and/or OFC, the child was automatically advanced to Tier II. Additionally, 475 children were picked randomly from all 1st grade students enrolled in the schools; 374 had consent to participate. All randomly-selected children were also advanced to Tier II regardless of size. Therefore, all small and all randomly-selected children were advanced to Tier II and received a dysmorphology exam from a research team pediatrician, fellowship-trained in clinical genetics/dysmorphology.
Figure 1.
Sampling Methodology for Prevalence of FASD in a Third Sample in South African Community
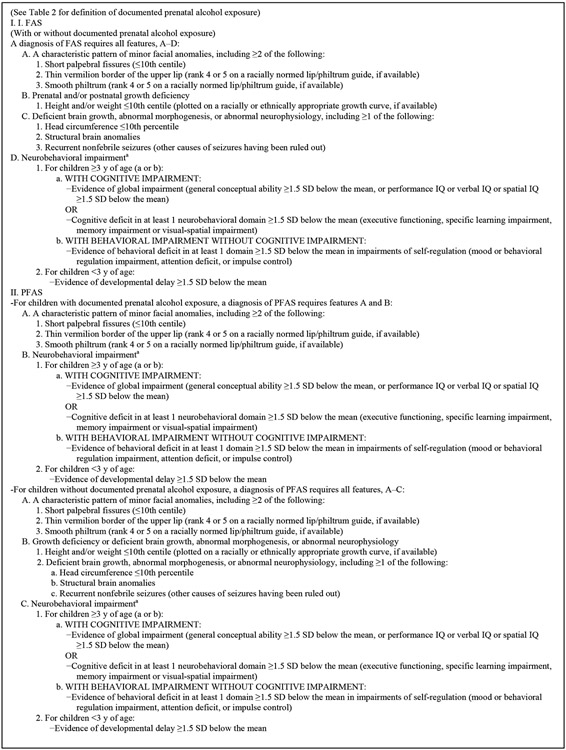
Institute of Medicine (IOM) Diagnostic Categories
The IOM diagnostic criteria of four FASD diagnoses were used in this study, and they are described in detail elsewhere (Hoyme et al., 2016) and summarized in Figure 2. Individuals with fetal alcohol syndrome (FAS) present with significant growth retardation (≤10th centile on height and/or weight), small OFC, at least two of the three cardinal facial features of FAS, and cognitive and/or behavioral impairment. Individuals with partial fetal alcohol syndrome (PFAS) display similar characteristics to those with FAS, but children with PFAS present with less growth restriction. The clinical dysmorphic traits of FAS and PFAS have been linked clearly with prenatal alcohol exposure (PAE) in multiple studies (Jones and Smith, 1973; May et al., 2013b, 2013d, 2011b; Stratton et al., 1996); therefore, these two diagnoses can be made by qualified pediatricians without direct documentation of PAE (Hoyme et al., 2016). In previous FASER studies in SA communities, few children were diagnosed with FAS or PFAS without direct or collateral evidence of PAE. Children with alcohol-related neurobehavioral disorder (ARND) do not have a characteristic pattern of cardinal FASD facial characteristics; therefore, direct evidence of PAE is required, and there must be strong evidence of cognitive and behavioral impairment documented by appropriate test results. The diagnosis of alcohol-related birth defects (ARBD) is for children with one or more major anomalies attributable to documented prenatal alcohol use, but the affected children do not have accompanying neurobehavioral problems outside of the normal range for the local population.
Figure 2.
Diagnostic Criteria for FASD. Reproduced with permission from Pediatrics, Vol. 138, Pages 3-4, Copyright © 2016 by the AAP
Assessment of Cognitive and Behavioral Traits - Tier III
All randomly selected children regardless of size or dysmorphology, and all children with significant features common to a diagnosis within FASD were advanced to Tier III for neurodevelopment assessment. Their teachers completed Achenbach Teacher Report Forms (TRF) (Achenbach and Rescorla, 2001) to evaluate inattention and behavioral issues. The Kaufman Assessment Battery for Children (KABC-II) (Kaufman and Kaufman, 2004) was administered to measure processing and cognitive abilities which result in a mental processing index (MPI) including measures of sequential processing, simultaneous processing, and learning. The KABC-II has been used in SA research and determined to be generally culturally fair (Skuy et al., 2000) and valid (Bangirana et al., 2009). The KABC was administered by blinded, South African contract educational psychologists and psychometrists, fluent in Afrikaans (the dominant regional language) and English. Neurobehavioral testing was completed in the first language of the child. Only a few children were tested by a Xhosa-speaking psychometrist. In order to determine cut off levels for impairment, a frequency distribution of all neurobehavioral scores was constructed for all participants in the study. As per the criteria for an FASD diagnosis in the second Revised IOM diagnostic guidelines, children who were found to be 1.5 standard deviations below the mean were considered impaired (Hoyme et al., 2016). A KABC MPI score (≤7th centile) was used to determine deficit/neurobehavioral delay and qualified for a FASD diagnosis. The two Achenbach TRF scores (total behavior problems and total inattention problems) were scored as follows: total problem t-score ≥ 64 fell in the clinical range and an inattention t-score of ≥ 22 was in the clinical range.
Maternal Risk Factor Assessment: Proximal and Distal Variables - Tier III
In Tier III, mothers and/or legal guardians completed an in-person interview to assess risk factors for FASD. Proximal variables assessed were alcohol use by quantity, frequency, and timing, use of tobacco and other drugs during pregnancy. Timing of drinking was assessed for three months prior to pregnancy and each trimester. Alcohol information was ascertained using time-line-follow-back methods (Sobell et al., 2001, 1988), and questions were asked in a broader context of overall dietary intake (King, 1994). Distal variables of risk for an FASD birth were addressed within a general family history, and included manual measurement of the mother’s height, weight, OFC, calculation of BMI, a detailed childbearing history, and demographic and socioeconomic (SES) measures.
Review of Data Collected and Diagnostic Case Conferences
In formal, multidisciplinary case conferences, findings from each domain (growth, dysmorphology, cognitive/behavioral performance, and maternal risk factors) were reviewed by the research team members who participated in the exams, testing, and maternal interviews. Weighing all data and input from the multidisciplinary team, final diagnosis was made for each child by the dysmorphologists.
Statistical Analysis
Case control analysis compared FASD diagnostic groups and controls. Data were analyzed with SPSS (IBM, 2021). Statistical significance for nominal and ordinal level data was determined using chi-square. One-way analysis of variance (ANOVA) with Bonferroni-adjusted p-values (.05/n) was used for interval level data as provided in Tables 1, 2, 3, and 4 as a conservative correction for multiple comparisons, and post-hoc analyses were performed using Dunnett’s C for pairwise comparisons (α = .05) to control for alpha error (Type I, false positive). Binary logistic regression assessed the association between an FASD diagnosis and drinks per drinking day, alcohol with concurrent tobacco exposure, and alcohol exposure by trimester(s) of exposure.
Table 1.
Children’s Demographic, Growth, Cardinal FASD Variables, and Total Dysmorphology Score From South Africa with Post Hoc Analysis Summary: A Third Rural Sample
| All children1 (n=865) |
FAS (n=95) |
PFAS (n=64) |
ARND (n=77) |
Randomly- Selected Controls (n=213) |
||
|---|---|---|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | p-value | |
| Sex (% Male) | 48.3 | 44.2 | 51.6 | 57.1 | 45.1 | .243 |
| Age of child (in months) | 83.3 (6.1) | 87.6 (8.6) | 84.6 (6.7) | 84.9 (6.9) | 82.7 (4.5) | <.001C,F |
| Height (cm) | 117.0 (5.8) | 112.3 (4.8) | 115.6 (5.7) | 116.3 (5.3) | 118.2 (5.2) | <.001A,B,C,E |
| Height centile | -- -- | 4.4 (6.0) | 18.2 (21.5) | 22.8 (23.8) | 33.8 (26.0) | <.001A,B,C,E,F |
| Weight (kg) | 21.3 (4.1) | 17.7 (2.4) | 20.2 (3.3) | 20.9 (3.2) | 22.2 (4.2) | <.001A,B,C,E,F |
| Weight centile | -- -- | 2.9 (3.4) | 22.5 (24.4) | 24.3 (26.1) | 40.5 (30.0) | <.001A,B,C,E,F |
| Child's Body Mass Index (BMI) | 15.4 (2.1) | 13.8 (.8) | 15.1 (1.5) | 15.1 (1.6) | 15.9 (2.2) | <.001A,B,C,E,F |
| BMI centile of child | -- | 12.6 (14.2) | 37.5 (26.9) | 37.2 (28.4) | 48.9 (30.5) | <.001A,B,C,E,F |
| Occipitofrontal circumference (OFC) (cm) | 51.2 (1.7) | 48.8 (1.0) | 51.1 (1.2) | 50.8 (1.5) | 51.8 (1.5) | <.001A,B,C,E,F |
| OFC centile | -- -- | 3.3 (3.1) | 32.6 (24.3) | 28.4 (29.9) | 51.8 (29.9) | <.001A,B,C,F |
| OFC ≤3rd centile (%) | -- | 69.5 | 7.8 | 18.2 | 4.7 | <.001 |
| OFC ≤10th centile (%) | -- | 100.0 | 12.5 | 45.5 | 10.8 | <.001 |
| Palpebral Fissure Length (PFL) centile | -- -- | 6.1 (9.5) | 17.7 (17.5) | 29.0 (16.7) | 29.1 (18.9) | <.001A,B,C,D,E |
| PFL ≤3rd centile | 60.0 | 32.8 | 7.8 | 9.4 | <.001 | |
| PFL ≤10th centile | 82.1 | 46.9 | 13.0 | 18.3 | <.001 | |
| Smooth Philtrum (%)2 | -- | 82.1 | 90.6 | 14.3 | 25.4 | <.001 |
| Narrow Vermilion of the Upper Lip (%)2 | -- | 86.3 | 87.5 | 16.9 | 20.7 | <.001 |
| Total Dysmorphology Score3 | -- -- | 18.8 (3.0) | 13.4 (3.4) | 8.8 (3.8) | 7.6 (3.9) | <.001A,B,C,D,E |
All children with consent. All children column was excluded from statistical analyses.
