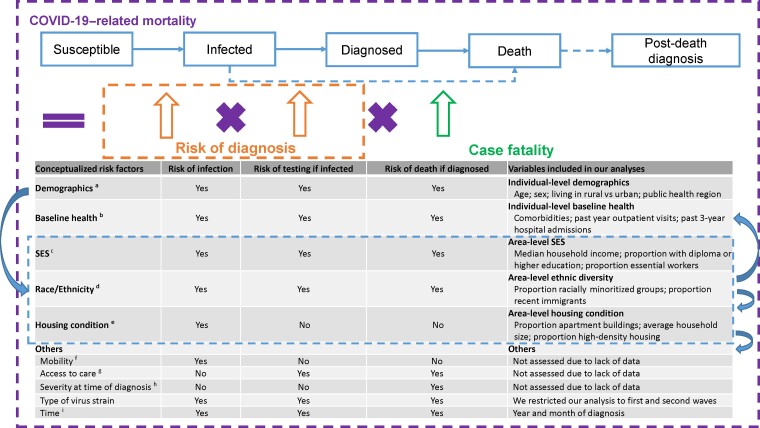
Figure 1.
Conceptualization of risk factors for COVID-19–related mortality. Based on the conceptualized factors, we sourced data, where available, at the individual level, otherwise at the area level. aAreas where an individual resides might reflect contact rates in communities and healthcare system capacity and quality and therefore associated with risk of infection, testing, and death [1, 2, 12]. bIndividual's baseline health (eg, comorbidities) has been correlated with susceptibility to COVID-19 infection and severity of infection and therefore associated with risk of infection, testing, and death [4]. cOccupation (eg, essential workers) might reflect contact rates at work and therefore be associated with risk of infection and testing [12, 29]. Income and education might affect exposure to the virus through working or living conditions, while also reflecting access to healthcare services, and therefore be associated with risk of infection, testing, and death [12, 30]. dRacially minoritized groups might be subject to systemic racism and socioeconomic inequalities, affecting the risk pathway of COVID-19–related mortality [3, 8]. eHousing conditions might reflect contact rates within household and be associated with risk of infection [12, 28, 31]. fWe assume mobility is a mediator for the relationship between social determinants of health (SDOH) and risk of infection. gWe assume access to care is a mediator for the relationship between SDOH and risk of testing and death. hWe assume severity at time of diagnosis is a mediator for the relationship between SDOH and risk of death. iA change occurred in August 2020 regarding clinical practice with respect to the use of steroids to treat COVID-19. Abbreviations: COVID-19, coronavirus disease 2019; SES, socioeconomic status; SDOH, Social determinants of health.