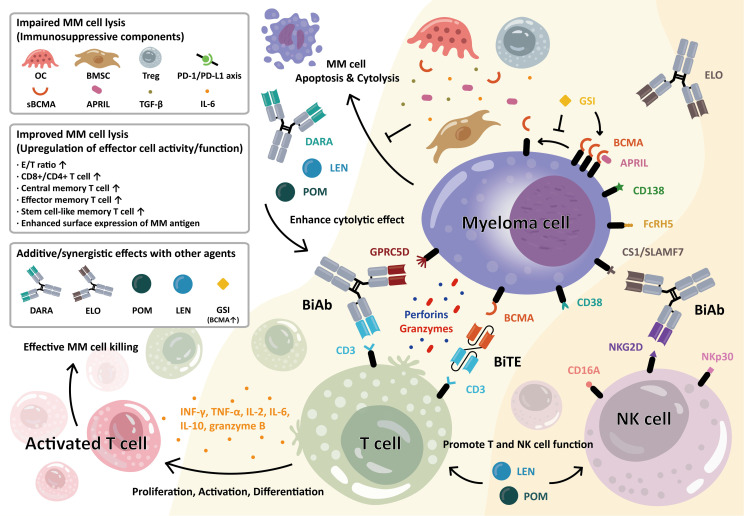
Figure 1.
Anti-myeloma activity of bispecific antibody (BiAb) and bispecific T-cell engager (BiTE) molecules in the bone marrow MM microenvironment. T-cell–redirecting BiAb and BiTE simultaneously bind to the myeloma-specific antigens on MM cells and CD3 on T cells. MM antigens include BCMA, CD38, CS1/SLAMF7, GPRC5D, and FcRH5, as indicated. Upon engagement, the immune synapse is formed, followed by the production and secretion of cytolytic molecules, i.e., perforin and granzymes, from T cells, resulting in MM cell lysis. This further induces T-cell activation, proliferation, and differentiation into various memory subsets. The BiAb/BiTE-mediated T-cell activation leads to increased levels of granzyme B, IFN-γ, IL2, IL6, IL8, IL10, and TNF-α. The BiAb/BiTE-mediated MM cell killing is negatively affected by cellular and molecular factors including bone marrow stromal cells (BMSC), osteoclast (OC), regulatory T cells (Treg), a proliferation-inducing ligand (APRIL), transforming growth factor-β (TGF-β), interleukin-6 (IL-6), soluble BCMA (sBCMA), and upregulation in PD-L1/PD1 axis. Conversely, upregulation in effector/target (E/T) ratio, CD8+ T cell, and differentiated T cells with central and stem-like memory subsets are associated with improved BiAb/BiTE-mediated MM cell lysis. Furthermore, the potency and durability of their ability to kill MM cells could be enhanced when combined with current standard-of-care therapies including daratumumab (DARA), elotuzumab (ELO), lenalidomide (LEN), or pomalidomide (POM). Moreover, soluble BCMA (sBCMA), constantly shed by gamma-secretase (GS), could antagonize optimal MM cell eradication by BCMA-targeting agents. The GS inhibitor (GSI) rapidly blocks the release of sBCMA and augments BCMA protein retention on the MM cell membrane, thereby MM cell targeting and killing are significantly improved. In a similar manner, the BiAbs or natural killer cell engagers (NKCEs) also target natural killer (NK) cell-related receptor antigens (i.e., CD16A, NKG2D, NKp30) to activate NK cells and augment their anti-MM activities. For example, the anti-CS1 Ab elotuzumab (ELO) enhances NK cell function via CS1 and NKG2D to kill MM cells. (Some elements of Figure 1 are created with BioRender.com).