Scores of 4 or 5 on South African Lip/Philtrum Guide (Hoyme et al, 2015).
Scores determined using Hoyme et al., 2005
Bonferroni-adjusted significance value for all Table 1 comparisons: p<.0038
Significant (p<.05) post-hoc Dunnett C comparisons between:
FAS & PFAS
FAS & ARND
FAS & Randomly-Selected Controls
PFAS & ARND
PFAS & Randomly-Selected Controls
ARND & Randomly-Selected Controls
Table 2.
Other Minor Anomalies of Children with FAS, PFAS, and ARND Compared to Randomly-Selected Controls: A Third Rural Sample in South Africa
| FAS (n=95) |
PFAS (n=64) |
ARND (n=77) |
Randomly- Selected Controls (n=213) |
p-value | |
|---|---|---|---|---|---|
| Maxillary Arc (cm) – Mean (SD) | 23.1 (.8) | 23.9 (1.0) | 23.9 (.8) | 24.4 (1.0) | <.001A,B,C,E,F |
| Mandibular Arc (cm) – Mean (SD) | 24.3 (1.0) | 25.1 (1.3) | 25.2 (1.0) | 25.6 (1.2) | <.001A,B,C,E,F |
| Inner Canthal Distance (ICD) centile – Mean (SD) | 52.0 (20.9) | 59.7 (21.9) | 58.1 (22.0) | 62.4 (20.9) | .001C |
| Inner Pupillary Distance (IPD) centile – Mean (SD) | 45.5 (23.7) | 60.6 (23.9) | 65.0 (21.9) | 70.5 (21.6) | <.001A,B,C,E |
| Outer Canthal Distance (OCD) centile – Mean (SD) | 19.6 (12.4) | 32.9 (19.8) | 40.0 (17.8) | 42.7 (21.3) | <.001A,B,C,E |
| Hypoplastic midface (%) | 85.3 | 73.4 | 67.5 | 61.0 | <.001 |
| Epicanthal folds (%) | 55.8 | 40.6 | 39.0 | 40.4 | .056 |
| Altered Palmer Creases (%) | 47.4 | 48.4 | 29.9 | 37.1 | .044 |
| Camptodactyly (%) | 13.7 | 7.8 | 10.4 | 4.7 | .048 |
| Heart Murmur (%) | 13.7 | 10.9 | 9.1 | 4.2 | .027 |
| Prognathism (%) | 13.7 | 10.9 | 6.5 | 4.7 | .037 |
| Ptosis (%) | 34.7 | 17.2 | 18.2 | 8.5 | <.001 |
Bonferroni-adjusted significance value for all Table 2 comparisons: p<.0042
Significant (p<.05) post-hoc Dunnett C comparisons between:
FAS & PFAS
FAS & ARND
FAS & Randomly-Selected Controls
PFAS & ARND
PFAS & Randomly-Selected Controls
ARND & Randomly-Selected Controls
Table 3.
Mean Scores on Developmental and Behavioral Indicators1 of Children with FAS, PFAS, and ARND Compared to Controls from Three Rural Communities in South Africa with Post Hoc Analyses
| FAS (n=95) |
PFAS (n=64) |
ARND (n=76) |
RS Controls (n=212) |
||
|---|---|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | p-value | |
| Global Percentile Rank | 2.8 (4.9) | 3.2 (2.5) | 3.3 (2.6) | 15.5 (18.8) | <.001C,E,F |
| Short Term Memory Percentile Rank | 14.7 (16.0) | 17.1 (14.1) | 19.4 (15.8) | 33.0 (23.5) | <.001C,E,F |
| Visual Processing Percentile Rank | 5.0 (10.2) | 8.0 (10.2) | 6.6 (7.7) | 18.0 (19.4) | <.001C,E,F |
| Long Term Storage and Retrieval Percentile Rank | 7.7 (11.9) | 7.3 (8.0) | 8.8 (10.7) | 20.7 (22.6) | <.001C,E,F |
| Planning Percentile Rank | 3.2 (5.9) | 5.3 (5.8) | 4.7 (6.2) | 17.2 (21.6) | <.001C,E,F |
| Number Recall Percentile Rank | 25.5 (22.9) | 31.4 (20.9) | 32.4 (24.5) | 44.1 (25.6) | <.001C,E,F |
| Word Order Recall Percentile Rank | 12.4 (14.4) | 13.1 (10.9) | 15.1 (12.8) | 26.6 (19.8) | <.001C,E,F |
| Conceptual Thinking Percentile Rank | 3.7 (6.6) | 5.1 (5.2) | 4.1 (5.4) | 15.6 (18.9) | <.001C,E,F |
| Triangles Percentile Rank | 8.8 (14.8) | 11.3 (14.6) | 10.6 (11.9) | 25.4 (23.8) | <.001C,E,F |
| Pattern Reasoning Percentile Rank | 8.8 (12.9) | 14.6 (14.6) | 12.5 (13.3) | 21.9 (19.7) | <.001C,E,F |
| Atlantis Percentile Rank | 9.8 (10.5) | 13.0 (10.7) | 13.5 (13.7) | 21.2 (18.6) | <.001C,E,F |
| Rebus Percentile Rank | 10.8 (18.6) | 8.5 (12.7) | 10.6 (15.5) | 26.5 (30.0) | <.001C,E,F |
| TRF Total Behavior Problems t-score | 58.6 (9.0) | 56.2 (7.6) | 55.3 (7.3) | 52.9 (5.4) | <.001B,C,E,F |
| TRF Total Inattention Problems t-score | 54.6 (11.6) | 54.2 (10.8) | 51.7 (11.2) | 47.9 (9.4) | <.001C,E,F |
All scores standardized for age of child at time of testing.
TRF: Teacher Report Form
Bonferroni-adjusted significance value for all Table 3 comparisons: p< 0.0036
Significant (p<.05) post-hoc Dunnett C comparisons between:
FAS & PFAS
FAS & ARND
FAS & Randomly-Selected Controls
PFAS & ARND
PFAS & Randomly-Selected Controls
ARND & Randomly-Selected Controls
Table 4.
Maternal Size, Demographic, Childbearing, and Drinking of Alcohol in South Africa: A Third Rural Sample
| FAS (n=95) |
PFAS (n=64) |
ARND (n=77) |
RS Controls (n=213) |
||
|---|---|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | p-value | |
| Maternal Size, Demographic, and Childbearing | |||||
| Maternal height (in cm) | 155.0 (5.9) | 155.6 (6.6) | 156.6 (6.0) | 159.2 (6.1) | <.001C,E,F |
| Maternal weight (in kg) | 58.5 (15.1) | 68.5 (20.9) | 71.3 (22.3) | 76.2 (19.8) | <.001A,B,C |
| Maternal OFC (in cm) | 54.6 (2.0) | 56.0 (3.1) | 55.5 (2.3) | 56.1 (2.7) | <.001A,C |
| Maternal Upper Left Arm Circumference (in cm) | 26.3 (4.5) | 29.0 (5.8) | 31.0 (7.9) | 30.6 (5.0) | <.001A,B,C |
| Maternal body mass index (BMI) | 24.4 (6.2) | 28.2 (7.8) | 29.0 (8.6) | 30.0 (7.4) | <.001A,B,C |
| # of years of school completed | 7.7 (2.6) | 9.2 (2.6) | 9.3 (2.3) | 10.0 (2.3) | <.001A,B,C |
| Household income (in Rand) | 5814 (3517) | 7612 (8077) | 6266 (4215) | 7494 (5313) | .047C |
| Gravidity | 3.6 (1.6) | 2.9 (1.7) | 3.0 (1.5) | 2.8 (1.4) | <.001A,B,C |
| Parity | 3.3 (1.6) | 2.6 (1.3) | 2.6 (1.4) | 2.5 (1.3) | <.001A,B,C |
| Child of Interest (COI) in birth order | 3.0 (1.7) | 2.2 (1.5) | 2.2 (1.3) | 2.1 (1.3) | <.001A,B,C |
| Age (years) when pregnant with COI | 28.5 (7.0) | 25.2 (6.1) | 25.3 (6.5) | 25.8 (6.9) | .004A,B,C |
| Aware of pregnancy with COI (weeks) | 12.4 (6.0) | 11.0 (5.6) | 14.3 (5.9) | 11.5 (5.9) | .002D,F |
| Alcohol Consumption | |||||
| 3 months before pregnancy, usual # of drinks per drinking day (DDD) | 7.1 (8.9) | 4.6 (5.0) | 7.2 (4.4) | 1.4 (3.1) | <.001C,D,E,F |
| Drank in 1st trimester (%) | 77.2 | 65.5 | 98.6 | 23.0 | <.001 |
| Usual number of DDD in 1st trimester | 6.9 (8.8) | 4.1 (4.4) | 7.1 (4.5) | 1.1 (2.8) | <.001C,D,E,F |
| Usual number of DDD in 1st trimester1 | 9.2 (9.1) | 6.3 (4.0) | 7.2 (4.4) | 4.9 (4.2) | .006C,F |
| Drank in 2nd trimester (%) | 60.0 | 32.8 | 73.0 | 10.7 | <.001 |
| Usual number of DDD in 2nd trimester | 5.3 (7.6) | 1.9 (3.3) | 4.7 (5.1) | 0.5 (2.3) | <.001A,C,D,E,F |
| Usual number of DDD in 2nd trimester1 | 9.4 (8.0) | 6.2 (3.0) | 6.7 (4.9) | 5.6 (5.2) | .048 |
| Drank in 3rd trimester (%) | 41.8 | 17.2 | 35.1 | 5.3 | <.001 |
| Usual number of DDD in 3rd trimester | 3.6 (6.5) | 0.6 (1.6) | 1.9 (3.9) | 0.2 (1.7) | <.001A,C,F |
| Usual number of DDD in 3rd trimester1 | 9.6 (7.5) | 4.3 (1.8) | 6.1 (4.8) | 5.4 (6.6) | .056 |
| Tobacco and Other Drug Use | |||||
| Used tobacco during pregnancy (% Yes) | 72.3 | 37.5 | 55.4 | 27.1 | <.001 |
| Used other drugs during pregnancy (% Yes) | 1.1 | 3.4 | 4.1 | 0.0 | .036 |
| Used other drugs in lifetime (% Yes) | 12.9 | 11.1 | 15.1 | 6.8 | .154 |
Significant (p<.05) post-hoc Dunnett C comparisons between:
FAS & PFAS
FAS & ARND
FAS & Randomly-Selected Controls
PFAS & ARND
PFAS & Randomly-Selected Controls
ARND & Randomly-Selected Controls
Drinkers only in that specific time period.
