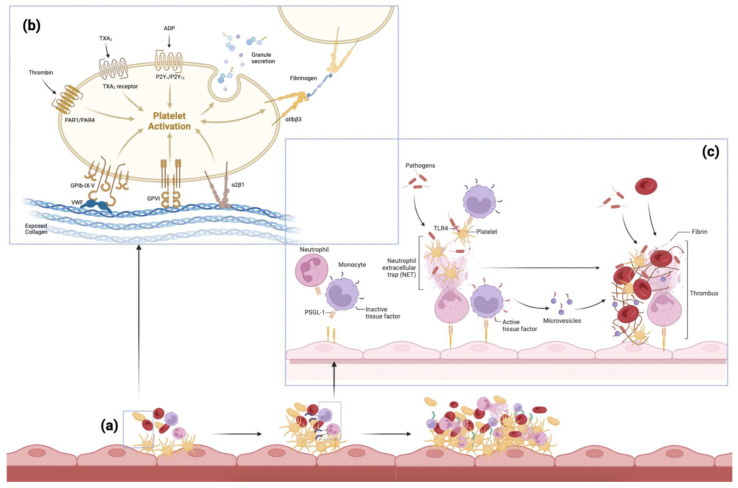
Figure 2.
The pathogenesis of thromboembolism. Various pathways implicated in the pathogenesis of thromboembolism: (a) The accumulation of thrombotic mediators and cells, starting with primary hemostasis including platelet activation and immuno-thrombosis, followed by secondary hemostasis forming a thrombus. (b) The process of platelet activation: exposed connective tissue and collagen cause platelets to change shape and adhere to the vessel wall via pseudopods and platelet receptors. Activated platelets release factors from their granules such as adenosine diphosphate (ADP) (causing nearby platelets to adhere, creating a platelet plug), thromboxane A2 (TXA2) (promoting platelet aggregation and release of more ADP), and thrombin (a strong platelet agonist converting fibrinogen to fibrin). The von Willebrand Factor (VWF) helps platelets adhere via platelet receptor Glycoprotein Ib (GP Ib) on the platelet membrane [28]. (c) Neutrophils release neutrophil extracellular traps (NETs), which further promote thrombus formation and help platelet activation. Monocytes express tissue factors on their surface, and aid red blood cell (RBC) recruitment and fibrin formation [29]. Adapted from Engelmann and Massberg (2013) and Bi et al. (2021) [29,31]. Abbreviations: TXA2: thromboxane A2; ADP: adenosine diphosphate; PAR: protease-activated receptor; GP: glycoprotein; VWF: von Willebrand factor; NET: neutrophil extracellular trap; RBC: red blood cell; TLR: toll-like receptor; PSGL-1: P-selectin glycoprotein ligand-1.