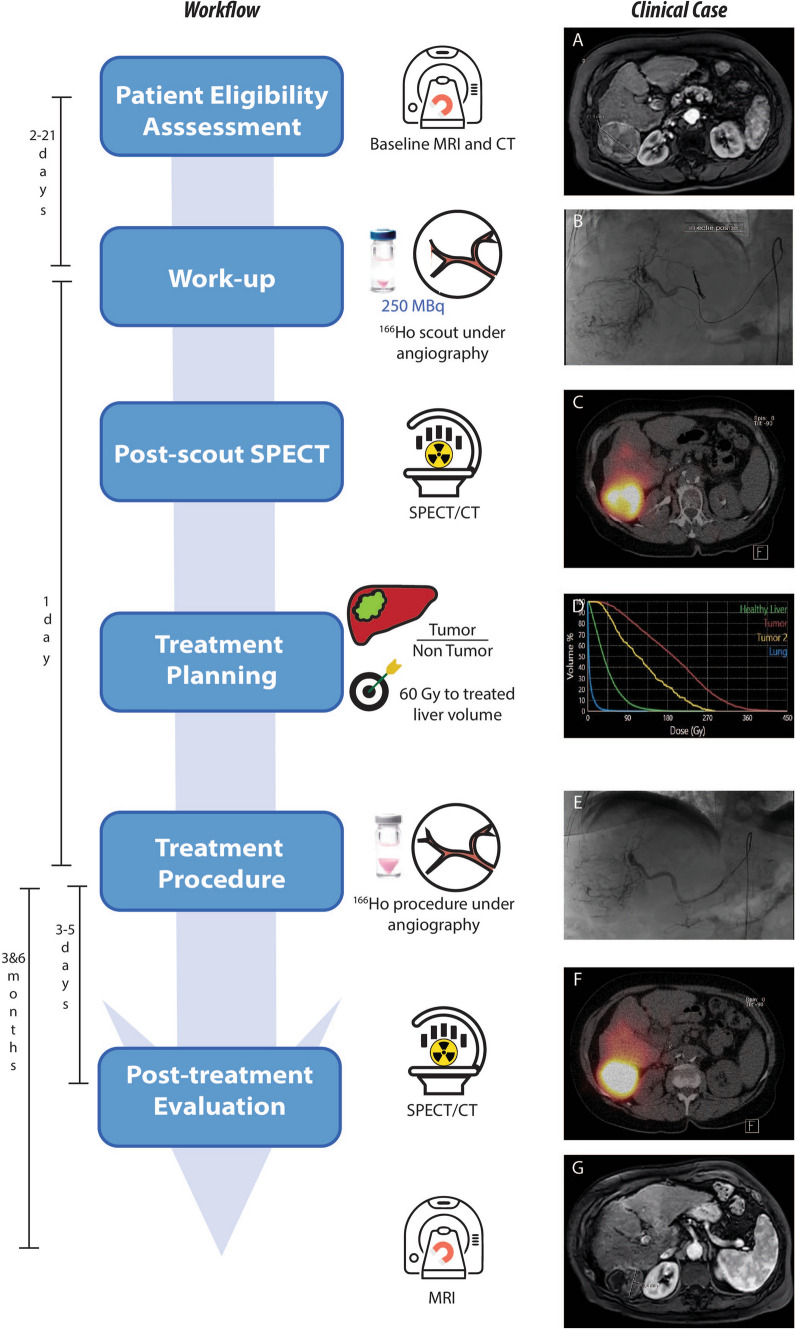
Fig. 1.
On the left, the steps of the clinical workflow for 166Ho liver radioembolization are depicted. On the right, images referring to an exemplary clinical case are reported. A 73 years old female patient diagnosed with hepatocellular carcinoma was referred for 166Ho radioembolization. Among others, she presented a lesion in segment 6 with a maximum diameter of 71 mm, as it is possible to see from the baseline MRI reported in panel A. During the workup angiography (panel B), coil embolization of the segment 4 artery was performed to obtain intrahepatic redistribution. Consequently, activity initially planned for segment 4 was added to the activity injected in the right hepatic artery, for a total of 122 MBq. In the SPECT/CT acquired after the scout procedure and displayed in panel C, it is possible to see a clear 166Ho uptake in the segment 6, where the tumor lesion was located. No extrahepatic deposition was reported, confirming a successful scout procedure. After having planned the treatment aiming at 60 Gy average absorbed dose to the whole liver (panel D), 4116 166Ho MBq was injected into the right hepatic artery (panel E). 3 days after the treatment, a SPECT/CT was acquired to visually confirm the good targeting of tumor in segment 6 (panel F). Post-treatment dosimetry revealed a good targeting of the tumor, which received a mean dose of 137 Gy, and a safe uptake by the healthy liver, which had a mean absorbed dose of 36 Gy. The MRI acquired 3 months after the treatment (panel G) showed a decrease in lesion size of segment 6 from 71 to 42 mm and complete disappearance of contrast enhancement (complete response according to mRECIST)