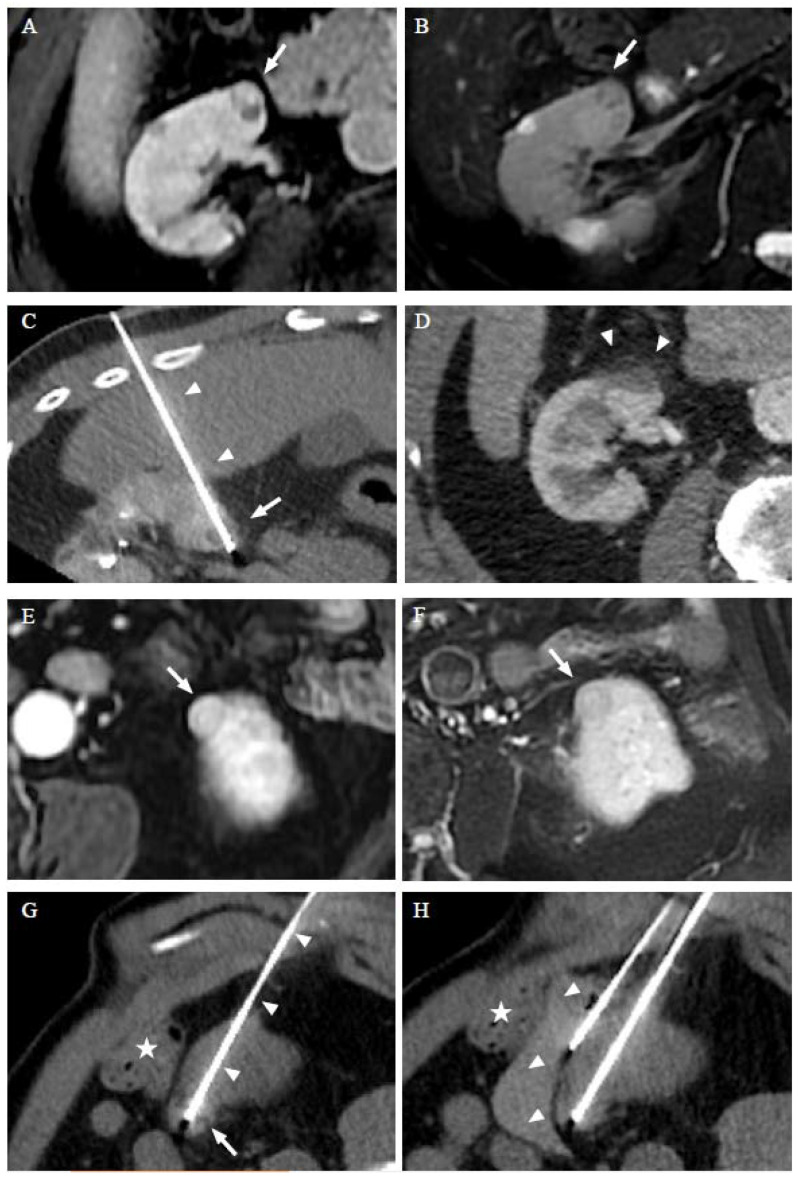
Figure 1.
RFA of a 68-year-old man with Birt–Hogg–Dubé syndrome who had a history of partial nephrectomy and presents two ccRCCs treated in two separate sessions. Dynamic axial T1w sequences with fat suppression after gadolinium injection (A) and axial T2w image with fat saturation (B) show the first ccRCC (arrow) treated. Computed tomography (CT) images in the axial plane obtained during the RFA show the transhepatic probe (arrowheads) into the lesion (arrow) (C). CT images in the axial plane on the follow-up 6 months later show a RFA scar (arrow) (D). Dynamic axial T1w sequences with fat suppression after gadolinium injection (E) and axial T2w image with fant saturation (F) show the second ccRCC (arrow) developed in the left kidney 26 months after the initial RFA session. CT images in the axial plane obtained during the 2nd session of RFA show the RFA probe (arrowheads) into two of the lesions (G), and hydrodissection with 60 cc of serum glucose 30% was performed to protect the colon (star) (H). The patient was alive with no local progression or distant metastasis 33 months after the initial thermal ablation.