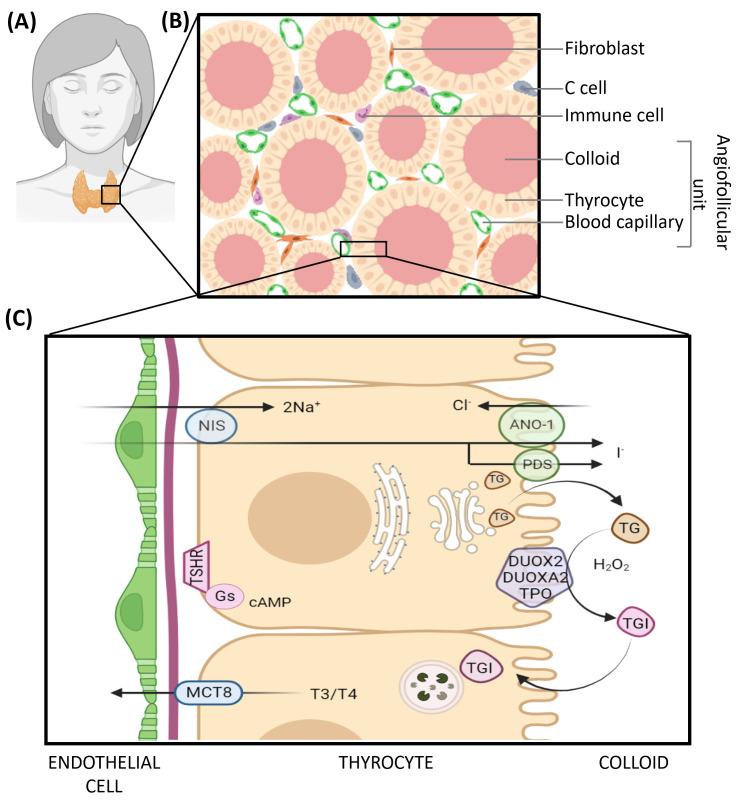
Figure 1.
Histology and function of the healthy thyroid gland. (A) Anatomical localization of the gland. (B) Schematic representation of the thyroid parenchyma. (C) Oversimplified representation of thyroid hormone synthesis with major actors. The synthesis of thyroid hormones, namely thyroxine or tetra-iodothyronine (T4) and tri-iodothyronine (T3), begins in thyrocytes with the expression of thyroglobulin (TG). TG is glycosylated in the Golgi and secreted by exocytosis in the follicular lumen. Concomitantly, thyrocytes captures iodide (I−) from the bloodstream via the sodium/iodine symporter (NIS) located at their basolateral pole. Cytoplasmic iodide is then transferred across the apical membrane into the lumen via Anoctamin-1 (ANO-1) and Pendrin (PDS). Within the lumen, iodide is oxidized to di-iodine (I2) and serves as a substrate for thyroglobulin iodination on tyrosine residues. TPO catalyzes the covalent binding of mono-iodide or di-iodide to tyrosine residues of thyroglobulin (MIT or DIT) and different coupling reactions between modified residues thereby generating iodinated thyroglobulin (TGI). Those reactions require the presence of H202 generated by DUOX2 and DUOXA2 proteins. Upon TSH binding to its receptor at the basal membrane, colloid droplets are endocytosed (among other events), and endosomes fuse with lysosomes. TGI is hydrolyzed by lysosomal proteases, and the released T3/T4 hormones are transported in the cytoplasm. They are finally exported from the thyrocyte to the extracellular milieu via the monocarboxylate transporter MCT8; they cross the basal lamina and reach the blood flow through the fenestrated capillaries.