Bonferroni-adjusted significant values: demographic and childbearing: p≤.004; drinking variables: p≤.005; tobacco use and other drugs: p≤.025
The final FASD prevalence rates (by specific diagnosis) are presented in three sections and four columns of Table 5. Crude prevalence rates were calculated using two denominators: a) total students enrolled in the community schools (the lower bound) and b) total students with consent to participate in the study. Two other techniques were applied: c) prevalence of FASD cases among the randomly-selected entrants to the study over the total number selected randomly and d) weighted prevalence employing simple projection of the proportion of each specific diagnosis identified in randomly-selected entrants to the number of children who did not receive consent to enter the study. This last, weighted rate (d) is considered the true prevalence of FASD. More description of methods is presented elsewhere (May, Chambers et al., 2018).
Table 5.
Prevalence Rates (per 1,000) of Individual Diagnoses within Fetal Alcohol Spectrum Disorders (FASD) and Total FASD by Three Methods of Estimation from a Third Rural Sample in South African Communities
| Oversample of children ≤ 25th centile on height, weight, or OFC |
Random Sample Rate of FASD Diagnoses and Estimated Cases in the Non-Consented Children |
(c) Estimated ARND cases in small children screened negative for FAS or PFAS (n=124) |
Combined rate from cases: a) in consented sample (n=1433) and b) estimated cases in non-consented sample (n=600) and c) small children not followed in Tier III |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Diagnosis | (a) Total Cases Diagnosed n |
School Enrollment rate1 (n=1158) |
Consented student rate2 (n=888) |
Cases found among randomly- selected control candidates n |
Proportion of FASD cases in random sample (n=336) |
(b) Estimated cases in non- consented sample (n=270) |
Rate of FASD from random sample only3 |
95% Confidence Intervals |
(a + b+ c) Total diagnosed and estimated cases n |
Final estimated rate for all enrolled students4 |
95% Confidence Intervals |
|
| FAS | 95 | 82.0 | 106.9 | 32 | 0.09524 | 26 | 95.2 | 63.9 - 126.6 | 0 | 121 | 104.5 | 86.9 - 122.1 |
| PFAS | 64 | 55.3 | 72.1 | 32 | 0.09524 | 26 | 95.2 | 63.9 - 126.6 | 0 | 90 | 77.7 | 62.3 - 93.1 |
| ARND | 77 | 66.5 | 86.7 | 58 | 0.17262 | 47 | 172.6 | 132.2 - 213.0 | 21 | 145 | 125.2 | 106.2-144.3 |
| ARBD | 2 | 1.7 | 2.3 | 1 | 0.00298 | 1 | 2.9 | 0.0 - 8.8 | 0 | 3 | 2.6 | 0.0 - 5.5 |
| Total FASD | 238 | 205.5 | 268.0 | 123 | 0.36607 | 100 | 366.1 | 314.6 - 417.6 | 21 | 359 | 310.0 | 283.4-336.7 |
Denominator is all children attending first grade in local schools. Rate per 1,000 based on the entire enrollment in 1st grade classrooms (n=1158).
Denominator is the total number of children with consent to participate in this study. Rate per 1,000 based on the sample consented and screened (n=888).
Calculated as the FASD cases diagnosed from the randomly-selected control candidates (numerator) over total number of randomly-selected children (n=336) x 1,000.
Rate per 1,000 children was calculated from the FASD cases diagnosed in the consented sample (a), added to the estimated cases in the non-consented sample utilizing the proportional diagnostic distribution of FASD cases among randomly-selected children (b), added to the estimated cases of ARND in the small children who were neither FAS nor PFAS nor randomly-selected and therefore not tested in Tier III (c) and divided by all 1st grade children enrolled in the schools (n=1158).
RESULTS
Child Physical and Demographic Traits
In Table 1 the demographic, growth, cardinal FASD features, and total dysmorphology scores are presented. Except for the sex of the children, all variables were significantly different overall (p<.001) on ANOVA between the four groups. Children with an FASD, especially those with FAS, were older on average than the controls. This is usually due to lack of progress in mastering learning tasks required for promotion to 2nd grade. Height, weight, and BMI were age- and sex-adjusted using CDC norms, and each measure was found to be lower for children with FASD than for controls. This is consistent with standard diagnostic criteria for FAS but not necessarily for children with PFAS and ARND. OFC was smallest, on average, for children with FAS, and lower in all other diagnoses of FASD than for the controls. Seventy percent of the children with FAS had true microcephaly (≤3rd centile), along with 7.8% and 18.2% of children with PFAS and ARND; 45.5% of children with ARND had OFC ≤10th (Figure 3).
Figure 3.
Average Occipitofrontal (head) Circumference (OFC) by Measurement (cm) and Age-specific Percentile by Diagnostic Category for a Third Sample in Three Rural South African Communities
Sex-specific comparisons were also calculated, and these data are found in Supplemental Table S1. Comparing males with FASD with male controls and females with FASD to female controls, all centile means were significantly lower (p<.001) for children with FASD.
The three cardinal features of FAS are presented in Table 1. For palpebral fissure length (PFL - eye openings) the age-adjusted centile measurements were lower for children with FASD than controls. By definition, more children with FAS and PFAS had a smooth philtrum and narrow vermilion border of the upper lip than controls. Children with ARND were exceptions, for a lower percent of them had these features than the controls. The mean total dysmorphology scores for all groups were significantly different, and formed a continuum from highest in the children with FAS (18.8), then children with PFAS (13.4), and ARND (8.8), and lowest among controls (7.6) (Figure 4). Furthermore, in post-hoc analysis, individual, bivariate comparisons of group mean dysmorphology scores were significantly different for all comparisons except ARND vs. controls. Also different for each of the group post hoc comparisons were PFL centile means except for ARND vs. controls. One other notable post hoc comparison was that growth measurements (weight, BMI, and OFC) were significantly different across all groups except for PFAS and ARND. Children with ARND were significantly smaller than controls.
Figure 4.
Total Dysmorphology Score of FASD Diagnostic Groups and Normal Controls in Four Rural South African Communities:
A Third Sample
*Significant (p<.05) post-hoc Dunnet C Comparison was significantly different between diagnostic groups.
Error bars = +/− 1 SE
Other Minor Anomalies
Other minor anomalous traits are in Table 2 for children with each of the three FASD diagnosis and for controls. Children with FASD were all significantly different from controls at the Bonferroni-adjusted value (p<.0042): maxillary and mandibular arcs, inner canthal distance (ICD), inner pupillary distance (IPD), outer canthal distance (OCD), and clinical observations of hypoplastic midface and ptosis of the eyelids. Approaching significance were: altered palmar creases, camptodactyly, prognathism, and heart murmur. Finally, epicanthal folds were not statistically different as measured by chi-square. Post-hoc, bi-variate analysis revealed a statistically significant difference among each of the groups on both maxillary and mandibular arcs except for PFAS vs. ARND. Notably, these arc measurements differentiated the group with ARND from controls. Furthermore, IPD and ICD differentiated groups in four bivariate comparisons.
Developmental and Behavioral Traits
Table 3 presents case control comparison of the cognitive, behavioral, and neurodevelopmental traits of the children. Results indicated outstanding consistency on percentile rank of every variable of the KABC. Children with each of the FASD diagnoses performed more poorly than controls on: Global Mental Processing (MPI); Sequential Processing (short term memory visual processing, long term storage and retrieval of information, planning, number recall, and word order recall); Simultaneous Processing (conceptual thinking, triangles, pattern reasoning); and Learning (Atlantis and Rebus). The Atlantis subtest requires the child to point to the correct picture of underwater fish and objects when the evaluator asks him/her to do so shortly after being taught the objects. In the Rebus subtest, the evaluator teaches the child a concept associated with a drawing, and the child is to read the phrases and sentences that are created by these drawings. Both subtests measure a child’s ability to learn a new task. Children with FAS performed more poorly than children in other diagnostic categories of FASD, and all FASD diagnostic groups performed significantly worse than controls on all ANOVA comparisons and post hoc comparisons.
The Teacher Report Form variables clearly in distinguished children with FASD from controls. On Total Behavior Problems and Total Inattention Scores, the children with FASD had more problems as in previous evaluations of children in this SA context (May et al., 2021c, 2016c, 2016a).
Distal Maternal Risk: Body Size, Childbearing, and Demographic
Distal and proximal maternal risk for FASD are presented in Table 4. Distal measures of maternal height, weight, OFC, upper arm circumference, and BMI were, without exception in the ANOVA comparisons, lower among mothers of children with FASD. Post-hoc, bivariate analysis indicated that mothers of children with FAS were shorter than mothers of controls, they were lighter, and had lower BMI (24.4) than mothers of PFAS, ARND, and the controls (28.2–30.0). Mothers of children with PFAS and ARND, however, did not differ significantly in weight and BMI from one another or from controls.
