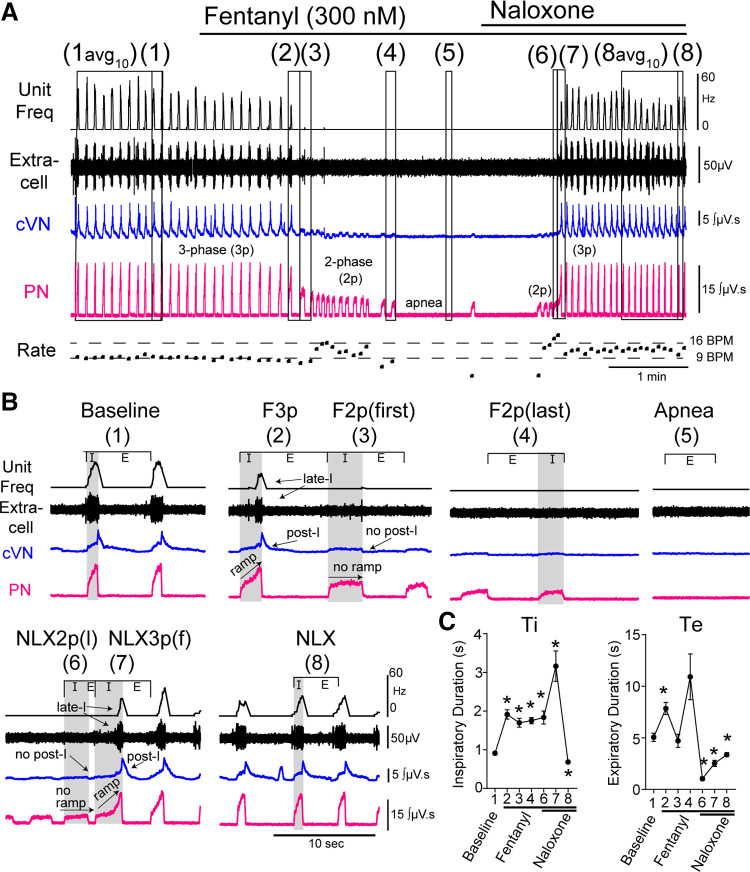
Figure 1.
Respiratory motor output during fentanyl and naloxone (NLX) administration. Recordings from central vagus nerve (cVN), phrenic nerve (PN), and the dorsolateral pons were made using an in situ preparation of rat. A: continuous recording of (top to bottom) integrated instantaneous frequency of single dorsolateral pontine unit spiking activity (black, Unit Freq), raw signal from dorsolateral pontine extracellular recording (black, Extracell), integrated cVN activity (blue), and integrated PN activity (pink). Instantaneous respiratory rate [fictive breaths per minute (BPM)]) is shown below. Systemic application of fentanyl (300 nM) results in slowing of normal three-phase output, transition to low-amplitude, two-phase bursts, which then slowed resulting in sustained apnea. Systemic application of naloxone (1 μM) restores output in a similar but reversed manner to fentanyl-mediated decline. B: zoomed in view of epochs indicated in A. Avg10 is average of 10 breaths. Epochs are as follows: (1) baseline, (2) last three-phase breath in fentanyl (F3p), (3) first two-phase breath in fentanyl (F2p(f)), (4) last two-phase breath in fentanyl (F2p(l)), (5) Apnea, (6) last two-phase breath in naloxone (NLX2p(l)), (7) first three-phase breath in naloxone (NLX3p(f)), and (8) recovery after naloxone (NLX). C: inspiratory duration (Ti) and expiratory duration (Te) during each epoch. Symbols are group means ± SE, n = 47 rats. *P < 0.0001, compared with baseline by repeated-measures two-way ANOVA and Tukey’s post hoc test.