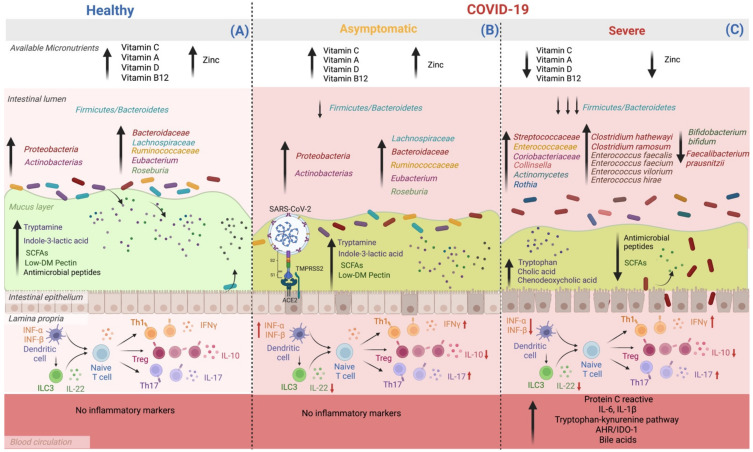
Figure 2.
Micronutrient availability, gut microbiota, and its derived metabolites modifications according to COVID-19 severity. Patients with severe complications from COVID-19 have lower availability of micronutrients such as vitamin C, A, D, B12, and Zn compared to asymptomatic and healthy subjects. On the other hand, the dysbiosis of GM seems to worsen as the complications of the disease progress. (A) Healthy subjects have an adequate balance in the Firmicutes: Bacteroidetes ratio, as well as an abundance of beneficial species belonging to the Proteobacteria and Actinobacteria phyla, such as Lachnospiraceae, Bacteroidaceae, Ruminococcaceae, Eubacterium, and Roseburia. Therefore, there is an adequate production of metabolites from the processing of host nutrients: SCFAs, secondary BA, tryptamine, and indole-3-lactic acid. Additionally, some molecules that regulate immune cell function are present, including the balance between Th cell subtypes and their role in controlling a tolerogenic environment and the intestinal barrier. (B) In asymptomatic people with COVID-19, no micronutrient deficiency is observed; in addition, although there is an alteration in the GM when compared to uninfected individuals, it is not as marked; the Firmicutes–Bacteroidetes ratio decreases, mainly affecting immunological regulation since there is a decrease in the production of IL-22 and IL-10. Also, an increase in IFNγ IL-17, the latter cytokines are necessary for the antiviral response. (C) In patients with severe COVID-19, there is a deficiency of vitamins C, A, D, B12, and Zn. In addition, the ratio of Firmicutes–Bacteroidetes decreases significantly, the abundance of pathogenic bacteria increases, and those beneficial in pathways decrease nutrient metabolism, which reduces beneficial host metabolites synthesis, such as SCFAs and tryptophan-derived metabolites synthesized by bacteria, such as tryptamine and indole-3-lactic acid. This set of events, together with the intrinsic failure of intestinal transit, also causes the accumulation of primary BA in the colon and an increase in the circulation of primary and secondary BA. Therefore, it increases the damage to the intestinal barrier and bacterial translocation, which leads to a proinflammatory environment with high serum levels of C-reactive protein, IL-6 and IL-1β, proinflammatory cytokines that promote the continuous activation of AHR-IDO-1 and reduces the antiviral response of INF type 1 (α and β) (created by BioRender.com).