Two measures of socioeconomic status (SES) in Table 4 indicated that mothers of children with FASD were more frequently of lower SES as measured by maternal education, and household income, although this income difference did not reach Bonferroni-adjusted significance. Bivariate data indicated that the mothers of children with FAS were significantly lower in formal education (7.7 years) than mothers of all other groups (PFAS, ARND, and controls). Mothers of children with FAS were from significantly lower income households than controls.
The five variables characterizing childbearing history indicated that mothers of children with FASD (especially FAS) had significantly different childbearing experience than mothers of controls. Bivariate analysis indicated that mothers of children with FAS were significantly higher in gravidity, parity, and older when pregnant with the index child. Children with FAS were significantly later in the birth order (3.0) than children in the other three categories (PFAS and ARND=2.2 and controls=2.1).
Proximal Maternal Risk: Alcohol and Tobacco Consumption
Mothers of typically-developing controls reported drinking in the first trimester (23%), 10.7% in the second, and 5.3% in the third. But a significantly higher percentage of mothers of FAS, ARND, and PFAS reported drinking more than control mothers in each trimester. Additionally, mothers of children with any FASD drank more per drinking day than mothers of control children who all of were developing within normal parameters for this population. In the first trimester, 98.6% of mothers of children with ARND reported drinking 7.2 drinks per drinking day (DDD), 77.2% of mothers of children with FAS reported drinking 9.2 DDD, and 65.5% of mothers of PFAS children reported drinking 6.3 DDD. Differences in timing of drinking and DDD existed among the mothers of the three FASD diagnostic groups. A higher percentage of mothers of children with FAS drank and drank greater quantities per drinking day (9.2–9.6) throughout pregnancy. Mothers of children with PFAS did most of their drinking in first trimester and then tapered off steadily in the second and third trimester to where 17.2% were drinking 4.3 DDD in third trimester. Mothers of children with ARND were the most likely to report drinking at a high level in the first (98.6% at 7.2 DDD) and second trimesters (73.0% at 6.7 DDD), but in the third trimester 35.1% reported drinking at a usual level of 6.1 DDD.
Tobacco and other drug use in Table 4 indicates that mothers of children of all diagnostic categories of FASD were more likely to use tobacco during index pregnancies than were mothers of controls. The highest use was reported by mothers of children with FAS (72.3%), and the lowest among mothers of controls (27.1%). Other drug use during pregnancy was not significantly different among the groups and was lowest (zero) among controls, respectively lower among mothers of children with FAS (1.1%), PFAS (3.4%), and ARND (4.1%). Lifetime use of other drugs was not significantly different for the maternal groups, but was highest for mothers of children with ARND (15.1%), then FAS, PFAS, and controls (6.8%).
Prevalence of Each Specific FASD Diagnosis and Total FASD
Table 5 presents a tally of the cases of FASD diagnosed in this study and four estimates of the prevalence of each specific diagnosis of FASD in these communities. The first and second simple techniques utilize two different denominators and the total number of cases as the numerator. There were 238 children diagnosed with an FASD in this cohort: 95 with FAS, 64 with PFAS, 77 with ARND, and 2 with ARBD (column “a” in Table 5). Using the total number of children enrolled in this school cohort (n=1158) as the denominator, the rate of FASD was 205.5 per 1,000. This is the lowest (‘lower bound’) estimate that can be calculated from the results. If the denominator of only the consented children were used (n=888), the rate of total FASD was 268.0 per 1,000.
If one used a third, basic technique and estimated the prevalence from only the random sampling in this study, the highest of the estimates was produced (middle section of Table 5). There were 123 children with an FASD diagnosed within the random sample entrants (n=336). The total prevalence of FASD from the random sample entrants was therefore (123/336 = 0.36607 x 1,000) 366.1 children with FASD per 1,000 (95%CI= 314.6-417.6).
Proportions of the prevalence of each diagnosis within the random sample were also used to produce the fourth estimate which corrects for cases missed in the cohort due to no consent to participate in the study. The number of children with an FASD that would likely have been present among the non-consented children (n=270) in the entire first-grade cohort was estimated from the random sample results and added to the numerator. Therefore, the fourth estimate utilized these proportional correction values to estimate the total number of cases likely to exist among unconsented children (column “b”) and to estimate the probable ARND cases among small children (≤25th centile) who were neither selected randomly nor tested for neurobehavioral problems (column “c”). Thus, this estimate of true prevalence was calculated from a numerator which was the sum of these columns in Table 5: (a) the actual number of cases diagnosed in the consented sample, (b) the FASD cases estimated to be in the non-consented sample, and (c) the estimated ARND cases among entrants to the study because of small size who received only dysmorphology exams and were not tested for neurobehavior. Therefore, the final calculation used the sum of cases in columns a + b + c as the numerator (n=359), and the denominator was all 1st grade children in these schools (n =1158). This last technique yielded estimates of the prevalence of: FAS- 104.5 per 1,000, PFAS- 77.7 per 1,000, ARND- 125.2 per 1,000, and ARBD- 2.6 per 1,000. Total FASD using this technique was estimated as 310 per 1,000 (95%CI = 283.4–336.7), or 31% when expressed as a percentage.
Regression Analysis: The Likelihood of an FASD Diagnosis
In Table 6, adjusted binary logistic regression provided estimates of the effects of alcohol, tobacco use, and two SES measures (monthly household income and years of formal maternal education) on the likelihood of an FASD diagnosis among the randomly-selected study entrants in this cohort. Prenatal alcohol consumption at the quantity and frequency levels described in the case control analysis data in Table 4 yielded a significant difference over that of abstaining mothers with an odds ratio (OR) of 16.5 (p<.001, 95%CI= 7.51–36.56). Smoking tobacco with no prenatal alcohol consumption was not a significant predictor of FASD. But, when tobacco and alcohol were both consumed at the level described in this population, odds increased to an OR of 19.0 (p<.001, 95%CI= 8.59–42.34). Household income was not associated with an FASD diagnosis, but maternal education level approached significance (.05<α<.10) and was negatively associated with FASD diagnosis (OR=0.508, p=.060, 95%CI = 0.25–1.03). The greater the formal education of a mother, the lower the likelihood of an FASD diagnosis.
Table 6.
Adjusted Binary Logistic Regression: Likelihood of an FASD Diagnosis by Alcohol and Tobacco Use During Pregnancy - Among Randomly-Selected Children Only (n=300)
| During Pregnancy | B | S.E. | Sig. | OR | 95% C.I. for OR | |
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| No Alcohol or Tobacco Use | 1 | -- | -- | |||
| Alcohol Only | 2.808 | .404 | <.001 | 16.570 | 7.510 | 36.556 |
| Tobacco Only | .916 | .501 | .067 | 2.499 | .936 | 6.671 |
| Alcohol and Tobacco Use | 2.948 | .407 | <.001 | 19.076 | 8.594 | 42.342 |
| Monthly Household Income (sqrt) | −.001 | .006 | .834 | .999 | .988 | 1.010 |
| Years of formal maternal education (sqrt) | −.678 | .360 | .060 | .508 | .250 | 1.029 |
| Constant | −.059 | 1.156 | .959 | .943 | -- | -- |
In Table 7, binary logistic regression was applied to predicting: A) the likelihood of an FASD diagnosis by quantity (number of drinks per drinking day – DDD) and B) gestational timing of drinking (by trimester). Covariates, prenatal tobacco use and maternal education, were also considered in these analyses. In part A) the odds of having a child with FASD were significantly greater for women who consumed 2 DDD than among mothers who abstain (OR=5.88, p=.002, 95%CI= 1.96– 7.67). The association increased with 3 DDD (OR=5.89) and was highest at 4 DDD (OR=38.27, p<.001, 95%CI = 9.85–148.64). At 5 or more DDD the odds dropped to OR= 19.79, probably due to under reporting of total drinks and the underreporting values clustered at 4 DDD. In this analysis, the sole use of tobacco was not significantly associated with the likelihood of an FASD diagnosis, but years of formal education of the mothers was significantly protective (p=.005) from a diagnosis (OR= 0.325) when DDD was considered.
Table 7.
Adjusted Binary Logistic Regression Predicting Odds of a FASD Diagnosis by Usual Drinks per Drinking Day in 1st Trimester and by Trimester: A Third Rural South African Sample - - Among Randomly-Selected Children Only
| Part A (n=302) | B | S.E. | Sig. | Odds Ratio |
95% C.I. for EXP (B) | |
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| Non-drinkers (referent group) | -- | -- | <.001 | 1.0 | -- | -- |
| 1 drink per drinking day | 1.269 | .772 | .100 | 3.557 | .783 | 16.158 |
| 2 drinks per drinking day | 1.772 | .561 | .002 | 5.882 | 1.957 | 17.673 |
| 3 drinks per drinking day | 1.774 | .735 | .016 | 5.893 | 1.394 | 24.905 |
| 4 drinks per drinking day | 3.645 | .692 | <.001 | 38.274 | 9.855 | 148.644 |
| 5+ drinks per drinking day | 2.985 | .382 | <.001 | 19.789 | 9.367 | 41.805 |
| Covariates | ||||||
| Used Tobacco (Yes) | .355 | .341 | .298 | 1.426 | .731 | 2.782 |
| Years of formal maternal education (sqrt) | -1.125 | .396 | .005 | .325 | .149 | .706 |
| Constant | 1.368 | 1.239 | .270 | 3.929 | -- | -- |
| Part B (n=311) | B | S.E. | Sig. | Odds Ratio |
95% C.I. for EXP (B) | |
| Lower | Upper | |||||
| Non-drinkers (referent group) | -- | -- | <.001 | 1.0 | -- | -- |
| 1st trimester | 2.126 | .364 | <.001 | 8.379 | 4.102 | 17.115 |
| 1st and 2nd trimester | 2.875 | .440 | <.001 | 17.726 | 7.476 | 42.030 |
| 1st, 2nd, and 3rd trimester | 2.925 | .458 | <.001 | 18.632 | 7.594 | 45.716 |
| Covariates | ||||||
| Used Tobacco (Yes) | .397 | .317 | .210 | 1.488 | .799 | 2.770 |
| Years of formal maternal education (sqrt) | −.758 | .357 | .034 | .469 | .233 | .943 |
| Constant | .259 | 1.130 | .819 | 1.296 | -- | -- |
Part B of Table 7 indicates that drinking in all three trimesters presented the greatest likelihood for bearing a child with FASD (OR=18.63, p<.001, 95%CI= 7.59–45.72). Drinking in first trimester only and both first and second trimester were also not good for the fetus. The odds ratio for first trimester drinking was 8.38 and 17.73 for first and second trimester drinking. In this analysis of timing of drinking, smoking and not drinking was not significantly associated with FASD, but higher level of maternal education was again protective for the (OR=0.47, p=.034, 95%CI= 0.233–0.943).
DISCUSSION
Diagnosis of FASD
Child trait results from this first grade cohort are indications of accurate diagnoses following the revised IOM guidelines (Hoyme et al., 2016), therefore providing confidence in the final prevalence figures. Virtually all case control comparisons of physical and neurobehavioral traits indicated highly significant differences between children with any FASD diagnosis and the children (controls) who were randomly selected for study entry and verified to be developing in a typical manner in this population. Furthermore, in many of the post-hoc, bivariate comparisons, significant differences among the specific FASD diagnostic groups were documented. The most significant findings differentiated FASD groups from one another. Especially notable were significant differences between children with ARND and the typically developing controls: weight, BMI, head circumference, and maxillary and mandibular arcs. Careful assessment of all physical and dysmorphology traits in Tables 1 and 2 aided differential diagnosis. And when used in combination with the neurobehavioral traits assessed in this study (Table 3), all enhance and enable identification of children on the full continuum of FASD.
The physical traits of FASD are mostly indicators of stunted growth and midface hypoplasia indicative of poor brain development. Other minor anomalies provide additional clues of poor brain growth and midface development (e.g. PFL, ICD, IPD, OCD, and maxillary and mandibular arcs), and stunted development (Abell et al., 2016; Gomez et al., 2020; Valentine et al., 2017). As illustrated well in this study, physical traits aid in the diagnosis of multiple categories of FASD (see also Carter et al., 2013; Jacobson et al., 2021), even when differentiating children with ARND from controls who may have been borderline in their neurobehavioral functioning in their younger years (Carter et al., 2016).
Neurobehavioral Measures and Traits
Significantly lower scores were recorded in children in all diagnostic categories of the FASD spectrum when compared to randomly-selected controls. The mean scores of children diagnosed with FAS, PFAS, and ARND were statistically lower for every subtest administered in the study. Comparing the mean scores of the control children versus the mean scores of the children diagnosed on the spectrum (regardless of significance) revealed remarkably lower scores overall among the affected children. Therefore, general mental ability, including measures of simultaneous and sequential processing and measures of learning (as measured by the KABC-II) fell significantly behind for the affected children. Similar results were demonstrated in two longitudinal cohorts of children in the SA population over time (Jacobson et al., 2021; Kalberg et al., 2019).
The Achenbach behavioral measures revealed that all groups of children, including randomly-selected controls, had mean inattention scores in the clinical range. This may indicate a pervasive incidence of inattention in this population, with inattention being even more marked in children on the FASD continuum. While mean scores for total behavior problems were significantly different between affected and control children, all fell within the average range for that test.
Maternal Risk: Quantity, Frequency, and Timing of Alcohol Use and Other Drug Use
The pattern of quantity, frequency, and timing of maternal drinking varies among the mothers of children with the various diagnoses of FASD. Binge drinking (defined by NIAAA as 4 drinks per occasion for females (NIAAA, n.d.), and 3 or more in our studies of FASD in this population (May et al., 2008), has once again proven to be the most common pattern of drinking that causes great risk to the fetus (Livy et al., 2003; Maier et al., 1999, 1997). Mothers of children with FASD in this population binge drink more per drinking day than mothers of children who are developing within normal parameters (see also: Carter et al., 2022; Fletcher et al., 2018; Watt et al., 2017). Not only were mothers of children with FAS very heavy and frequent drinkers who were likely to drink throughout pregnancy, but mothers of children with ARND also showed a similar pattern. However, there was a tendency for mothers of children with ARND to report quitting drinking in the final trimester and to be younger during the index pregnancy. In the first trimester, 98.6% of mothers of children with ARND reported drinking an average of 7.2 drinks per drinking day (DDD), 77.2% of mothers of children with FAS reported drinking and average of 9.2 DDD, and 65.5% of mothers of PFAS children reported drinking 6.3 DDD. Affecting the higher frequency of drinking among mothers of children with ARND, is that the diagnosis of FAS and PFAS can be made without direct reports of prenatal drinking in the index pregnancy, whereas the diagnosis of ARND cannot be made at all without direct evidence of substantial alcohol exposure (Hoyme et al, 2016). Differences in timing and quantity (DDD) of drinking existed among the mothers of the three FASD diagnostic groups. A higher percentage of mothers of children with FAS reported drinking greater quantities per drinking day (9.2 – 9.6) throughout pregnancy. Mothers of children with PFAS did most of their drinking in the first trimester and then tapered off in second and third trimesters to the point where 17.2% were drinking 4.3 DDD in third trimester. Mothers of children with ARND were the most likely to report drinking at a very high level in the first (98.6% at 7.2 DDD) and second trimesters (73.0% at 6.7 DDD), but reducing in the third trimester to 35.1% drinking at a usual level of 6.1 DDD.
Risk for FASD: Alcohol and Tobacco, Daily Consumption Pattern, and Timing by Trimester
Use of tobacco (hand rolled cigarettes) during pregnancy was high for all mothers in the study. Tobacco use was highest for mothers of children with FAS (72.3%) and co-morbid alcohol and tobacco use was a significant proximal risk factor for FASD in this study, a finding common to other studies in other populations (Cogswell et al., 2003; McQuire et al., 2020). Use of alcohol alone produced an odds ratio of 16.6 for a diagnosis on the FASD continuum over that of a mother who abstained during pregnancy. And although the use of alcohol alone and tobacco alone during pregnancy was not statistically significantly different among the four groups of mothers, the simultaneous use of these two teratogens ranged from 27.1% among mothers of controls, to 55% in those of children with PFAS, to 72.3% in mothers of children with FAS. The odds ratio associated with an FASD was highest at 19.1 for those mothers com-morbid use of alcohol and tobacco during pregnancy.
Drinks per drinking day (DDD) has proven to be a useful measure of binge drinking in multiple studies in the US and SA. Two DDD is the lower bound (threshold) for an FASD in this SA, predominantly mixed-race population, whereas 3 DDD has been shown to be the threshold in US population studies (May et al., 2022). The modal frequency of drinking in both the SA and US studies is two days per week. Undernutrition and low body weight/mass may influence the greater significance of the lower threshold in this SA population (Carter et al., 2022, 2017; Hasken, 2021; May et al., 2016b, 2014b).
As the case control data have shown in this sample, trimester of drinking differs across FASD diagnoses. But when all diagnoses are considered together, the association with any diagnosis of an FASD is greatest when drinking occurs throughout pregnancy (OR=18.6) compared to that of abstainers. Drinking in the first and second trimesters indicated a very high-risk pattern (OR= 17.7). Drinking only in the first trimester and quitting in the final two trimesters was not without risk, for the odds of a child with FASD were associated with 8.4 times greater risk than with prenatal abstention.
Prevalence of Total FASD and Change in Prevalence of Specific Diagnoses Over Time
This was the third population-based, active case ascertainment study carried out in this region of the Western Cape Province. Each of these cross-sectional studies used identical methods and techniques of sampling, diagnosis, and maternal risk assessment. In 2009-2010 the rates of total FASD were estimated slightly more conservatively than in subsequent studies, yielding a range of estimated rates of 18–26%. In 2011-2012 the range of estimated total FASD rates was 20–28%, and the range in the current study was 20–31%. Therefore, the rates of total FASD were relatively constant.
Change in the mix of FASD diagnoses occurred in this region, for there was a lower proportion of FAS cases diagnosed in this sample, and a higher proportion of the less severe cases (PFAS and ARND). This was demonstrated in both specific diagnostic percentages and case ratios. As our diagnostic systems and specificity of criteria gained in sensitivity and accuracy across the continuum of FASD, the percentage of FAS cases (the most seriously affected children) within the total FASD continuum dropped significantly over time (2009 – 2016). FAS diagnoses accounted for 49.1% of all diagnoses in Sample I, 46.9% in sample II, and dropped to 33.7% in this third sample (z = 4.56, p<.001) (Figure 5). The case ratios of other FASD diagnoses (PFAS/ARND) to FAS also reflected this significant change (Figure 6). There were 1.04 cases of other FASD to every case of FAS in Sample I, 1.13 other cases in Sample II, and 1.94 cases of other FASD diagnoses to each case of FAS in Sample III. Therefore, the severity of the cases of FASD dropped overall within the continuum, for in Sample I there was one case of other FASD diagnoses for every case of FAS, and by Sample III there were approximately two cases of other FASD to each case of FAS. Part of this significant ratio change is explained by a doubling of diagnosed and estimated cases of children with ARND from sample I to Sample III (z = 7.34, p<.001). Another component of this change was a significant drop in the proportion of children with PFAS from 33.3% and 34.8% in Samples I and II to 25.1% in Sample III (z = 2.61, p=.009). While this pattern of change in diagnoses is clearly reflected in the data, it may or may not be proof of successful prevention. An optimist might attribute this change in severity of diagnoses to nine years of wide dissemination of messages to prevent FASD. This messaging that alcohol and pregnancy do not mix may have lowered the prevalence of FAS, and therefore, declare it as a victory. On the other hand, a more skeptical person might discount the change to higher rates of ARND as not much of a change or improvement at all for children with ARND in this sample were not without many problems themselves. They also performed significantly worse than controls on most every neurobehavioral measure, as did the children with FAS and PFAS. Regardless of the interpretation one might choose, the trend in severity of diagnosis is in a positive direction. Children with an FASD were exhibiting better physical growth and development in this third study which may indicate fewer cases of what Jacobson et al (2021) referred to as the “strong phenotype” that persisted over time and more cases of “a less consistent” phenotype where the “physical phenotype was most apparent during early childhood” and diminished during puberty. Children with the less consistent phenotype often exhibit better neurobehavior than those with the strong phenotype (e.g., FAS) as they age (Carter et al., 2016; Jacobson et al., 2021).
Figure 5.
Proportional Distribution of Fetal Alcohol Spectrum Disorders (FASD) Diagnoses
Figure 6.
Case Ratio: Total Cases of Partial Fetal Alcohol Syndrome (PFAS) and Alcohol-Related Neurodevelopmental Disorder (ARND) per Case of Fetal Alcohol Syndrome (FAS)
Strengths and Limitations
The fact that this is the third population-based study in this region with similar methods employed in, enables monitoring of prevalence and changes over time. First, as this manuscript has shown, total FASD rates are consistent over time, for gross patterns of alcohol consumption have not changed dramatically in this population. Drinking remains an entrenched behavior among a substantial portion of women of childbearing age (e.g., weekend binge drinking) (May et al., 2019). Second, data produced in these studies have provided findings and insights into more than the prevalence of FASD. Also studied in detail were physical and behavioral traits of children with FASD and comparison of those of developing typically in this region. Maternal risk for FASD was studied from both proximal and distal factors leading not just to understandings of associations with maternal drinking, but with multiple variables that are significantly associated with an FASD. Therefore, they may be especially useful for understanding preventive applications and interventions for children. Third, comprehensive clinical epidemiological studies such as this one identify significant and innovative patterns which provide insights to guide intervention and prevention in local clinics and communities. Fourth, one example of the utility of these findings is that multifaceted case management (MCM) has been shown to work as indicated prevention of FASD (de Vries et al., 2015; May et al., 2013c), but it is intensive in labor, costs, and resources. Fifth, more sophisticated neurobehavioral testing was employed in this study than in most of our previous cross-sectional prevalence studies in SA, and these results provided better information for improved diagnostic assessment and better guidance for enhancing development for individual children.
There were weaknesses in this study. First, it would have been beneficial to have used more sophisticated cognitive and neurobehavioral tests in the first two samples in this sub-region. It would have enabled better monitoring of neurobehavioral the trends over time. But limited time, resources, and manpower available for the first two studies did not permit this. Second, the observations made, and methods used, for clinical assessment, especially in the diagnostic category of ARND, evolved and improved during the decade of the studies. While this will ultimately benefit many children via accurate assessment and diagnosis, interpretation of the trends in FASD prevalence found here is more complex. Third, the consent rate of 77% is not the highest rate we have ever obtained in similar studies in the Western Cape Province, but it is significantly higher than generally obtained in other studies, particularly in more developed countries and communities such as the US (May et al., 2018), Canada (Popova et al., 2019), Italy (May et al., 2011a), and elsewhere in Europe (May et al., 2021b; McCarthy et al., 2021; Okulicz-Kozaryn et al., 2017; Petkovic and Barisic, 2013, 2010).
Implications for Other Populations
Some scholars and public health researchers might say that the findings regarding maternal risk and child diagnostic traits from SA may not be applicable to other populations. The FASER team authors have even said and written about a possible lack of applicability to other, more highly-developed populations. But over the years, especially in recent studies in the United States, evidence of their general applicability has emerged. Many of the same maternal risk factors, both proximal and distal, have now been found in the US and Italy (Ceccanti et al., 2014; McQuire et al., 2019), but their relevance, strength, and significance often differ by degree. Furthermore, with some variance by ethnic and racial physical phenotypes, a majority of the hallmark child traits of the continuum of FASD are also found in the USA and Europe (Chambers et al., 2019; May et al., 2022). Therefore, we now believe that the epidemiology and developmental findings from SA are broadly applicable to other populations.
CONCLUSIONS
The final prevalence of FAS was 104.5 per 1,000 or 10.5 %, and total FASD prevalence was 310 per 1,000 or 31%. FASD continued as significant problems in this rural region, nine years after the first of three cohort studies was initiated. But the severity of physical traits and diagnoses within the continuum of FASD are trending downwards. The likelihood of a diagnosis of an FASD is associated with co-morbid, prenatal use of alcohol and tobacco. Maternal drinking of two or more drinks per drinking day is also significantly associated with an FASD diagnosis as is drinking in first, second, or all trimesters.
Supplementary Material
Acknowledgements
Funding was provided by the National Institute on Alcohol Abuse and Alcoholism (NIAAA) (UO1 AA15134). We thank the South African Western Cape Province Department of Education and teachers who approved the study and supported us and the children, all parents who gave permission for their children to participate in the study, children who participated in the study at each of the schools, and all the mothers who provided information for the maternal risk portion of this study. We are especially indebted to the dedicated field staff members for this study. Project officers Carisa Siemens, Cecile Kriel, Marlene de Vries, Nerina Bester, Natalie Cronje, Belinda Joubert, Carolien Viljoen, and Cate Doms consistently applied their skills to interviewing and quality control of the data in all domains of the study. Florette Kamfer and Paula Hess exercised their talents to locating and transporting participants which were invaluable to the success of the entire project. The Educational Psychologist, Lynette Minnaar, and Psychometrist Carolien Viljoen applied their skills with diligence in the neurobehavioral testing of all the children in English and Afrikaans. Testing in Xhosa was completed by Rosy Khutelo. Andrea Engelbrecht, Suzelle Kruger, and Shumaya Uithaler carried out the logistics and data management for the study. Protocols and consent forms used were approved by the Institutional Review Boards of the University of New Mexico, the University of North Carolina, and the Ethics Committee of the Stellenbosch University, faculty of Medicine and Health Sciences.
REFERENCES
- Abell K, May W, May PA, Kalberg W, Hoyme HE, Robinson LK, Manning M, Jones KL, Abdul-Rahman O (2016) Fetal Alcohol Spectrum Disorders and Assessment of Maxillary and Mandibular Arc Measurements. Am J Med Genet A 170:1763–1771. [DOI] [PubMed] [Google Scholar]
- Achenbach T, Rescorla L (2001) Manual For The ASEBA School-Age Forms And Profiles. Burlington, VT, University of Vermont, Research Center for Children, Youth, and Families. [Google Scholar]
- Adnams CM, Kodituwakku PW, Hay A, Molteno CD, Viljoen D, May PA (2001) Patterns of Cognitive-Motor Development in children with Fetal Alcohol Syndrome from a Community in South Africa. Alcohol Clin Exp Res 25:557–562. [PubMed] [Google Scholar]
- Bangirana P, Seggane-Musisi, Allebeck P, Giordani B, Chandy CJ, Opoka OR, Byarugaba J, Ehnvall A, Boivin MJ (2009) A preliminary examination of the construct validity of the KABC-II in Ugandan children with a history of cerebral malaria. Afr Health Sci 9:186–192. [PMC free article] [PubMed] [Google Scholar]
- Carter RC, Georgieff MK, Ennis KM, Dodge NC, Wainwright H, Meintjes EM (2022) Prenatal Alcohol-Related Alterations in Maternal, Placental, Neonatal , and Infant Iron Homeostasis. Am J Clin Nutr 1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carter RC, Jacobson JL, Molteno CD, Dodge NC, Meintjes EM, Jacobson SW (2016) Fetal Alcohol Growth Restriction and Cognitive Impairment. Pediatrics 138:e20160775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carter RC, Jacobson JL, Sokol RJ, Avison MJ, Jacobson SW (2013) Fetal alcohol-related growth restriction from birth through young adulthood and moderating effects of maternal prepregnancy weight. Alcohol Clin Exp Res 37:452–462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carter RC, Senekal M, Dodge NC, Bechard LJ, Meintjes EM, Molteno CD, Duggan CP, Jacobson JL, Jacobson SW (2017) Maternal Alcohol Use and Nutrition During Pregnancy: Diet and Anthropometry. Alcohol Clin Exp Res 41:2114–2127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ceccanti M, Fiorentino D, Coriale G, Kalberg WO, Buckley D, Hoyme HE, Gossage JP, Robinson LK, Manning M, Romeo M, Hasken JM, Tabachnick B, Blankenship J, May PA (2014) Maternal Risk Factors for Fetal Alcohol Spectrum Disorders in a Province in Italy. Drug Alcohol Depend 145:201–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chambers CD, Coles C, Kable J, Akshoomoff N, Xu R, Zellner JA, Honerkamp-Smith G, Manning MA, Adam MP, Jones KL (2019) Fetal Alcohol Spectrum Disorders in a Pacific Southwest City: Maternal and Child Characteristics. Alcohol Clin Exp Res 43:2578–2590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cogswell ME, Weisberg P, Spong C (2003) Cigarette smoking, alcohol use and adverse pregnancy outcomes: Implications for micronutrient supplementation In: Journal of Nutrition . [PubMed] [Google Scholar]
- de Vries MM, Joubert B, Cloete M, Roux S, Baca BA, Hasken JM, Barnard R, Buckley D, Kalberg WO, Snell CL, Marais AS, Seedat S, Parry CDH, May PA (2015) Indicated Prevention of Fetal Alcohol Spectrum disorders in South Africa: Effectiveness of Case Management. Int J Environ Res Public Health 13:ijerph13010076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fletcher OV., May PA, Seedat S, Sikkema KJ, Watt MH (2018) Attitudes Toward Alcohol Use During Pregnancy Among Women Recruited from Alcohol-Serving Venues in Cape Town, South Africa: A Mixed-Methods Study. Soc Sci Med 215:98–106. [DOI] [PubMed] [Google Scholar]
- Gomez DA, May PA, Tabachnick BG, Hasken JM, Lyden ER, Kalberg WO, Hoyme HE, Manning MA, Adam MP, Robinson LK, Jones KL, Buckley D, Abdul-Rahman OA (2020) Ocular Measurements in Fetal Alcohol Spectrum Disorders. Am J Med Genet Part A 182:2243–2252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasken JM (2021) Maternal Body Mass Index and Diet as Protective Factors Against the Adverse Effects of Prenatal Alcohol Exposure. University of North Carolina. [Google Scholar]
- Hoyme HE, Kalberg WO, Elliott AJ, Blankenship J, Buckley D, Marais A-S, Manning MA, Robinson LK, Adam MP, Abdul-Rahman O, Jewett T, Coles CD, Chambers C, Jones KL, Adnams CM, Shah PE, Riley EP, Charness ME, Warren KR, May PA (2016) Updated Clinical Guidelines for Diagnosing Fetal Alcohol Spectrum Disorders. Pediatrics 138:e20154256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoyme HE, May PA, Kalberg WO, Kodituwakku PW, Gossage JP, Trujillo PM, Buckley DG, Miller JH, Aragon AS, Khaole N, Viljoen DL, Jones KL, Robinson LK (2005) A Practical Clinical Approach to Diagnosis of Fetal Alcohol Spectrum Disorders: Clarification of the 1996 Institute of Medicine Criteria. Pediatrics 115:39–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- IBM (2021) IBM SPSS Statistics for Windows. [Google Scholar]
- Jacobson SW, Hoyme HE, Carter RC, Dodge NC, Molteno CD, Meintjes EM, Jacobson JL (2021) Evolution of the Physical Phenotype of Fetal Alcohol Spectrum Disorders from Childhood through Adolescence. Alcohol Clin Exp Res 45:395–408. [DOI] [PubMed] [Google Scholar]
- Jones KL, Smith DW (1973) Recognition of the fetal alcohol syndrome in early infancy. Lancet 302:999–1001. [DOI] [PubMed] [Google Scholar]
- Kalberg WO, May PA, Buckley D, Hasken JM, Marais A-S, de Vries MM, Bezuidenhout Heidre, Manning MA, Robinson LK, Adam MP, Hoyme DB, Parry CD, Seedat S, Elliott AJ, Hoyme HE (2019) Early-Life Predictors of Fetal Alcohol Spectrum Disorders. Pediatrics 144:e20182141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalberg WO, Provost B, Tollison SJ, Tabachnick BG, Robinson LK, Eugene Hoyme H, Trujillo PM, Buckley D, Aragon AS, May PA (2006) Comparison of Motor Delays in Young Children With Fetal Alcohol Syndrome to Those With Prenatal Alcohol Exposure and With No Prenatal Alcohol Exposure. Alcohol Clin Exp Res 30:2037–2045. [DOI] [PubMed] [Google Scholar]
- Kaufman A, Kaufman N (2004) Kaufman Assessment Battery for Children. [Google Scholar]
- King AC (1994) Enhancing the self-report of alcohol consumption in the community: two questionnaire formats. Am J Public Health 84:294–296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kodituwakku PW, Adnams CM, Hay A, Kitching AE, Burger E, Kalberg WO, Viljoen DL, May PA (2006) Letter and Category Fluency in Children with Fetal Alcohol Syndrome from a Community in South Africa. J Stud Alcohol 67:502–509. [DOI] [PubMed] [Google Scholar]
- Livy DJ, Miller EK, Maier SE, West JR (2003) Fetal alcohol exposure and temporal vulnerability: Effects of binge-like alcohol exposure on the developing rat hippocampus. Neurotoxicol Teratol 25:447–458. [DOI] [PubMed] [Google Scholar]
- Maier SE, Chen W-JA, Miller JA, West JR (1997) Fetal alcohol exposure and temporal vulnerability: Regional differences in alcohol-induced microencephaly as a function of the timing of binge-like exposure during rat brain development. Alcohol Clin Exp Res 21:1418–1428. [DOI] [PubMed] [Google Scholar]
- Maier SE, Miller JA, Blackwell JM, West JR (1999) Fetal alcohol exposure and temporal vulnerability: Regional differences in cell loss as a function of the timing of binge-like alcohol exposure during brain development. Alcohol Clin Exp Res 23:726–734. [DOI] [PubMed] [Google Scholar]
- May PA, Baete A, Russo J, Elliott AJ, Blankenship J, Kalberg WO, Buckley D, Brooks M, Hasken J, Abdul-Rahman O, Adam MP, Robinson LK, Manning M, Hoyme HE (2014a) Prevalence and Characteristics of Fetal Alcohol Spectrum Disorders. Pediatrics 134:855–866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- May PA, Blankenship J, Marais A-S, Gossage JP, Kalberg WO, Barnard R, De Vries M, Robinson LK, Adnams CM, Buckley D, Manning M, Jones KL, Parry C, Hoyme HE, Seedat S (2013a) Approaching the Prevalence of the Full Spectrum of Fetal Alcohol Spectrum Disorders in a South African Population-Based Study. Alcohol Clin Exp Res 37:818–830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- May PA, Blankenship J, Marais AS, Gossage JP, Kalberg WO, Joubert B, Cloete M, Barnard R, De Vries M, Hasken J, Robinson LK, Adnams CM, Buckley D, Manning M, Parry CDH, Hoyme HE, Tabachnick B, Seedat S (2013b) Maternal Alcohol Consumption Producing Fetal Alcohol Spectrum Disorders (FASD): Quantity, Frequency, and Timing of Drinking. Drug Alcohol Depend 133:502–512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- May PA, Brooke L, Gossage JP, Croxford J, Adnams C, Jones KL, Robinson L, Viljoen D (2000) Epidemiology of Fetal Alcohol Syndrome in a South African Community in the Western Cape Province. Am J Public Health 90:1905–1912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- May PA, Chambers CD, Kalberg WO, Zellner J, Feldman H, Buckley D, Kopald D, Hasken JM, Xu R, Honerkamp-Smith G, Taras H, Manning MA, Robinson LK, Adam MP, Abdul-Rahman O, Vaux K, Jewett T, Elliott AJ, Kable JA, Akshoomoff N, Daniel F, Arroyo JA, Hereld D, Riley EP, Charness ME, Coles CD, Warren KR, Jones KL, Hoyme HE (2018) Prevalence of Fetal Alcohol Spectrum Disorders in 4 US Communities. J Am Med Assoc 319:474–482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- May PA, De Vries M, Marais A-S, Kalberg W, Buckley D, Adnams C, Hasken J, Tabachnick B, Robinson L, Manning M, Bezuidenhout H, Adam M, Jones K, Seedat S, Parry C, Hoyme H (2017) Replication of High Fetal Alcohol Spectrum Disorders Prevalence Rates, Child Characteristics, and Maternal Risk Factors in a Second Sample of Rural Communities in South Africa. Int J Environ Res Public Health 14:522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- May PA, de Vries MM, Marais AS, Kalberg WO, Adnams CM, Hasken JM, Tabachnick B, Robinson LK, Manning MA, Jones KL, Hoyme D, Seedat S, Parry CD, Hoyme HE (2016a) The Continuum of Fetal Alcohol Spectrum Disorders in Four Rural Communities in South Africa: Prevalence and Characteristics. Drug Alcohol Depend 159:207–218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- May PA, Fiorentino D, Coriale G, Kalberg WO, Eugene Hoyme H, Aragón AS, Buckley D, Stellavato C, Phillip Gossage J, Robinson LK, Jones KL, Manning M, Ceccanti M (2011a) Prevalence of Children with Severe Fetal Alcohol Spectrum Disorders in Communities Near Rome, Italy: New Estimated Rates Are Higher than Previous Estimates. Int J Environ Res Public Health 8:2331–2351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- May PA, Fiorentino D, Phillip Gossage J, Kalberg WO, Eugene Hoyme H, Robinson LK, Coriale G, Jones KL, del Campo M, Tarani L, Romeo M, Kodituwakku PW, Deiana L, Buckley D, Ceccanti M (2006) Epidemiology of FASD in a Province in Italy: Prevalence and Characteristics of Children in a Random Sample of Schools. Alcohol Clin Exp Res 30:1562–1575. [DOI] [PubMed] [Google Scholar]
- May PA, Gossage JP, Marais A-S, Adnams CM, Hoyme HE, Jones KL, Robinson LK, Khaole NCO, Snell C, Kalberg WO, Hendricks L, Brooke L, Stellavato C, Viljoen DL (2007) The Epidemiology of Fetal Alcohol Syndrome and Partial FAS in a South African Community. Drug Alcohol Depend 88:259–271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- May PA, Gossage JP, Marais A-S, Hendricks LS, Snell CL, Tabachnick BG, Stellavato C, Buckley DG, Brooke LE, Viljoen DL (2008) Maternal Risk Factors for Fetal Alcohol Syndrome and Partial Fetal Alcohol Syndrome in South Africa: A Third Study. Alcohol Clin Exp Res 32:738–753. [DOI] [PubMed] [Google Scholar]
- May PA, Hamrick KJ, Corbin KD, Hasken JM, Marais AS, Blankenship J, Hoyme HE, Gossage JP (2016b) Maternal Nutritional Status as a Contributing Factor for the Risk of Fetal Alcohol Spectrum Disorders. Reprod Toxicol 59:101–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- May PA, Hamrick KJ, Corbin KD, Hasken JM, Marais AS, Brooke LE, Blankenship J, Hoyme HE, Gossage JP (2014b) Dietary Intake, Nutrition, and Fetal Alcohol Spectrum Disorders in the Western Cape Province of South Africa. Reprod Toxicol 46:31–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- May PA, Hasken JM, Baete A, Russo J, Elliott AJ, Kalberg WO, Buckley D, Brooks M, Ortega MA, Hedrick DM, Tabachnick BG, Abdul-Rahman O, Adam MP, Jewett T, Robinson LK, Manning MA, Hoyme HE (2020a) Fetal Alcohol Spectrum Disorders in a Midwestern City: Child Characteristics, Maternal Risk Traits, and Prevalence. Alcohol Clin Exp Res 44:919–938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- May PA, Hasken JM, Bozeman R, Jones JV, Burns MK, Goodover J, Kalberg WO, Buckley D, Brooks M, Ortega MA, Elliott AJ, Hedrick DM, Tabachnick BG, Abdul-Rahman O, Adam MP, Jewett T, Robinson LK, Manning MA, Hoyme HE (2020b) Fetal Alcohol Spectrum Disorders in a Rocky Mountain Region City: Child Characteristics, Maternal Risk Traits, and Prevalence. Alcohol Clin Exp Res 44:900–918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- May PA, Hasken JM, Hooper SR, Hedrick DM, Jackson-Newsom J, Mullis CE, Dobbins E, Kalberg WO, Buckley D, Robinson LK, Abdul-Rahman O, Adam MP, Manning MA, Jewett T, Hoyme HE (2021a) Estimating the Community Prevalence, Child Traits, and Maternal Risk Factors of Fetal Alcohol Spectrum Disorders (FASD) from a Random Sample of School Children. Drug Alcohol Depend 227:108918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- May PA, Hasken JM, Manning MA, Hoyme HE (2021b) The challenges and pitfalls of fetal alcohol spectrum disorders prevalence studies. Alcohol Clin Exp Res 45:2468–2470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- May PA, Hasken JM, Marais A, de Vries MM, Kalberg WO, Manning MA, Hoyme HE (2022) Comparative Analysis of the Physical Traits of Children with Fetal Alcohol Spectrum Disorders in South Africa and the United States and the Likelihood of FASD Births In: Advances in Fetal Alcohol Spectrum Disorder (Chudley AE ed), New York, NY, Springer. [Google Scholar]
- May PA, Hasken JM, Stegall JM, Mastro HA, Kalberg WO, Buckley D, Brooks M, Hedrick DM, Ortega MA, Elliott AJ, Tabachnick BG, Abdul-Rahman O, Adam MP, Robinson LK, Manning MA, Jewett T, Hoyme HE (2020c) Fetal Alcohol Spectrum Disorders in a Southeastern County of the United States: Child Characteristics and Maternal Risk Traits. Alcohol Clin Exp Res 44:939–959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- May PA, Keaster C, Bozeman R, Goodover J, Blankenship J, Kalberg WO, Buckley D, Brooks M, Hasken J, Gossage JP, Robinson LK, Manning M, Hoyme HE (2015) Prevalence and Characteristics of Fetal Alcohol Syndrome and Partial Fetal Alcohol Syndrome in a Rocky Mountain Region City. Drug Alcohol Depend 155:118–127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- May PA, Marais A-S, Gossage JP, Barnard R, Joubert B, Cloete M, Hendricks N, Roux S, Blom A, Steenekamp J, Alexander T, Andreas R, Human S, Snell C, Seedat S, Parry CC, Kalberg WO, Buckley D, Blankenship J (2013c) Case Management Reduces Drinking During Pregnancy among High Risk Women. Int J Alcohol Drug Res 2:61–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- May PA, Marais AS, De Vries M, Hasken JM, Stegall JM, Hedrick DM, Snell CL, Seedat S, Parry CDH (2019) The dop system of alcohol distribution is dead, but it’s legacy lives on. Int J Environ Res Public Health 16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- May PA, Marais AS, De Vries MM, Buckley D, Kalberg WO, Hasken JM, Stegall JM, Hedrick DM, Robinson LK, Manning MA, Tabachnick BG, Seedat S, Parry CD, Hoyme HE (2021c) The Prevalence, Child Characteristics, and Maternal Risk Factors for the Continuum of Fetal Alcohol Spectrum Disorders: A sixth Population-Based Study in the Same South African Community. Drug Alcohol Depend 218:108408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- May PA, Marais AS, de Vries MM, Kalberg WO, Buckley D, Hasken JM, Adnams CM, Barnard R, Joubert B, Cloete M, Tabachnick B, Robinson LK, Manning MA, Jones KL, Bezuidenhout H, Seedat S, Parry CDH, Hoyme HE (2016c) The Continuum of Fetal Alcohol Spectrum Disorders in a Community in South Africa: Prevalence and Characteristics in a Fifth Sample. Drug Alcohol Depend 168:274–286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- May PA, Tabachnick BG, Gossage JP, Kalberg WO, Marais A-S, Robinson LK, Manning MA, Blankenship J, Buckley D, Hoyme HE, Adnams CM (2013d) Maternal Factors Predicting Cognitive and Behavioral Characteristics of Children with Fetal Alcohol Spectrum Disorders. J Dev Behav Pediatr 34:314–325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- May PA, Tabachnick BG, Gossage JP, Kalberg WO, Marais A-SS, Robinson LK, Manning M, Buckley D, Hoyme HE (2011b) Maternal Risk Factors Predicting Child Physical Characteristics and Dysmorphology in Fetal Alcohol Syndrome and Partial Fetal Alcohol Syndrome. Drug Alcohol Depend 119:18–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCarthy R, Mukherjee RAS, Fleming KM, Green J, Clayton-Smith J, Price AD, Allely CS, Cook PA (2021) Prevalence of fetal alcohol spectrum disorder in Greater Manchester, UK: An active case ascertainment study. Alcohol Clin Exp Res 45:2271–2281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McQuire C, Daniel R, Hurt L, Kemp A, Paranjothy S (2020) The Causal Web of Foetal Alcohol Spectrum Disorders: A Review and Causal Diagram. Eur Child Adolesc Psychiatry 29:575–594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McQuire C, Mukherjee R, Hurt L, Higgins A, Greene G, Farewell D, Kemp A, Paranjothy S (2019) Screening prevalence of fetal alcohol spectrum disorders in a region of the United Kingdom: A population-based birth-cohort study. Prev Med (Baltim) 118:344–351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism (NIAAA) (n.d.) What Is A Standard Drink? Available at: https://www.niaaa.nih.gov/alcohols-effects-health/overview-alcohol-consumption/what-standard-drink [Google Scholar]
- Okulicz-Kozaryn K, Borkowska M, Brzozka K (2017) FASD Prevalence among Schoolchildren in Poland. J Appl Res Intellect Disabil 30:61–70. [DOI] [PubMed] [Google Scholar]
- Petkovic G, Barisic I (2013) Prevalence of fetal alcohol syndrome and maternal characteristics in a sample of schoolchildren from a rural province of Croatia. Int J Environ Res Public Health 10:1547–1561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petkovic G, Barisic I (2010) FAS prevalence in a sample of urban schoolchildren in Croatia. Reprod Toxicol 29:237–241. [DOI] [PubMed] [Google Scholar]
- Popova S, Lange S, Poznyak V, Chudley AE, Shield KD, Reynolds JN, Murray M, Rehm J (2019) Population-based prevalence of fetal alcohol spectrum disorder in Canada. BMC Public Health 19:845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skuy M, Taylor M, O’Carroll S, Fridjhon P, Rosenthal L (2000) Performance of black and white South African children on the Wechsler intelligence scale for children-revised and the Kaufman assessment battery. Psychol Rep 86:727–737. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Agrawal S, Annis H, Ayala-Velazquez H, Echeverria L, Leo GI, Rybakowski JK, Sandahl C, Saunders B, Thomas S, Zioikowski M (2001) Cross-cultural evaluation of two drinking assessment instruments: alcohol timeline followback and inventory of drinking situations. Subst Use Misuse 36:313–331. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB, Riley DM, Schuller R, Pavan DS, Cancilla A, Klajner F, Leo GI (1988) The reliability of alcohol abusers’ self-reports of drinking and life events that occurred in the distant past. J Stud Alcohol 49:225–232. [DOI] [PubMed] [Google Scholar]
- Stratton K, Howe C, Battaglia F (1996) Fetal Alcohol Syndrome: Diagnosis, Epidemiology, Prevention, and Treatment. Washington DC. [Google Scholar]
- Valentine M, Bihm DCJ, Wolf L, Hoyme HE, May PA, Buckley D, Kalberg W, Abdul-Rahman OA (2017) Computer-Aided Recognition of Facial Attributes for Fetal Alcohol Spectrum Disorders. Pediatrics 140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Viljoen DL, Gossage JP, Brooke L, Adnams CM, Jones KL, Robinson LK, Hoyme HE, Snell C, Khaole NCO, Kodituwakku P, Asante KO, Findlay R, Quinton B, Marais A-S, Kalberg WO, May PA (2005) Fetal Alcohol Syndrome Epidemiology in a South African Community: A Second Study of a Very High Prevalence Area. J Stud Alcohol 66:593–604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watt MH, Knettel BA, Choi KW, Knippler ET, May PA, Seedat S (2017) Risk for Alcohol-Exposed Pregnancies Among Women at Drinking Venues in Cape Town, South Africa. J Stud Alcohol Drugs 78:795–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.